Abstract
Introduction:
Hemimandibular hyperplasia is a facial deformity which may develop in any age and includes a unilateral enlarged mandibular condylar head, deviation of mandible and chins, elongated condylar neck or ramus, and an occlusal cant with open bite. Different surgical treatments are proposed in the literature from simple low or high condylectomy to more complex procedures combining osteotomies in different sites of the mandible. Surgical procedure is defined by the clinical evaluation and scintigraphic diagnosis of activity or inactivity in the center of condylar growth.Case Presentation:
This case report describes a 30-year-old female patient with left hemimandibular hyperplasia with activity of condylar growth, that was successfully treated with low condylectomy, asymmetric lefort I osteotomy and inferior border ostectomy on the affected side, and associated with a unilateral sagittal split ramus osteotomy on the contra-lateral side.Discussion:
The innovation on nerve dissection by removing the overlying buccal bone and performing inferior ostectomy under direct visualization of the nerve, proved to be a safe technique with a low risk of nerve damage.Keywords
1. Introduction
Condylar Hyperplasia (CH) of mandible and hemimandibular hyperplasia are very close pathologic conditions in which condyle is affected in a way that results in overgrowth of the mandible with significant facial asymmetry (1). CH begins in the second decade of life, continues to grow till the mid-20s and usually occurs bilaterally, but can occur unilaterally as well. There is facial asymmetry usually in a horizontal direction, protrusive and deviated mandible, articular dysfunction such as pain, joint sounds, and mouth opening limitations is seen due to the mandibular overgrowth (2, 3). There is a class III occlusion on the ipsilateral side and a cross-bite on the contra-lateral side (4, 5). Prominent radiographic features may include an elongated mandibular condylar head and neck with normal architecture, outward bowing of the body on the affected side and more flattening of the contra-lateral side (6-8). Suggested theories for the etiology and pathogenesis include hormonal influences, trauma, heredity, infections, arthrosis and hypervascularity (4, 9, 10). The most effective methods to diagnose CH and determine the active growth are serial radiographs (i.e. lateral cephalograms, cephalometric tomograms) and clinical evaluations. Bone scans may or may not be valuable in diagnosing CH because of its slow rate of growth (1, 11).
Hemimandibular hyperplasia which also has been termed as mandibular condylar osteochondromas or osteomas develops at any age, and may be slower in growing over the time, but never stops (12). Increased unilateral facial height and vertical and transverse chin asymmetry may be seen. In more rapid growing condition, a lateral open bite can be presented on the affected side, and in slow ones, maxillary canting with tilting of the occlusal plane and dental compensation can be observed (13). Radiographic features include an enlarged deformed condylar head, elongated condylar neck with increased thickness on the affected side, increased vertical height of ramus and body of mandible on the same side, and vertical alveolar bone growth for closing the lateral open bite. Bone scans may help in diagnosing the condition by the amount of isotope uptake, especially in rapid growing conditions (1).
This paper proposes a low condylectomy, lefort I osteotomies combined with unilateral sagittal split ramus osteotomy and inferior border ostectomy to correct the facial asymmetry due to hemimandibular hyperplasia. The combination of these operational methods has led to satisfying and beneficial outcomes in patients with unilateral overdevelopment of the face caused by hemimandibular hyperplasia.
2. Case Presentation
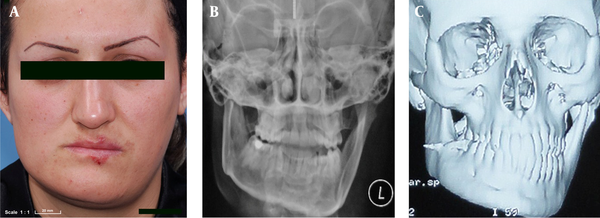
A 30-year-old female patient was visited at the Oral and Maxillofacial Surgery Department of the Tehran Azad University (Buali hospital) with the chief complaint of a deviated mandible and facial asymmetry that had begun eight years ago and affected her social life following adolescence (Figure 1). The patient reported that the left side of the jaw had grown more than the opposite side after the puberty, and continued till 28 years of age. There was no history of trauma or inflammation in the jaw and in the temporomandibular joint. The clinical examination revealed significant facial asymmetry, with deviation of the mandible and chin to the right side. The patient exhibited tilted lips and occlusal plane with maxillary canting near six mm in left side. Difference of the heights of the face from the lateral canthal to the gonial angle was one point four mm and there was no significant impairment or pain in movements of the mandible and joints. Panoramic radiography revealed elongation of the condylar neck, increasing the size and length of the condyle, with a downward projection of the angle and body of the left mandible. Computed tomography revealed deformity of the left side of the mandible. Scintigraphy revealed increased condylar activity on the left. According to these data, the diagnosis of hemimandibular hyperplasia was established (Figure 1).
