Abstract
Background:
Staphylococcus aureus is one of the main agents of nosocomial infections. Identifying coagulase enzyme in staphylococcal infections is of great importance as it is one of the main virulence agents. The present study aims to accurately detect the presence of coagulase gene and its relationship with antibiotic resistance patterns in clinical isolates.Methods:
In this experimental study, a total of 20 clinical samples of S. aureus and 10 clinical samples of coagulase-negative staphylococci were collected and identified from hospitals and laboratories in Nowshahr and Chalous. Antibiotic resistance patterns of isolates were examined based on CLSI and finally polymerase chain reaction was used in order to detect the presence of coagulase gene with specific primers. Treatments were examined in three intervals and the results were analyzed using one-way analysis of variance (ANOVA), univariate ANOVA, and t-test at the probability level of P < 0.05. Moreover, the comparison of means was presented using Duncan’s multiple range tests (P < 0.05). All the statistical analyses were carried out using SPSS (V. 16).Results:
Suggested that isolates showed phenotypic presence of coagulase enzyme and had this gene genotypically as well. Coagulase-positive samples demonstrated higher resistance to tetracycline 20%, oxacillin 55%, gentamicin 20%, and kanamycin 25%. Statistically, there was no significant difference among inhibition zone diameters of oxacillin, nalidixic acid, gentamicin, kanamycin, and penicillin.Conclusions:
Coagulase gene causes antibiotic resistance and coagulase-negative staphylococci are spreading rapidly and their resistance is increasing.Keywords
Coagulase Drug Resistance Microbial PCR Staphylococcus aureus
1. Background
Staphylococcus aureus is a Gram-positive, facultative anaerobic non-spore-forming, catalase-positive bacterium [1]. Staphylococci, especially Staphylococcus epidermidis, are part of the normal flora of human skin, and gastrointestinal and respiratory tracts. S. aureus is the most significant pathogen of human infections, mainly wound, respiratory tract and skin infections that is associated with several pathological processes such as food poisoning, pneumonia, bacteremia, folliculitis, and osteomyelitis [2-4]. This organism is one of the most important causes of nosocomial infections, which become increasingly more resistant against the antibiotics of beta-lactam and vancomycin groups [5, 6]. Coagulase is an enzyme produced by S. aureus that causes clotting of blood in the human host. S. aureus secretes two forms of coagulase enzyme, bound coagulase and free coagulase [7, 8]. Free coagulase binds with coagulase-reacting factor (CRF) in plasma and creates a complex, staphylothrombin [9-11]. Dawnson et al. Conducted a descriptive study in China on specific molecular and epidemiological characteristics of S. aureus in patients in Xinyang, China [12]. The Coa gene, coding for the coagulase enzyme, can be used for DNA-based diagnosis of S. aureus. The coa gene is highly polymorphic because of differences in the sequence of the 30 variable region. Analysis of the Coa gene in a variety of staphylococcal species has shown diversity in the amino acid sequence and the number of tandem repeats at the 30 end. There is heterogeneity in this domain, including the number of 81-bp tandem short sequence repeats encoding repeated 27 amino acid sequences in the C-terminal region. Detecting the coagulase enzyme in staphylococci infections is important because it is considered as one of the pathogenic factors of this bacterium [13, 14]. Studies on molecular diagnosis of genes encoding coagulase of S. aureus using different techniques such as PCR and RFLP can be conducted. PCR, based on molecular methods, is often preferred to diagnose antibiotic resistant genes. Rapid and reliable methods for antibiotic susceptibility are important to institute appropriate therapy [13-15]. Accordingly, the present study aims to determine the antibiotic resistance patterns and their relationship with presence of coagulase gene in clinical isolated of S. aureus collected from hospitals of Nowshahr and Chalous.
2. Methods
2.1. Sample Collection
In the current study, that is experimental study, 30 isolates of staphylococci, including 6 samples of S. epidermidis, 4 samples of S. saprophyticus, and 20 samples of S. aureus, which were obtained from hospital clinical samples (pharynx, nose, urine, trachea, lung, vagina, joint fluid, and lesion) of hospitals in Nowshahr and Chalous, between March 2015 to august 2015. It should also noteworthy that ethical issues regarding collecting the samples above were thoroughly regarded in that the researchers were permitted to gather the required samples. All the samples were cultured and purified in blood agar media.
