Abstract
Keywords
Misoprostol Transcervical Catheter Syntocinon (Oxytocin) Bishop Score Induction of Labor
1. Background
In many cases, pregnant women need pregnancy termination due to different causes (1). Over the past 20 years, studies have shown a high increase in the rate of induced labor from 9.5% in 1990 to 21.2% in 2004 (2). Reports have shown that increased labor duration could raise the risk of cesarean section in pregnant women (3). If oxytocin is prescribed before cervical preparation, it may increase the success rate of induction (4) and prevent prolonged induction and delivery problems that have adverse psychological and physical effects on the pregnant women and affects the individual’s sense of satisfaction with natural delivery (5). The appropriate cervix is clinically relevant to the degree of softness, effacement, and dilatation of the cervix (6). Several methods have been proposed for the ripening of the cervix before labor induction, which are mainly classified in the two groups of mechanical and pharmacological (7). The ideal method should not be associated with adverse maternal and fetal side effects during cervical preparation (8). The mechanical techniques include a transcervical catheter with or without extra-amniotic saline infusion (EASI) to enhance endogenous prostaglandin secretion. These methods, which are performed by using a foreign body in the cervix, are the oldest methods introduced for labor induction and are still widely used (9). Due to the improvement of pharmaceutical methods and transcervical catheters with or without EASI, these methods can efficiently cause cervical dilatation and ripening. However, minor complications are unusual and include pain, bleeding, acute amniotomy, and febrile morbidity (10, 11). The results of two systematic studies showed that mechanical techniques due to less maternal and fetal complications in comparison with pharmacological methods, especially prostaglandins, are more effective and safe (12, 13).
The use of drugs such as mifepristone, misoprostol, and oxytocin for pregnancy termination is effective and safe. Misoprostol is an analogue of prostaglandin that is used in over 60 countries for the treatment and prevention of gastric ulcers caused by long-term use of non-steroidal anti-inflammatory drugs. Misoprostol is mostly used to induce labor in the second trimester for cervical ripening before curettage, hysteroscopy, endometrial biopsy, preterm delivery termination, missed abortion, postpartum hemorrhage, and induction of term delivery (14). Oxytocin is one of the most common and well-known hormones used to induce labor.
Oxytocin directly affects the contractions of the uterus. A significant increase in the number of oxytocin receptors up to 300 times has been reported with pregnancy progression (15). Oxytocin hormone is produced by the hypothalamus and its storage location is in the posterior pituitary gland. Oxytocin is released from the posterior pituitary gland during labor and affects the myometrial smooth muscle of the uterus. Oxytocin also affects the breasts (8). By releasing oxytocin at the initiation of labor, it directly affects the uterus’ function and increases contractions of the uterus in terms of frequency and strength. Signals that increase the concentration of calcium inside the muscle cells lead to the contraction of the uterus due to the effect of oxytocin on the G-protein receptors (8). In the past several decades, synthetic oxytocin versions have been used for labor induction. Studies have shown that the induction of labor by the use of oxytocin has the best results. It has been reported that the use of oxytocin is more beneficial for cervical ripening, compared with expectant management (16).
Since in many cases, during the termination of pregnancy, the cervix is inappropriate and induction of labour in these conditions leads to prolonged delivery and maternal fatigue, the use of cervical preparation methods is recommended.
2. Objectives
The aim of this study was to compare the effects of the three methods of syntocinon, misoprostol, transcervical catheter with syntocinon on the success of labor induction.
3. Methods
The present study was conducted among 120 primigravida women with a Bishop score of < 5 who were candidates for labor induction in Ali Ibn Abi Talib and Khatam hospitals of Zahedan in 2014.
The inclusion criteria included primigravida women with Bishop score less than 5 and vertex presentation who were candidates for labor induction. The exclusion criteria comprised of premature preterm rupture of membranous (PPROM), preterm rupture of membranous (PROM), uterine scars, Bishop score of more than 5, history of Cesarian Section, and contraindications for natural vaginal delivery. Therefore, women who were willing to participate in the study were chosen using the convenience sampling method. After obtaining informed consent, using the block randomization method, they were assigned to the three groups of receiving syntocinon (4 miliunit per minute), misoprostol (25 micrograms), or transcervical catheter with syntocinon (4 miliunit per minutes).