Imaging of Facial Asymmetry
2.1. Technical Note and results
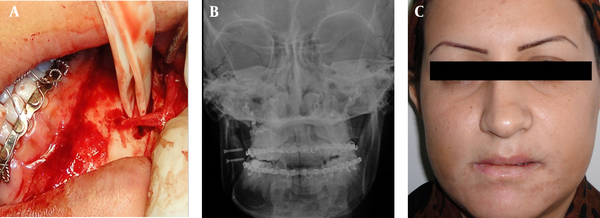
The height of the cuts was planned by using panoramic radiography and computed tomography. Al-kayat Bramely approach was chosen to make low condylectomy with six mm removal of the condylar head on the left and condylar neck was reshaped (ostectomy). Intraoral approach was performed to make the asymmetric lefort I osteotomy with impaction of five mm on the affected side and unilateral sagittal split ramus osteotomy for correction of the deviation of the mandibular midline and chin on the contra-lateral side. Then, an inferior border ostectomy on the left side of the mandible was performed, extending from the ramus to the symphysis region, passing with a three mm margin below the mental foramen. Seven millimeters of the body of the mandible was removed to the lowermost region of the mandible. In our technique, for protection of the inferior alveolar nerve, the buccal cortex overlying the inferior alveolar nerve was removed, the nerve was retracted with umbilical band, and the osteotomy was done under direct visualization of the nerve (Figure 2 a). Internal rigid fixation with miniplates and screws was used. Surgery steps are summarized in table 1. Panoramic radiography and postero-anterior skull radiograph shows the correction of the previous asymmetry after surgery (Figure 2 b). The patient has been in postoperative follow-up for two years and satisfied with her appearance (Figure 2c). There was no relapses, no joint symptoms, and no numbness after two years, and the occlusion and mandible movements remained normal.
Post-op Images of a 30-Year-Old Female With a Deviated Mandible and Facial Asymmetry
Surgical Steps in Order of Execution and Technical Note for Each Surgical Procedure
| Surgical Step | Technical Note |
|---|---|
| Condyle accesses | Al-kayat Bramely approach was chosen with regard to the facial nerve and damage to the nerve was avoided by using nerve stimulator. Low condylectomy was performed with six mm removal of the condylar head. |
| Condylar neck reshaping | In a convex form to perform as a new condyle. |
| Lefort I osteotomy | With an intraoral approach, the canting of maxilla by an asymmetric osteotomy was corrected with an impaction of five mm on the left and was subsequently fixed with miniplates according to the surgical splint made by model surgery. |
| Unilateral sagittal split osteotomy | With an intraoral approach, ascending ramus was incised until first molar tooth in the buccal groove region on the unaffected side, conventional osteotomy was performed and two screws were fixed after the intermaxillary fixation. |
| Nerve dissection | buccal cortex overlying the inferior alveolar nerve was removed, the nerve was retracted with umbilical band and the osteotomy was done under direct visualization of the nerve. |
| Inferior border ostectomy | Oscillatory saw was used to perform a linear osteotomy from the ramus to the symphysis region. Special care should be taken to achieve bicortical osteotomy without damage to soft tissues. |
3. Discussion
Different surgical treatments are proposed in the literature, from simple low or high condylectomy of the affected side to more complex procedures like single or both jaws osteotomies at different sites in the mandible (6). Most studies have indicated condyle resection with orthognathic treatment in active condyle growth (14). Wolford and Lebanc treated patients with active condylar hyperplasia by high condylectomy and mono- or bimaxillary surgery and showed predictable outcomes compared to those treated with orthognathic surgery alone (15). Lippold et al. declared that condylectomy in patients with active condylar growth can correct hemimandibular hyperplasia by treating the underlying disease (8). Follow-up or orthognathic treatment with no surgery on the condyle is indicated when the growth is inactive (16). Motamedi et al. (2) performed unilateral or bilateral ramus osteotomy for correction of the facial asymmetry when the growth is completed, without any surgery on the condyle, and the outcomes were acceptable.
Surgical treatment depends on the clinical assessment and the extent of skeletal deformity. Bone scans can be useful for the evaluation of any center of bone growth because of higher Technetium-99 uptake in the areas of increased osteoblastic activity (5), but Slootweg and Muller (11) and Grey at al. (3) found no correlation between the results of bone scans and histologic growth evidence, so bone scan alone is not reliable for diagnosing the condition.
