Abstract
Background:
The lateral thoracic-lumbar-scapular region is an ideal source to supply flaps. The study towards improving the method of taking flaps towards conserving a part of the muscle needs to clarify the ratio of branching forms of the arteries in the muscle.Objectives:
This study was done to describe the typical anatomy, the anatomical and size variations of subscapular and circumflex scapular vessels, the branching and distribution of vascular pedicle supplying latissimus dorsi muscle flap, and serratus anterior muscle flap of circumflex scapular vessels.Methods:
We conducted a cross-sectional study on 24 corpses of adults of both genders. The flap vessels were revealed through two stages of surgery, including the axillary region and the lumbar-scapular region. We classified the collected information and recognized typical and transformed forms based on statistical data.Results:
The subscapular artery was separated by the axillary artery, the general origin of the circumflex scapular artery, and the thoracodorsal artery. Subscapular vessels were found in 40/42 cases, accounting for 95.2%, and the length and diameter were 3.04 ± 0.51 cm and 2.85 ± 0.46mm, respectively. The circumflex scapular artery, which had originated from the subscapular artery, was found in 40/42 cases. It also showed origin from subscapular artery with 2/42 cases. The length of the circumflex scapular artery was 3.14 ± 0.70 cm, and its diameter was 2.46 ± 0.48 mm. Terminal branches of the circumflex scapular artery were very variable. Almost all branching forms of the artery in the latissimus dorsi muscle were external branches, but they might be present or not in internal and recurrent branches.Conclusions:
The vascular pedicle’s distribution, size, and presence were influenced by the subscapular artery supply flaps. Due to the diverse blood supply from the flaps’ vessels, the surgeon can use the flaps based on the subscapular artery in many forms. These flaps could be used as a seamless vascular flap or a free flap in orthopedic surgery.Keywords
Flaps Latissimus Dorsi Muscle Flap Serratus Anterior Muscle Flap Vascular Pedicle Subscapular Artery
1. Background
The lateral thoracic-lumbar-scapular region is an ideal source for flaps supply. The flaps, which are taken from this region prevail in many body flaps. These are also suitable for anatomical, functional, and aesthetic requirements of both flap’s donor and recipient sites (1, 2). The anatomical structures in this region are nourished by the branch system of the subscapular artery that is the biggest branch of the axillary artery (3). Typical characteristics of the thoracic–lumbar region’s flaps are the same as subscapular vessels with two thoracodorsal branches and a circumflex scapular branch. Each branch splits into vascular pedicles with each flap. Therefore, general vascular pedicles may be used to extend and increase the diameter of any particular vascular pedicle of any flap or serve as a common vascular pedicle for a bunch of flaps (4).
According to medical literature, the anatomical foundation of the flaps of the lateral thoracic–lumbar–scapular region has been studied at different levels (5). The medical literature also has indicated that the vascular pedicles of each flap could be variable. Latissimus dorsi muscle flap is one of the most researched and applied factors. In the flap transfer methods, the flap is taken towards conserving a part of the muscle. The proportion of branched samples should be clearer about arteries in that muscle (1, 6). Serratus anterior muscle flaps have not been widely studied, particularly in Vietnam (7-10). The vascular branches entering the serratus anterior muscle are often varied regarding quantum and origin; additional data on this aspect are needed if these differences are clinically significant. Circumflex scapular artery and its terminal branches located in circumflex scapular artery go over medial triangular space reported in just around 60% of cases (11). The branching and distribution of the terminal cutaneous branches into the scapular and lateral scapular flap regions have not been well described, especially the ascending cutaneous branch. We think that these problems need to be further studied.
The reference sources indicated that the vascular pedicle supplying each flap often had approached its research by the author; thus, they are superficial and local. Therefore, the relationship between anatomical and clinical ties has not been considered adequately.
2. Objectives
We aimed to describe typical anatomy and the anatomical and size variations of subscapular and circumflex scapular vessels. We also described the branching and distribution of vascular pedicle supplying latissimus dorsi muscle flap and serratus anterior muscle flap of the circumflex scapular vessels.