2.2. Species Identification
Using microbial standard methods including, catalase, coagulase (tube and slide), mannitol fermentation on mannitol salt agar, brad parker agar, DNase agar, the isolated S. aureus was confirm. Also for detecting coagulase-negative staphylococci (epidermidis and saprophyticus) from micrococcus Bacitracin test was used. In order to distinguish S. epidermidis and S. saprophyticus, Novobiocin resistance test was used. Isolates were stored at -80°C in Nutrient Broth (Merk-Germany) supplemented with 30 percent Glycerol
2.3. Susceptibility Testing
The sensivity of isolates (S. aureus, S. epidermidis, S. saprophyticus, and micrococcus) was examined by disk diffusion method based on CLSI guide direction, including: penicillin, oxacillin, gentamicin, chloramphenicol, vancomycin, kanamycin, and nalidixic acid.
2.4. DNA Extraction
To extract nucleic acid from bacteria, the boiling method proposed in a study by Hosseinpour et al. was used [11]. DNA-containing micro-tubes were kept at -20°C.
2.5. PCR Technique
Isolates were tested for the presence of coa gene using two sequence of primers as described by Hookey et al. [16]. Including the Forward primers (5-ATA-GAG-ATG-CTG-GTA-CAG-G-3) and Reverse (5- GCT-TCC-GAT-TGT-TCG-ATG-C-3). Each of extracted 50-microliter tube of PCR reaction contained 2.5 microliter nucleic acid, a master mix of 3.2 µL, forward primer of 0/8 µL, reverse primer of 0/8 µL, and 12.7 µL of distilled water. Reaction was performed in the thermo cycler ( Eppendorf- Germany) by denaturation at 95°C for 5 minutes, followed by 40 cycles of 95°C for 30 seconds, 55°C for 1 minute and 72°C for 1 minute. Final extension was 7 minutes at 72°C in the end of cycle. The products of the PCR were analyzed by electrophoresis in a 2% agarose gel.
Treatments were examined in three intervals and the results were analyzed using one-way analysis of variance (ANOVA), univariate ANOVA, and t-test at the probability level of P < 0.05. Moreover, the comparison of means was presented using Duncan’s multiple range test (P < 0.05). All the statistical analyses were carried out using SPSS (V. 16) and graphs were drawn using Microsoft Excel 2007.
3. Results
3.1. Antibiotic Resistance in Isolates of S. aureus, S. Epidermidis, and S. Saprophyticus
Table 1 shows that coagulase-positive strains are more resistant to antibiotics compared with coagulase-negative strains.
| Antibiotics | ||||||||
|---|---|---|---|---|---|---|---|---|
| Gene | K | V | PG | NA | GM | OX | C | TE |
| CoA+ | 25 | 0 | 100 | 55 | 20 | 55 | 0 | 20 |
| CoA- | 0 | 0 | 100 | 50 | 10 | 10 | 0 | 10 |
Coagulase-negative strains show 10% resistance to nalidixic acid, oxacillin, and tetracycline, they were sensitive to kanamycin, vancomycin, and chloramphenicol.
The results reveal that coagulase-positive staphylococci samples were 100% sensitive or semi-sensitive to chloramphenicol, 100% sensitive to vancomycin, 45% sensitive to oxacillin, 80% sensitive to tetracycline, 75% sensitive to kanamycin, 45% sensitive to nalidixic acid, and 80% sensitive to gentamicin. All of the isolates were resistant to penicillin.
Also, the results show that coagulase-negative staphylococci were 90% sensitive or semi-sensitive to gentamicin, and 100% sensitive or semi-sensitive to kanamycin and vancomycin. All of the isolates were resistant to penicillin, and 90% sensitive to oxacillin.