After admission to the maternity room, demographic characteristics (i.e., age, body mass index, and gestational age) and maternal vital signs (i.e., blood pressure, pulse rate, respiratory rate, and temperature) were recorded. Then, a vaginal examination was performed, and the Bishop score was determined. Afterward, the women were randomly assigned to the syntocinon, misoprostol, or transcervical catheter with syntocinon groups.
The interval between the initiation of labor induction and the active phase of labor and the interval between the onset of labor induction and delivery (by digital vaginal examination and determination of dilatation of the cervix in cm every two hours), as well as unwanted side effects such as infection, fever, bleeding ,vomiting, diarrhoea and chills up to one week later, were compared among the three groups.
Data analysis was performed by SPSS version 18. For qualitative variables, frequency and distribution rate were reported, and for the quantitative variables, mean and standard deviation were calculated. We used the chi-square test to compare treatment outcomes and the complications, and ANOVA was used to compare the timing of induction and the interval between initiation induction and delivery. If the results were significant.
4. Results
Overall 120 (40 per group) women were included in this study. The subjects were similar in terms of variables such as age, dilatation of the cervix, and mean time interval in the three groups (Table 1).
Distribution of Age, Cervix Dilatation and Time Interval Among Three Studied Groups (P > 0.05)a
| Groups Variable | Age | Dilatation | Time Interval |
|---|---|---|---|
| Syntocinon | 26.77 ± 5.4 | 2.78 ± 0.8 | 359.25 ± 55.9 |
| Misoprostol | 26.88 ± 5.1 | 3.10 ± 0.7 | 362.75 ± 60.0 |
| Transcervical catheter with syntocinon | 25.80 ± 5.3 | 3.0 ± 0.8 | 365.50 ± 60.3 |
Frequency distribution of the characteristics such as body mass index (BMI), family history, success ates and medication side effects were also determined in the three groups (Table 2).
The Distribution of Dependent Variables (Including BMI, Family History and Success Rate in Each Group and Side Effect of the Medications) in the Three Groups According to the Chi-Square Testa
| Groups | Variables | P Value | ||
|---|---|---|---|---|
| Syntocinon | Misoprostol | Transcervical Catheter with Syntocinon | ||
| Family history | > 0.05 | |||
| Yes | 8 (20) | 9 (22.5) | 7 (17.5) | |
| No | 32 (80) | 31 (77.5) | 33 (82.5) | |
| Success | > 0.05 | |||
| Yes | 29 (72.5) | 26 (65) | 31 (77.5) | |
| No | 11 (27.5) | 14 (35) | 9 (22.5) | |
| BMI | > 0.05 | |||
| Thin | 6 (15) | 2 (5) | 2 (5) | |
| NL | 25 (62.5) | 19 (47.5) | 25 (62.5) | |
| Owerwaight | 5 (12.5) | 17 (42.5) | 12 (30) | |
| Obese | 4 (10) | 2 (5) | 1 (2.5) | |
| Side effects of medications | > 0.05 | |||
| Yes | 3 (7.5) | 1 (2.5) | 3 (7.5) | |
| No | 37 (92.5) | 39 (97.5) | 37 (92.5) | |
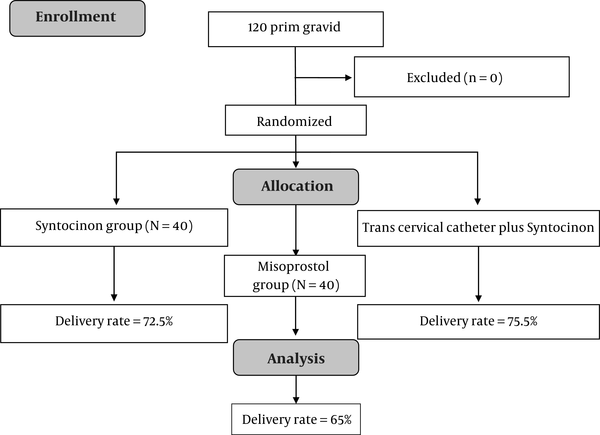
The rates of normal vaginal delivery in the syntocinon, transcervical catheter plus syntocinon, and misoprostol groups were 72.5%, 77.5%, and 65%, respectively, which did not show a significant difference between the three groups based on the chi-square test (Figure 1).
Flowchart of pregnancy chart between the three groups (syntocinon, misprostol, and transcervical plus synctocinon)
Side effects of medications in the syntocinon, syntocinon group plus transcervical catheter, and misoprostol groups were 7.5%, 7.5%, and 2.5%, respectively, which did not show a significant difference between the three groups based on the chi-square test.