There is a treatment protocol that was advocated by Wolford (1) for hemimandibular hyperplasia as follows: 1) Perform low condylectomy; 2) Reshape the condylar neck; 3) Perform orthognathic surgery; 4) Perform an inferior border ostectomy. Our case had most of the criteria's of the hemimandibular hyperplasia, so we performed this protocol with some innovation in nerve dissection because of the risk of nerve damage with this protocol. Removing the overlying buccal bone on the inferior alveolar nerve, retracting with umbilical band and performing inferior ostectomy under direct visualization proved to be a safe technique with a low risk of nerve damage, but it is quite complicated. Also, we overcorrected the remaining asymmetry with inferior ostectomy to overcome the positional compensatory of the head. There were no relapses, no joint symptoms, and no numbness after two years follow-up and the occlusion and mandible movements remained normal.
Acknowledgements
References
-
1.
Wolford LM. Facial Asymmetry; diagnosis and treatment consideration. 2 ed. 2009.
-
2.
Motamedi MH. Treatment of condylar hyperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofac Surg. 1996;54(10):1161-9. [PubMed ID: 8859233].
-
3.
Gray RJ, Sloan P, Quayle AA, Carter DH. Histopathological and scintigraphic features of condylar hyperplasia. Int J Oral Maxillofac Surg. 1990;19(2):65-71. [PubMed ID: 2111360].
-
4.
Yang J, Lignelli JL, Ruprecht A. Mirror image condylar hyperplasia in two siblings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(2):281-5. [PubMed ID: 14970789]. https://doi.org/10.1016/S1079210403005560.
-
5.
Cervelli V, Bottini DJ, Arpino A, Trimarco A, Cervelli G, Mugnaini F. Hypercondylia: problems in diagnosis and therapeutic indications. J Craniofac Surg. 2008;19(2):406-10. [PubMed ID: 18362718]. https://doi.org/10.1097/SCS.0b013e318069019f.
-
6.
Angiero F, Farronato G, Benedicenti S, Vinci R, Farronato D, Magistro S, et al. Mandibular condylar hyperplasia: clinical, histopathological, and treatment considerations. Cranio. 2009;27(1):24-32. [PubMed ID: 19241796].
-
7.
Kaya B, Arman A, Uckan S. Orthodontic and surgical treatment of hemimandibular hyperplasia. Angle Orthod. 2007;77(3):557-63. [PubMed ID: 17465670].
-
8.
Lippold C, Kruse-Losler B, Danesh G, Joos U, Meyer U. Treatment of hemimandibular hyperplasia: the biological basis of condylectomy. Br J Oral Maxillofac Surg. 2007;45(5):353-60. [PubMed ID: 17145124]. https://doi.org/10.1016/j.bjoms.2006.10.011.
-
9.
Egyedi P. Aetiology of condylar hyperplasia. Aust Dent J. 1969;14(1):12-7. [PubMed ID: 5252191].
-
10.
Oberg T, Fajers CM, Lysell G, Friberg U. Unilateral hyperplasia of the mandibular condylar process. A histological, microradiographic, and autoradiographic examination of one case. Acta Odontol Scand. 1962;20:485-504. [PubMed ID: 13939358].
-
11.
Slootweg PJ, Muller H. Condylar hyperplasia. A clinico-pathological analysis of 22 cases. J Maxillofac Surg. 1986;14(4):209-14. [PubMed ID: 3461098].
-
12.
Obwegeser HL, Makek MS. Hemimandibular hyperplasia--hemimandibular elongation. J Maxillofac Surg. 1986;14(4):183-208. [PubMed ID: 3461097].
-
13.
Mehrotra D, Dhasmana S, Kamboj M, Gambhir G. Condylar hyperplasia and facial asymmetry: report of five cases. J Maxillofac Oral Surg. 2011;10(1):50-6. [PubMed ID: 22379321]. https://doi.org/10.1007/s12663-010-0141-5.
-
14.
Munoz MF, Monje F, Goizueta C, Rodriguez-Campo F. Active condylar hyperplasia treated by high condylectomy: report of case. J Oral Maxillofac Surg. 1999;57(12):1455-9. [PubMed ID: 10596668].
-
15.
Wolford LM, Lebanc J. Condylectomy to arrest disproportionate mandibular growth. In Proceedings of the American Cleft Palate Association Annual Meeting. 1986:16-9.
-
16.
Brusati R, Pedrazzoli M, Colletti G. Functional results after condylectomy in active laterognathia. J Craniomaxillofac Surg. 2010;38(3):179-84. [PubMed ID: 19501516]. https://doi.org/10.1016/j.jcms.2009.04.010.