3. Methods
3.1. Study Design and Population
We conducted a cross-sectional descriptive study using macroscopic dissection on formalin corpses using color injection and photographing. The study was conducted with a convenience sampling method and included 24 adult Vietnamese corpses who had died not due to diseases of the skin, muscles, blood vessels, and scapular, axillary, and lumbar regions were intact. There were 22 formalin corpses, and two fresh cadavers were under 24 hours of preservation at the Department of Anatomy, Hanoi Medical University and Department of Anatomy, Can Tho University of Medicine and Pharmacy. Twenty-one corpses had an entire vascular analysis of the flap that needed to be studied. Three corpses could only be anatomy vascular pedicle of the flap and latissimus dorsi muscle flap; the samples lost due to poor quality and damage during dissection were rejected. We, therefore, collected 42 specimens of vascular pedicle of the scapular and lateral scapular flaps, 42 specimens of vascular pedicle of serratus anterior myocutaneous flap, and 47 specimens of latissimus dorsi myocutaneous flap.
3.2. Anatomical Methods
Tools and materials needed for this research included conventional anatomy kits, microsurgical scissors, 4.5× magnifier, Swedish micrometer calipers, and specialized ruler with unit divisions to 0.1mm. Circuit pump kits included syringes of various sizes, needle sticks, catheters, and methylene blue staining. The dissection, color injection, and photographing after painting on blood vessels were techniques we used in this study.
Vascular of the flap was revealed through two stages of dissection. Firstly, we dissected the axillary region of corpses. The corpse was placed in the supine position, incision, and axillary skin with conventional techniques. The pectoralis major muscle and pectoralis minor muscles were cut, respectively. Then, the corpses were turned up to dissect the subscapular vessels. The branches of this artery included the circumflex scapular, thoracodorsal vessels, and the branches from the thoracodorsal vessels to the latissimus dorsi muscle and serratus anterior muscle. The circumflex scapular artery was dissected to the medial triangular space. Then, we poked a needle through the medial triangular space to the back to set the mark for the circumflex scapular artery in stage 2. The vascular pedicle in the serratus anterior muscle and the long thoracic nerve was dissected to the end of digitation. The vascular pedicle in the latissimus dorsi muscle and the thoracodorsal nerve was dissected to the navel.
Secondly, we dissected the lumbar–scapular region. The corpse’s body was placed in the prone position. The vascular pedicle of the scapular and the lateral scapular flaps (the terminal branches of the circumflex scapular artery) were dissected separately from the branching of the vascular pedicle supplying latissimus dorsi muscle. The location of the plugin in the first stage was indicated based on the needle. The skin was incised at the line of the anterior axillary, revealing the medial triangular space. Then, we made the teres muscles wider, and found the circumflex scapular artery, and observed the branching of infraspinatus and subscapularis muscles. After finding the terminal branches, we dissected the branches to the smallest branches. Finally, we injected the methylene blue stain into the artery, and measured the stained skin’s size, and took a picture.
3.3. Statistical Analysis
We classified the collected information, and based on the obtained data, we recognized typical and transform forms. Descriptive statistics were used to summarize categorical (proportions and frequencies) and continuous variables (means and standard deviations). Data were analyzed by Statistical Package for Social Sciences (SPSS) version 22.0 (IBM Corp., New York, the United States of America) for Windows. The chi-square test was used to investigate the relationship between the rates of two qualitative variables.
3.4. Ethical Approval
The ethical issue for this study was approved by the Institutional Review Board of Hanoi Medical University with the code of 1416/YHN-QD.