3.2. Polymerase Chain Reaction (PCR) for Coagulase Gene in S. aureus Samples
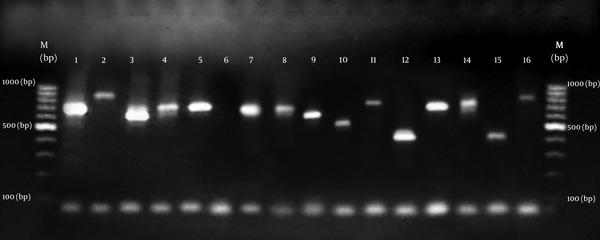
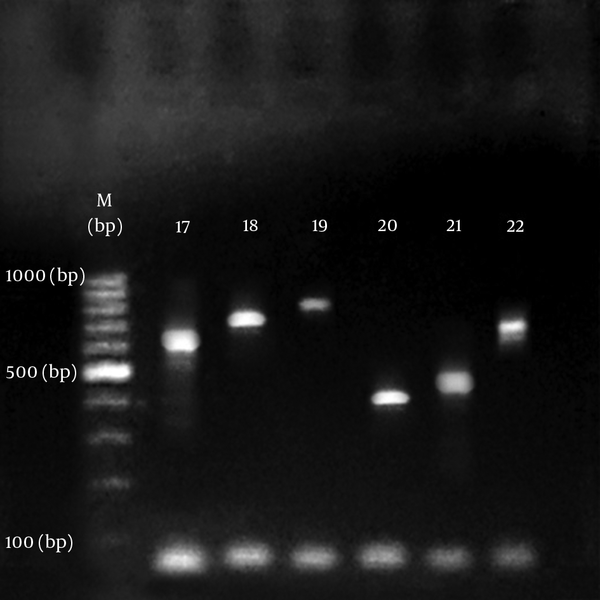
All isolates of S. aureus produced PCR amplicon with the coa primers. The agarose gel analysis of the digestion products showed 15 diferent sizes ranging from approximately 400 to 900 bp. As summarized in Figures 1 and 2. There was no amplification on product of DNA from s. epidermidis and s. saprophyticus. Results show that S. aureus samples in biochemical tests contained coagulase enzyme as well as containing it in PCR test (Table 2).
Agarose Gel Electrophoresis of Coagulase (coa) Gene PCR Products
Agarose Gel Electrophoresis of Coagulase (coa) Gene PCR Products
| Coagulase | ||
|---|---|---|
| Antibiotics | Coagulase + | Coagulase - |
| Oxacillin | 4/487 ± 19/090cd | 16/700 ± 2/830ab |
| Chloramphenicol | 4/442 ± 23/950b | 15/500 ± 3/028a |
| Tetracycline | 11/815 ± 29/220a | 17/000 ± 2/828ab |
| Vancomycin | 2/745 ± 20/800bc | 16/000 ± 1/333abc |
| Kanamycin | 4/125 ± 18/530cd | 1/729 ± 15/900abc |
| Nalidixic acid | 5/026 ± 15/210d | 2/936 ± 13/200c |
| Gentamicin | 4/651 ± 20/590bc | 4/111 ± 15/300bc |
| Penicillin | 3/976 ± 15/150d | 3/551 ± 13/110c |
4. Discussion
Staphylococcus aureus is the most important pathogen of human resources mainly wound, respiratory tract and skin infections. Infection spreads in hospitals because of close contact and the point that hospitals staff and patients carry antibiotic resistant S. aureus specially (MRSA) in their nose or on their skin [3, 4, 17].
Staphylococci, especially S. epidermidis are parts of the natural flora of human skin and digestive and respiratory tracts. [18].
This organism is one of the main agents of nosocomial infections which are becoming increasingly resistance to antibiotics of beta-lactam and vancomycin groups [5]. The main factor in the survival of these microorganisms in spite of numerous anti-staphylococcal antibiotics is their ability to become resistant against antimicrobial agents.
Conducting antimicrobial tests on pathogenic bacteria in patients can provide good guidance regarding how to proceed for treatment. Although various studies have shown different results of bacterial resistance and carriers which may be related to various bacterial detecting methods [17]. Morelli et al. in a study on 1,633 unique S. aureus isolates reported. All isolates were susceptible to trimethoprim sulfamethoxazole, linezolid, ceftaroline, and rifampin, while the majority of isolates were susceptible to clindamycin, tetracycline, and mupirocin [19]. Also, Sun et al. conducted a descriptive study in China on specific molecular and epidemiological characteristics of S. aureus in patients in Xinyang, China. Several antibiotic-resistant genes were examined. All the samples were sensitive to vancomycin and daptomycin, 98.1% resistant to penicillin, and 9.3 resistant to chloramphenicol [12].
Coagulase protein is a main virulence factor in S. aureus so addition to its important role in diagnosis S. aureus [17, 20].
The coa gene amplificationhas been considered a simple and accurate method for typing of S. aureus isolated from distinct sources, the coagulase protein is an important virulence factor of S. aureus. Like spa, coa has a polymorphic repeat region that can be used for differentiating S. aureus isolates. The variable region of coa gene is comprised of 81 bp tandem short sequence repeats (SSRs) [21].
In the current study, 20 samples of S. aureus and 10 samples of coagulase-negative staphylococci were studied to antibiotic resistance patterns against disks of penicillin, tetracycline, gentamicin, chloramphenicol, oxacillin, vancomycin, kanamycin, and nalidixic acid. Then, all of the isolates were analyzed for the presence of coagulase gene using polymerase chain reaction.