5. Discussion
Different reasons such as fetal death, pregnancy-related hypertension, fetal abnormalities in the second trimester, and PROM necessitate the termination of pregnancy. In the health centers of some countries, cervical ripening and induction of labor are performed by oxytocin alone or with a catheter, which increases the duration of delivery and costs. The use of prostaglandins in other countries is common because they have low adverse effects and more success.
The success rate (NVD) in the syntocinon group was 72.5%, in the syntocinon group plus transcervical catheter 77.5%, and in the misoprostol group 65%, which did not show a statistically significant difference between the three groups based on the chi-square test (P > 0.05). Totally, 10 patients underwent a cesarian section that were excluded from the study. The incidence of medication side effects in the syntocinon group was 7.5%, in the syntocinon plus catheter group 7.5%, and in the misoprostol group 2.5%, which did not show a significant difference between the three groups based on the chi-square test (P > 0.05).
The results of this study showed that any of the three methods (syntocinon, misoprostol and transcervical catheter with syntocinon) could be used for labor induction in primigravida women with low Bishop scores. These methods will improve the Bishop score and prepare the cervix in a shorter duration, which will reduce the duration of delivery.
The study of Cromi et al. (17) was performed among 210 women with a gestational age of 34 weeks or more and a Bishop score of less than 6 in two groups with cervix preparation by mechanical and pharmacological methods. The results showed that using the catheter is accompanied by a higher percentage of normal delivery for 24 hours (68.8% vs. 49.5%). In addition, the need for oxytocin was higher in the catheter group (85.7% vs. 54.4%). There was no significant difference in terms of improvement of Bishop score, cesarean rate, and maternal and fetal complications in the two groups (17).
The results of a study by Sciscione et al. (18) on pregnant women with a Bishop score of less than 6 showed no significant difference in this regard in the two groups of transvaginal catheters and misoprostol tablets. Also, there was no significant difference between the groups in terms of duration of delivery, delivery method, and fetal complications, but the incidence rates of uterine contractions (uterine tachysystole) and meconium excretion were significantly higher in the misoprostol group (18).
Fox et al. (19) showed that in pregnant women who used vaginal misoprostol or catheter, there was no significant difference in the mean duration vaginal delivery, cesarean section, or incidence of chorioamnionitis, but in the group receiving misoprostol, the incidence of uterine tachysystole was higher.
In a study performed by Pettker et al. (20) in the United States in 2008, two methods were used for labor induction. Transvaginal catheters were used for 92 women, and 91 patients only received oxytocin. The results of their study showed that the interval between the onset labor induction and the entrance to the active phase of labor, the interval between the onset labor induction and the time of delivery, and the side effects of medications in the two groups were similar. The results of that study were consistent with the results obtained in our study (20).
In a study by Cromi et al. (21) conducted in Italy in 2007, the transvaginal catheters method was assessed. Their results showed no complications in women who were induced using a transvaginal catheters. They reported that only 1.5% of the patients had infectious complications, and no fetal complications were observed. In our study, the frequency of complications in all three groups was relatively low, which indicates the safety of the methods under investigation (21). In another study on labor induction in Brazil in 2010, it was reported that success in the group that received misoprostol was significantly less than those receiving oxytocin and transvaginal catheters. However, the rates of uterine contractions and complications were similar in the two groups. The results of this study differed from our observations; the results of our study did not show any difference between the three groups (22). Pluchon (23) in 2014 reported the use of prostaglandin analogues, including gemeprost, dinoprostone, sulprostone, and misoprostol is one of the common methods to terminate the pregnancy. Their results showed that misoprostol has the least effects among the analogues, and its side effects are lower than those of other drugs in the same group. In addition, the dosage and method of using misoprostol, whether oral or vaginal, has no effects on the results (23). They reported that the best route of treatment for misoprostol is vaginal prescribing, which in our study also had a good effect. In a study conducted by Culver et al. (24) in 2004 on labor induction, it was reported that there was no difference between the group that received transvaginal catheters with oxytocin and the patients receiving misoprostol, which is consistent with our findings.
A study conducted in 2014 examined the efficacy of misoprostol for the induction of abortion in the first trimester of pregnancy. They reported that in sublingual and vaginal routes, misoprostol showed a significantly better efficacy than oral administration. In our study, there were no significant side effects for misoprostol (25). Mozurkewich et al. (26) used oral misoprostol to induce labor in PROM cases. They reported that there was no need for a cesarean section during the study.