4. Results
4.1. Subscapular Vessels
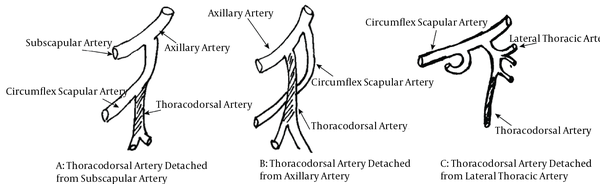
The subscapular artery had been separated by the axillary artery, the general origin of the circumflex scapular artery, and the thoracodorsal artery. In contrast, it was absent when the subscapular artery and thoracodorsal artery were separated independently. The circumflex scapulary was the branch of the axillary artery; the thoracodorsal was the branch of the axillary artery or the lateral thoracic artery (Figure 1). Subscapular vessels were found in 40/42 cases, accounting for 95.2%. The diameter and length of them are shown in Table 1.
Origin of the subscapular vessels
Size of the Subscapular Vessels and Dependent Arteries
| Diameter (mm) | Length (cm) | |
|---|---|---|
| Subscapular artery | 2.85 ± 0.46 | 3.04 ± 0.51 |
| Subscapular vein | 2.86 ± 0.48 | 3.04 ± 0.51 |
| Circumflex scapular artery | 2.46 ± 0.48 | 3.14 ± 0.70 |
| Circumflex scapular vein | 3.24 | 3.14 ± 0.70 |
| Terminal branches | ||
| Cutaneous scapular flap artery (n = 42) | 0.95 ± 0.29 | 5.13 ± 0.62 |
| Cutaneous parascapular flap artery (n = 38) | 0.45 ± 0.24 | 5.13 ± 1.69 |
| Ascending cutaneous artery (n = 33) | 0.43 ± 0.11 | 2.80 ± 0.85 |
| Deep branches | 1.2 ± 0.2 | - |
| Vascular pedicle | ||
| Main trunk | 1.88 ± 0.38 | 2.64 ± 0.30 |
| Upper branch | 1.04 ± 0.20 | 0.98 ± 0.17 |
| Lower branch | 1.18 ± 0.21 | 1.09 ± 0.18 |
| Muscle digitation branch | 0.36 ± 0.08 | 1.06 ± 0.24 |
4.2. Circumflex Scapular Vessels
The diameter and length of circumflex scapular vessels are also shown in Table 1. Circumflex scapular artery, which originated from a subscapular artery, had 40/42 cases. It also has origin from subscapular artery with 2/42 cases. We also found that the circumflex scapular vein had one vein with 39/42 cases and two with 3/42 cases. Besides, the circumflex scapular vein pours subscapular vein and axillary vein in 40/42 and 2/42 cases, respectively. Terminal branches of the circumflex scapular artery had four types in this study. Type I was one transverse cutaneous branch and many small lateral branches (about 9.5% with 4/42 cases). The rate of type II, which had three superficial cutaneous branches of the scapular, lateral scapular, and ascending cutaneous vessels from the scapular dermis, was found in about 16.7% (7/42 cases). Type III included three superficial cutaneous branches: cutaneous scapular artery, lateral scapular, and ascending cutaneous artery, had 26/42 cases (61.9%). Type IV had 5/42 cases (11.9%) with four superficial cutaneous branches: 2 cutaneous scapular branches and two cutaneous lateral scapular branches (Figure 2).
Type of terminal branches
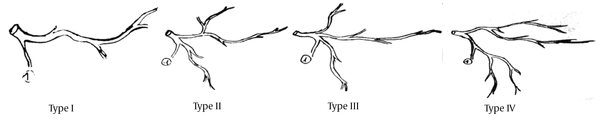
The cutaneous scapular flap artery (n = 42) of the terminal branches had a distance with the spinous process and the scapular spine around 8.73 ± 0.87 and 3.73 ± 1.08 cm, respectively. Similarly, the cutaneous parascapular flap artery (n = 38) had a distance with the lower angle of the clavicle and the lateral edge of the clavicle around 0.97 ± 0.14 and 1.61 ± 0.63 cm, respectively. Ascending cutaneous artery (n = 33) and deep branches in the superior lateral border were also the terminal branches, and their size is shown in Table 1. The axis of the cutaneous scapular flap artery was 15° above the horizontal line, the axis of the cutaneous parascapular flap artery was 60° under the horizontal line, and the axis of ascending cutaneous artery was 82.5° above the horizontal line. The size of the ingrain area of the circumflex artery in two specimens was 12 - 14 × 10 - 12 cm
4.3. Thoracodorsal Vessels and the Vascular Pedicle Supplying Serratus Anterior Muscle
The origin of the thoracodorsal artery had 95.2% from subscapular (40/42 cases), 2.4% from an axillary artery (1/42 case), and 2.4% lateral thoracic artery (1/42 case). The length of them was 5.46 ± 0.51 cm, and the average diameter was 2.28 ± 0.56 mm. The veins always went along with the arteries.