As to the results, coagulase-positive samples showed higher resistance towards antibiotics. Statistically, there was not a significant difference between inhibition zone diameters of oxacillin, nalidixic acid, gentamicin, kanamycin, and penicillin. Isolates of S. aureus were 25% resistant to kanamycin and 55% to nalidixic acid. Resistance to tetracycline and gentamicin was 20%. All of the isolates were sensitive to vancomycin and resistant to penicillin.
Staphylococcus epidermidis and S. saprophyticus isolates showed 10% resistance to oxacillin, tetracycline, and kanamycin. All of the isolates were sensitive to chloramphenicol and vancomycin.
To conclude, prevalence of S. aureus and S. epidermidis in hospitals is increasing. Coagulase-positive samples showed more resistance to antibiotics, which confirms the virulence of S. aureus based on Talebi Satlou et al. study [14]. The reports in this study and other reports emphasized that they were 100% resistant to penicillin. Coagulase gene has variance of amplicon which is in line with the reports of Talebi Satlou et al. [14]. In the present study, PCR products of different sizes were obtained by amplification of the coa gene, similar to other researchers in Iran and different parts of world [16, 17, 22].
Results of the study suggest that PCR is a safe and accurate way to detect coagulase gene in bacteria. Thus, choosing the right antibiotic, continuous monitoring of resistance patterns, and proper treatment of staphylococcal infections are of most importance. As to the literature regarding PCR technique, which has been carried out with other methods such as Ethanol, various ranges of size have been observed, highlighting such variety for Coagulase gene [22, 23]. Genotypic variation among different S. aureus isolates, which may be considered as an important criterion when treating staphylococcal infection [24].
4.1. Conclusions
Coagulase gene polymorphism analysis provides easy and early analysis of the clonal relatedness of isolates. This study emphasize the genotypic variation among different S. aureus isolates, which may be considered as an important criterion when treating staphylococcal infections. And finally, since coagulase gene has a variety of band sizes and, as reported in different sources, is polymorphic; more studies are required in this area. Moreover, due to the importance of staphylococci, genomic studies on enterotoxins in S. aureus and coagulase-negative staphylococci is suggested.
Acknowledgements
References
-
1.
Babu NR, Shree GB, Rekha L, Karthiga P. Molecular analysis of coagulase, (COA) gene polymorphism in clinical isolates of Staphylococcus aureus by PCR, RFLP. Int J Innov Res Sci Eng Technol. 2014;3:8163-8.
-
2.
Jawetz L. Medical microbiology. 2 ed. California: Appleton and Lange; 2007.
-
3.
Yano K, Minoda Y, Sakawa A, Kuwano Y, Kondo K, Fukushima W, et al. Positive nasal culture of methicillin-resistant Staphylococcus aureus (MRSA) is a risk factor for surgical site infection in orthopedics. Acta Orthop. 2009;80(4):486-90. [PubMed ID: 19593719]. https://doi.org/10.3109/17453670903110675.
-
4.
Anwar MS, Jaffery G, Rehman Bhatti KU, Tayyib M, Bokhari SR. Staphylococcus aureus and MRSA nasal carriage in general population. J Coll Physicians Surg Pak. 2004;14(11):661-4. [PubMed ID: 15530274].
-
5.
Chambers HF. Methicillin resistance in staphylococci: molecular and biochemical basis and clinical implications. Clin Microbiol Rev. 1997;10(4):781-91. [PubMed ID: 9336672].
-
6.
Weinstein R. Hospital acquired infections. In: Kasper D, Fauci A, Longo D, Harrison S, editors. Principles of internal medicine. 16 ed. New York: MC Graw Hill; 2005. p. 775-821.
-
7.
Friedman DA, Ratard RC. The Louisiana antibiogram In vitro antibiotic sensitivity patterns 2003, 2004. Louisiana, Louisiana State University School of Public Health and Louisiana Department of Health: Louisiana State University School of Public Health and Louisiana Department of Health; 2007. 6 p.
-
8.
Woodford N, Sundsfjord A. Molecular detection of antibiotic resistance: when and where? J Antimicrob Chemother. 2005;56(2):259-61. [PubMed ID: 15967769]. https://doi.org/10.1093/jac/dki195.
-
9.
Schroder A, Schroder B, Roppenser B, Linder S, Sinha B, Fassler R, et al. Staphylococcus aureus fibronectin binding protein, a induces motile attachment sites and complex actin remodeling in living endothelial cells. Mol Biol Cell. 2006;17(12):5198-210. https://doi.org/10.1091/mbc.E06-05-0463.
-
10.