A study by Clouqueur et al. (27) conducted in France in 2014 examined the various properties of misoprostol and its effectiveness during pregnancy. In this study, vaginal misoprostol was shown to be more effective than the oral method, and the onset of action is shorter. However, despite its benefits, its adverse effects did not differ from the oral method. They introduced misoprostol as an effective and safe method (27, 28), which is consistent with our findings. Our study showed that the three methods of syntocinon, misoprostol, and transcervical catheter with syntocinon could be used to terminate pregnancy in primigravida women with low Bishop scores, as they are low-risk and effective methods for cervical preparation. These methods can also promote the satisfaction of pregnant women by reducing the duration of labor.
Acknowledgements
References
-
1.
Zargar M, Nazari MA, Hormozy L, Madovi Mohammadi H. Efficacy of transcervical foley catheter and laminaria on induction of labor in post-term pregnancy: a clinical study. Tehran University Medical Journal TUMS Publications. 2014;72(3):161-6.
-
2.
Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al. Births: final data for 2006. Public Health Resources. 2009:65.
-
3.
Hemlin J, Möller B. Extraamniotic saline infusion is promising in preparing the cervix for induction of labor. Acta obstetricia et gynecologica Scandinavica. 1998;77(1):45-9. [PubMed ID: 9492717]. https://doi.org/10.1080/00016349808565810.
-
4.
Sherman DJ, Frenkel E, Tovbin J, Arieli S, Caspi E, Bukovsky I. Ripening of the unfavorable cervix with extraamniotic catheter balloon: clinical experience and review. Obstetrical & gynecological survey. 1996;51(10):621-7. [PubMed ID: 8888040]. https://doi.org/10.1097/00006254-199610000-00022.
-
5.
Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. American journal of obstetrics and gynecology. 2009;200(2):156. e1-4. https://doi.org/10.1016/j.ajog.2008.08.068.
-
6.
Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL. Preconceptional counseling. Williams Obstetrics. 23rd ed. New York, NY: McGraw-Hill. 2010.
-
7.
Adeniji OA, Oladokun A, Olayemi O, Adeniji OI, Odukogbe AA, Ogunbode O, et al. Pre-induction cervical ripening: transcervical foley catheter versus intravaginal misoprostol. Journal of obstetrics and gynaecology. 2005;25(2):134-9. [PubMed ID: 15814391]. https://doi.org/10.1080/01443610500040737.
-
8.
Gilstrop M, Sciscione A. Induction of labor-Pharmacology methods. Seminars in perinatology. Elsevier; 2015. p. 463-5.
-
9.
Sciscione AC. Methods of cervical ripening and labor induction: mechanical. Clinical obstetrics and gynecology. 2014;57(2):369-76. [PubMed ID: 24785420]. https://doi.org/10.1097/GRF.0000000000000023.
-
10.
Goldman JB, Wigton TR. A randomized comparison of extra-amniotic saline infusion and intracervical dinoprostone gel for cervical ripening. Obstetrics & Gynecology. 1999;93(2):271-4. https://doi.org/10.1097/00006250-199902000-00021.
-
11.
Siddiqui S, Zuberi NF, Zafar A, Qureshi RN. Increased risk of cervical canal infections with intracervical Foley catheter. Journal of College of Physicians and Surgeons Pakistan. 2003;13(3):146.
-
12.
Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BWJ, Irion O, Boulvain M. Mechanical methods for induction of labour. The Cochrane Library. 2012. https://doi.org/10.1002/14651858.CD001233.pub2.
-
13.
Boulvain M, Kelly A, Lohse C, Stan C, Irion O. Mechanical methods for induction of labour. Cochrane Database Syst Rev. 2001;4(4). https://doi.org/10.1002/14651858.CD001233.
-
14.
Allen R, O’Brien BM. Uses of misoprostol in obstetrics and gynecology. Reviews in obstetrics and gynecology. 2009;2(3):159.
-
15.
Kimura T, Takemura M, Nomura S, Nobunaga T, Kubota Y, Inoue T, et al. Expression of oxytocin receptor in human pregnant myometrium. Endocrinology. 1996;137(2):780-5. https://doi.org/10.1210/en.137.2.780.
-
16.
Alfirevic Z, Kelly AJ, Dowswell T. Intravenous oxytocin alone for cervical ripening and induction of labour. The Cochrane Library. 2009. [PubMed ID: 8593830]. https://doi.org/10.1002/14651858.CD003246.pub2.
-
17.