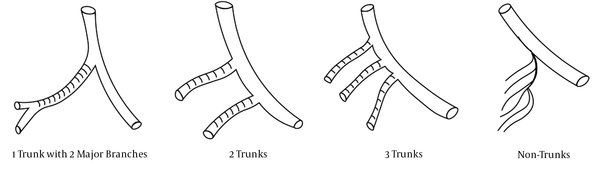
Branching types of the artery gets in serratus anterior muscle had four types (Figure 3). The schematic illustration of them is shown in Figure 4 that included one trunk with two major branches, two trunks, three trunks, and non-trunks (toothcomb) with the rates of 57.1%, 23.8%, 7.1%, and 11.9%, respectively. The diameter and length of the vascular pedicle supplying the serratus anterior muscle, which included the main trunk, upper branch, lower branch, and muscle digitation branch are presented in Table 1.
The branched forms of the artery located in serratus anterior muscle
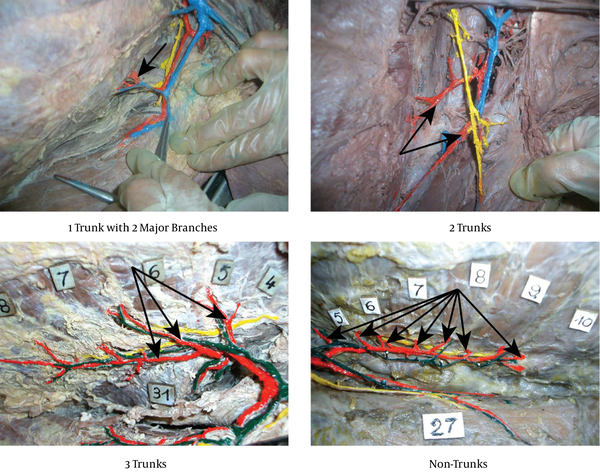
The branched form schematic illustration of the artery located in serratus anterior muscle
The size of serratus anterior digitations is shown in Table 2. The average length of the vascular pedicle supplying the serratus anterior muscle (including the length of the thoracodorsal artery and subscapular artery) was 11.10 ± 1.26 cm. The length of the long thoracic nerve that had the origin from the place that accompanied the artery was 9.36 ± 1.15 cm and its diameter was 1.51 ± 0.04 mm.
Size of the Serratus Anterior Digitations
| Digitations | Average Length (cm) | Average Width (cm) |
|---|---|---|
| Digitation no.5 | 10.51 ± 0.31 | 2.54 ± 0.23 |
| Digitation no.6 | 10.98 ± 0.32 | 3.05 ± 0.29 |
| Digitation no.7 | 11.52 ± 0.27 | 3.12 ± 0.24 |
| Digitation no.8 | 11.01 ± 0.29 | 2.85 ± 0.22 |
| Digitation no.9 | 9.48 ± 0.30 | 2.27 ± 0.20 |
4.4. Vascular Pedicle Supplying the Flaps and the Skin of Latissimus Dorsi
Branching forms of the artery located in the latissimus dorsi muscle are shown in Table 3. We found 47/47 specimens of the musculocutaneous perforators that had origined from an external branch (the one that runs parallelly with the lateral edge of the latissimus dorsi muscle). There were only five among 47 specimens that had originated from an external branch and other branches. Some musculocutaneous perforators from the external branch are presented in Table 3. When we compared locations of an external branch, we found that the external branch was distanced with the lateral latissimus dorsi muscle and insertion of muscle about 2.49 cm ± 0.246 and 11.05 cm ± 6.32 cm, respectively.