Hrabak J, Zemanova A, Chudackova E. [Mobile genetic elements in the epidemiology of bacterial resistance to antibiotics]. Epidemiol Mikrobiol Imunol. 2010;59(2):55-66. [PubMed ID: 20586167].
-
11.
Hosseinpour M, Sabokbar M, Bakhtiyari A, Parsa SH. Tracking comparative Salmonella in assembled isolate from Tehran with three methods, molecular, culture and ELISA. J microbiol world. 1392;1(14):62-72.
-
12.
Sun DD, Ma XX, Hu J, Tian Y, Pang L, Shang H, et al. Epidemiological and molecular characterization of community and hospital acquired Staphylococcus aureus strains prevailing in Shenyang, Northeastern China. Braz J Infect Dis. 2013;17(6):682-90. [PubMed ID: 23916451]. https://doi.org/10.1016/j.bjid.2013.02.007.
-
13.
Goh SH, Byrne SK, Zhang JL, Chow AW. Molecular typing of Staphylococcus aureus on the basis of coagulase gene polymorphisms. J Clin Microbiol. 1992;30(7):1642-5. [PubMed ID: 1352784].
-
14.
Talebi Satlou R, Ahmadi M, Dastmalchi Saei H. Restriction fragment length polymorphism genotyping of human staphylococcus aureus isolates from two hospitals in urmia region of iran using the Coa gene. Jundishapur J Microbiol. 2012;5(2):416-20. https://doi.org/10.5812/jjm.3522.
-
15.
Duran N, Ozer B, Duran GG, Onlen Y, Demir C. Antibiotic resistance genes & susceptibility patterns in staphylococci. Indian J Med Res. 2012;135:389-96. [PubMed ID: 22561627].
-
16.
Hookey JV, Richardson JF, Cookson BD. Molecular typing of Staphylococcus aureus based on PCR restriction fragment length polymorphism and DNA sequence analysis of the coagulase gene. J Clin Microbiol. 1998;36(4):1083-9. [PubMed ID: 9542942].
-
17.
Afrough P, Pourmand MR, Sarajian AA, Saki M, Saremy S. Molecular investigation of staphylococcus aureus, Coa and spa genes in ahvaz city hospitals staff nose compared with patients clinical samples. Jundishapur J Microbiol. 2013;6(4):5377.
-
18.
Brooks GF, Carroll KC, Butel JS, Morse SA. Jawets, melnick and adelbergs medical microbiology. 24 ed. NewYork: McGraw, Hill; 2007.
-
19.
Morelli JJ, Hogan PG, Sullivan ML, Muenks CE, Wang JW, Thompson RM, et al. Antimicrobial Susceptibility Profiles of Staphylococcus aureus Isolates Recovered from Humans, Environmental Surfaces, and Companion Animals in Households of Children with Community-Onset Methicillin-Resistant S. aureus Infections. Antimicrob Agents Chemother. 2015;59(10):6634-7. [PubMed ID: 26248385]. https://doi.org/10.1128/AAC.01492-15.
-
20.
Soltan Dallal MM, Khoramizadeh MR, Amiri SA, Saboor Yaraghi AA, Mazaheri Nezhad Fard R. Coagulase gene polymorphism of Staphylococcus aureus isolates, A study on dairy food products and other foods in Tehran, Iran. Food Sci Hum Wellness. 2016;5(4):186-90. https://doi.org/10.1016/j.fshw.2016.09.004.
-
21.
Hamza DA, Dorgham SM, Arafa A. Coagulase gene typing with emphasis on methicillin resistance staphylococci, Emergence to public health. Adv Infect Dis. 2015;5(4):196-203. https://doi.org/10.4236/aid.2015.54025.
-
22.
Osmonov D, Ozcan KS, Erdinler I, Altay S, Yildirim E, Turkkan C, et al. Cardiac device related endocarditis, 31 Years experience. J Cardiol. 2013;61(2):175-80. https://doi.org/10.1016/j.jjcc.2012.08.019.
-
23.
Sakoulas G, Cold HS, Vencataraman L, Degirolami PC, Eliopouls GM, Qian Q. Methicillin resistant staphylococcus aureus, comparison of susceptibility testing methods and analysis of mecA positive susceptible Strains. J clin microbial. 2001;39(11):3946-51.
-
24.
Mahmoudi H, Arabestani MR, Mousavi SF, Alikhani MY. Molecular analysis of the coagulase gene in clinical and nasal carrier isolates of methicillin-resistant Staphylococcus aureus by restriction fragment length polymorphism. J Glob Antimicrob Resist. 2017;8:41-5. [PubMed ID: 27987442]. https://doi.org/10.1016/j.jgar.2016.10.007.