Cromi A, Ghezzi F, Uccella S, Agosti M, Serati M, Marchitelli G, et al. A randomized trial of preinduction cervical ripening: dinoprostone vaginal insert versus double-balloon catheter. American Journal of Obstetrics & Gynecology. 2012;207(2):125. e1-7. [PubMed ID: 22704766]. https://doi.org/10.1016/j.ajog.2012.05.020.
-
18.
Sciscione AC, Nguyen L, Manley J, Pollock M, Maas B, Colmorgen G. A randomized comparison of transcervical Foley catheter to intravaginal misoprostol for preinduction cervical ripening. Obstetrics & Gynecology. 2001;97(4):603-7. https://doi.org/10.1016/S0029-7844(00)01186-8.
-
19.
Fox NS, Saltzman DH, Roman AS, Klauser CK, Moshier E, Rebarber A. Intravaginal misoprostol versus Foley catheter for labour induction: a meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology. 2011;118(6):647-54. [PubMed ID: 21332637]. https://doi.org/10.1111/j.1471-0528.2011.02905.x.
-
20.
Pettker CM, Pocock SB, Smok DP, Lee SM, Devine PC. Transcervical Foley catheter with and without oxytocin for cervical ripening: a randomized controlled trial. Obstetrics & Gynecology. 2008;111(6):1320-6. [PubMed ID: 18515515]. https://doi.org/10.1097/AOG.0b013e31817615a0.
-
21.
Cromi A, Ghezzi F, Tomera S, Uccella S, Lischetti B, Bolis PF. Cervical ripening with the Foley catheter. International Journal of Gynecology & Obstetrics. 2007;97(2):105-9. [PubMed ID: 17316649]. https://doi.org/10.1016/j.ijgo.2006.10.014.
-
22.
Olimpio Filho BM, Albuquerque RM, Cecatti JG. A randomized controlled trial comparing vaginal misoprostol versus Foley catheter plus oxytocin for labor induction. Acta obstetricia et gynecologica Scandinavica. 2010;89(8):1045-52. [PubMed ID: 20636243]. https://doi.org/10.3109/00016349.2010.499447.
-
23.
Pluchon M, Winer N. Misoprostol in case of termination of pregnancy in the second and third trimesters. Trials. Journal de gynecologie, obstetrique et biologie de la reproduction. 2014;43(2):162-8. [PubMed ID: 24440001]. https://doi.org/10.1016/j.jgyn.2013.11.009.
-
24.
Culver J, Strauss RA, Brody S, Dorman K, Timlin S, McMahon MJ. A randomized trial comparing vaginal misoprostol versus Foley catheter with concurrent oxytocin for labor induction in nulliparous women. American journal of perinatology. 2004;21(3):139-46. [PubMed ID: 15085496]. https://doi.org/10.1055/s-2004-823777.
-
25.
Beucher G, Dolley P, Carles G, Salaun F, Asselin I, Dreyfus M. Misoprostol: off-label use in the first trimester of pregnancy (spontaneous abortion, and voluntary medical termination of pregnancy). Journal de gynecologie, obstetrique et biologie de la reproduction. 2014;43(2):123-45. [PubMed ID: 24433988]. https://doi.org/10.1016/j.jgyn.2013.11.007.
-
26.
Mozurkewich E, Horrocks J, Daley S, Von Oeyen P, Halvorson M, Johnson M, et al. The MisoPROM study: a multicenter randomized comparison of oral misoprostol and oxytocin for premature rupture of membranes at term. American Journal of Obstetrics & Gynecology. 2003;189(4):1026-30. https://doi.org/10.1067/S0002-9378(03)00845-7.
-
27.
Clouqueur E, Coulon C, Vaast P, Chauvet A, Deruelle P, Subtil D, et al. Use of misoprostol for induction of labor in case of fetal death or termination of pregnancy during second or third trimester of pregnancy: efficiency, dosage, route of administration, side effects, use in case of uterine scar. Journal de gynecologie, obstetrique et biologie de la reproduction. 2014;43(2):146-61. [PubMed ID: 24461423]. https://doi.org/10.1016/j.jgyn.2013.11.008.
-
28.
Teimoori B, Esmaeilpoor M, Khaefi Ashkezari A, Farzaneh F. Comparison of Induction Abortion in the First Trimester Using Misoprostol Alone and Misoprostol With Estrogen Priming. International Journal of Women's Health and Reproduction Sciences. 2019;7(3):404-7. https://doi.org/10.15296/ijwhr.2019.66.