Branched Form of the Artery Located in Latissimus Dorsi Muscle and Quantum of Musculocutaneous Perforators from an External Branch (n = 47)
| Frequency (%) | |
|---|---|
| Branched form of the artery located in latissimus dorsi muscle | |
| 1 Branch (only had external branch) | 2 (4.3) |
| 2 Branches (including external branch and internal branch) | 24 (51) |
| 3 Branches (including (external branch, internal branch, and recurrent branch) | 21 (44.7) |
| Quantum of musculocutaneous perforators from external branch | |
| 3 Branches | 9 (19.1) |
| 4 Branches | 17 (36.2) |
| 5 Branches | 17 (36.2) |
| 6 Branches | 4 (8.5) |
The length of the latissimus dorsi muscle was 20.89 cm ± 2.66 cm, and its width was 13.39 ± 2.00 cm. Methylene blue stain was used as an indicator for the blood that nourished the latissimus dorsi muscle. When we injected a methylene blue stain into a thoracodorsal artery, we found the color of the stain exceeded the limits of these muscles. The accompanying thoracodorsal nerve - segment was 8.36 cm ± 1.20 cm in length and 1.46 cm ± 0.12 cm in diameter.
The average value of the angles that were created by the trunk of the thoracodorsal artery and branch of the artery located in serratus anterior muscle (α1), and the angle formed by the two main branches of the thoracodorsal artery, which runs inside the latissimus dorsi muscle (α2) were 45°. These angles could be changed around the ranges from 40° to 80°.
5. Discussion
5.1. Principal Findings
Based on the subscapular artery, all the flaps had a long vascular pedicle, big diameter, and little change if transported to the entire vascular pedicle. Vascular morphology helped for using simultaneous multiple flaps on a common vascular pedicle. Latissimus dorsi muscle flap and serratus anterior muscle flap could be used in flaps that had been gone along with motor nerves because these vascular pedicles were accompanied by large nerves (long thoracic and thoracodorsal nerves) in a long segment. Branch morphology of serratus anterior muscle digitations or parts of latissimus dorsi muscle helped the surgeon flexibly to take the flaps.
5.2. Possible Explanations and Comparison with Other Studies
In comparison with the study by Serafin, anatomy circumflex scapular artery results of us and My PV. in Vietnamese people only differed in quantity artery; although Serafin and My PV. found two circumflex scapular arteries with 8% and 1.67%, and we did not find any cases. There was no difference in changing rate of the origin of the circumflex scapular artery and its length and diameter of the artery between our study and the reports of My and Serafin, et al. (7, 12). The changes in the position where the descending cutaneous branches appeared in Upton’s study accounted for 10% of cases (30 cases) and appeared below teres major. However, our study detected that these branches were always presented in medial triangular space with 42 cases (13).
Three terminal branches of the circumflex scapular artery were described in several studies. Ohsaki and Maruyama explained the ascending cutaneous branch clearly (with the rate of 100%), and Upton told a variation of descending cutaneous branch position (13, 14). There were 4 of 42 cases (9.5%) of the cutaneous branch form (scapular cutaneous branch) with small lateral branches in our study. We recognized that this form had specific effects on getting lateral scapular, ascending, or L-shaped flaps, and it might be the cause of necrosis for these flap types.
As a branch of the thoracodorsal artery, the serratus anterior artery will be tightened using a simple latissimus dorsi muscle flap or both latissimus dorsi muscle and serratus anterior muscle flap. Table 4 shows the length and diameter of the vascular pedicle supplying latissimus dorsi muscle from the origin of the subscapular artery compared to the results of other authors (11, 15-18).
Comparing the Length and Diameter of Vascular Pedicle Supplying Latissimus Dorsi Muscle from the Origin of the Subscapular Artery
The ratio of the two branches of branching forms of the artery located in the latissimus dorsi muscle was not as high as the ratio reported by Lamberty (94%). It had a rate of only 51% in our study (19). The other forms included three branches with a large percentage of 44.7%, while there was one branch traveling along the lateral side (4.4%). Also, there was one branch distancing 2.49 cm from the lateral side. Thus, taking the flap with only a part of the latissimus dorsi muscle could be the best choice based on one branch. Besides, almost the external branch is dissected from a branch of musculocutaneous perforators. Most of the branches of musculocutaneous perforators dissected from an external branch of the latissimus dorsi muscle were a suitable choice. Tuat and Hai have shown that the skin area injected by stain into the thoracodorsal artery consistently exceeds the limit of muscles. The vitality of musculocutaneous flaps has been proved in the clinical setting (20, 21).
5.3. Strengths and Weaknesses of the Study
Because of studying Vietnamese corpses, we found more clinical evidence for flap transfer surgery improvement in Vietnam. Because the number of corpses was limited, we injected stains to study only two specimens. We also could not set up selective studies on musculocutaneous branches in fresh corpses. Besides, we need more research on digital subtraction angiography (DSA), computed tomography (CT), and magnetic resonance imaging (MRI) to learn about the branching pattern, length, and diameter of the subscapular artery to study generalize the data to larger sample size and catch more objective data on the flap on this artery.
5.4. Conclusions and Implications
The flaps that were based on subscapular arteries had many advantages when they were rotated independently or locally. Vascular morphology helped for using simultaneous multiple flaps on a common vascular pedicle. Each digitation of serratus anterior muscle, measured 2 × 10 cm, was compatible with the functional recovery of small muscles, especially for the face area. The capability of dissecting a flap with skin or bone helped complex injuries recovery became easier. Because the thoracodorsal nerve had no lateral branch, it was not affected by the scapular movement when we cut this nerve. Otherwise, the size of the thoracodorsal nerve could be used to restore paralyzed muscles to reanimate movement by microsurgery.
We recommend that clinicians use the flaps based on the subscapular artery in many forms: skin flap, simple muscle flap, or complex flap. These flaps could be used as a seamless vascular flap or a free flap. We consider using the extended scapular flap based on the ascending circumflex scapular artery. The latissimus dorsi muscle flap is a suitable choice when taking a part of the muscle or the lateral vertical axis of the muscle.
Acknowledgements
References
-
1.
Elzawawy EM, Kelada MN, Al Karmouty AF. Design of mini latissimus dorsi flap based on thoracodorsal vascular patterns. Ann Plast Surg. 2018;80(6):607-15. [PubMed ID: 29664831]. https://doi.org/10.1097/SAP.0000000000001403.
-
2.
Khan MN, Rodriguez LG, Pool CD, Laitman B, Hernandez C, Erovic BM, et al. The versatility of the serratus anterior free flap in head and neck reconstruction. Laryngoscope. 2017;127(3):568-73. [PubMed ID: 27279461]. https://doi.org/10.1002/lary.26116.
-
3.
Paulsen F, Böckers TM, Waschke J, Winkler S, Dalkowski K, Mair J, et al. Sobotta anatomy textbook: English edition with Latin nomenclature. Amsterdam, Netherlands: Elsevier Health Sciences; 2018.
-
4.
Hallock GG. The extended latissimus dorsi-serratus anterior chimeric local free flap for salvage of the complicated posterolateral thoractomy incision. Injury. 2019;50(Suppl 5):S8-S10. [PubMed ID: 31784056]. https://doi.org/10.1016/j.injury.2019.10.038.
-
5.
Sood A, Therattil PJ, Russo G, Lee ES. Functional latissimus dorsi transfer for upper-extremity reconstruction: A case report and review of the literature. Eplasty. 2017;17. e5. [PubMed ID: 28293330]. [PubMed Central ID: PMC5317028].
-
6.
Sia WT, Xu GG, Puhaindran ME, Tan BK, Cheng MH, Chew WY. Reconstruction of extensive soft-tissue defects with concomitant bone defects in the lower extremity with the latissimus dorsi-serratus anterior-rib free flap. J Reconstr Microsurg. 2015;31(6):407-13. [PubMed ID: 26036785]. https://doi.org/10.1055/s-0035-1548741.
-
7.
My PV. [An anatomical arteries study for blood supply serratus anterior muscles in Vietnamese people]. Ho Chi Minh City, Vietnam: Ho Chi Minh City University of Medicine and Pharmacy; 2021. Vietnamese.
-
8.
Webb AL, O'Sullivan E, Stokes M, Mottram S. A novel cadaveric study of the morphometry of the serratus anterior muscle: One part, two parts, three parts, four? Anat Sci Int. 2018;93(1):98-107. [PubMed ID: 27757809]. https://doi.org/10.1007/s12565-016-0379-1.
-
9.
Tamburino S, Menez T, Laloze J, Michot A, Paillet P, Perrotta RE, et al. Free serratus anterior artery perforator flap: A case report with an anatomic and radiological study. Surg Radiol Anat. 2017;39(8):837-42. [PubMed ID: 28236131]. https://doi.org/10.1007/s00276-017-1824-0.
-
10.
Gordon L, Levinsohn DG, Finkemeier C, Angeles A, Deutch H. The serratus anterior free-muscle transplant for reconstruction of the injured hand: An analysis of the donor and recipient sites. Plast Reconstr Surg. 1993;92(1):97-101. [PubMed ID: 8516412]. https://doi.org/10.1097/00006534-199307000-00014.
-
11.
Serafin D, Georgiade NG. Microsurgical composite tissue transplantation. Ann Surg. 1978;187(6):620-8. [PubMed ID: 646501]. [PubMed Central ID: PMC1396442]. https://doi.org/10.1097/00000658-197806000-00006.
-
12.
Serafin D, Rios AV, Georgiade N. Fourteen free groin flap transfers. Plast Reconstr Surg. 1976;57(6):707-15. [PubMed ID: 775516]. https://doi.org/10.1097/00006534-197606000-00005.
-
13.
Upton J, Albin RE, Mulliken JB, Murray JE. The use of scapular and parascapular flaps for cheek reconstruction. Plast Reconstr Surg. 1992;90(6):959-71. [PubMed ID: 1448531]. https://doi.org/10.1097/00006534-199212000-00003.
-
14.
Ohsaki M, Maruyama Y. Anatomical investigations of the cutaneous branches of the circumflex scapular artery and their communications. Br J Plast Surg. 1993;46(2):160-3. [PubMed ID: 8461907]. https://doi.org/10.1016/0007-1226(93)90152-2.
-
15.
Strauch B. Atlas of microvascular surgery: Anatomy and operative approaches. New York, USA: Thieme Medical Publishers; 1993. p. 504-22.
-
16.
Cormack GC, Lamberty BG. A classification of fascio-cutaneous flaps according to their patterns of vascularisation. Br J Plast Surg. 1984;37(1):80-7. [PubMed ID: 6692066]. https://doi.org/10.1016/0007-1226(84)90049-3.
-
17.
Bartlett SP, May JW, Yaremchuk MJ. The latissimus dorsi muscle: A fresh cadaver study of the primary neurovascular pedicle. Plast Reconstr Surg. 1981;67(5):631-6. [PubMed ID: 7232584].
-
18.
Cuong LV. [Arterial forms and abnormalities]. Ho Chi Minh City, Vietnam: Ho Chi Minh City University of Medicine and Pharmacy; 1991. Vietnamese.
-
19.
Cormack GC, Lamberty BGH. The arterial anatomy of skin flaps. Edinburgh, Scotland: Churchill Livingstone; 1994. 538 p.
-
20.
Hai LH. [Anatomy research and clinical applications of scapular, lateral scapular flap in the treatment of large soft defects in the shin, foot region]. Vietnam: Hanoi Medical University; 2005. Vietnamese.
-
21.
Tuat ND. Anatomical characteristics of Latissimus dorsi muscle of Vietnamese Human. Morphology. 1992;2(1):9.