Abstract
Background:
Mentalization-based treatment (MBT) and dialectical behavioral therapy (DBT) are two treatments with a strong theoretical basis for borderline personality disorder (BPD).Objectives:
We investigated the structures that influence the process of symptom recovery from the perspective of mentalization-based treatment.Methods:
This is a single-blind randomized controlled clinical trial conducted on 60 patients diagnosed with BPD. Data were collected from March 2017 to June 2017 by a psychiatrist in a semi-structured clinical interview. The participants were categorized into intervention and control groups. Before, immediately and two months after the group therapy based on MBT and DBT, the participants were assessed with Revised Adult Attachment Scale (RAAS), Reflective Function Questionnaire for Adult (RFQA), Eye Test-Test Revised Version, Beck Anxiety Inventory (BAI), and Beck Depression Inventory-II (BDI-II).Results:
Both of the treatments were effective in improving avoidant (P = 0.0001) and ambivalent (P = 0.0001) attachment styles, mentalization (P = 0.0001), and social cognition (P = 0.0001). These changes persisted from post-test to follow-up in mentalization (P = 0.003) and social cognition (P = 0.02).Conclusions:
Although both methods are effective in improving the symptoms of the disorder, MBT is more effective in improving the basic structures of the BPD. This may lead to greater stability in the treatment.Keywords
Borderline Personality Disorder Attachment Style Mentalization Social Cognition
1. Background
Borderline personality disorder (BPD) was recognized in the 1960s (1). The DSM-V diagnostic criteria only require individuals to have five out of nine symptoms (2). It is a common clinical disorder among clinical disorders (3, 4). The prevalence of this disorder is from 0.5 to 7.2% in the general population, 9.3 to 22% among psychiatric outpatients, and 28% in hospitalized patients (5).
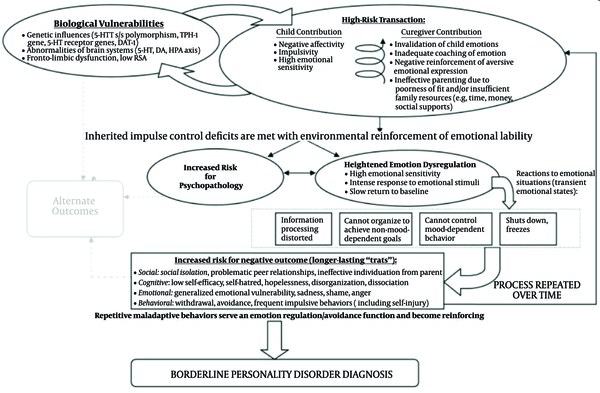
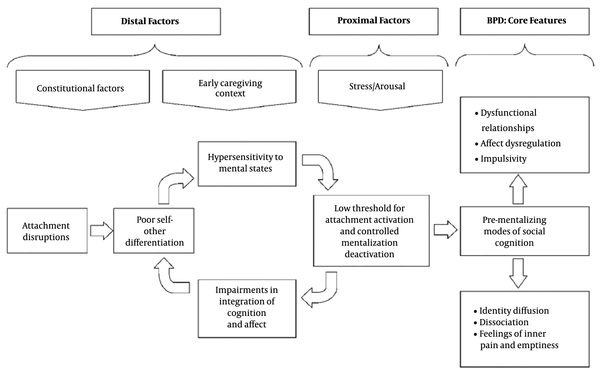
Dialectical behavior therapy (DBT) and mentalization-based treatment (MBT) are two treatments for BPD (6). One of the important theories that explain BPD is the biosocial developmental model (Linehan, 1995) -the basis of DBT- (Figure 1) (7), and the newer theory proposed is the mentalization-based theory as the basis of MBT (Figure 2) (8). Insecure attachment style in BPD leads to impaired mentalization and social cognition. Improving these three domains in the psychotherapy process can help recover the symptoms of the disorder (9).
Psychopathological dialectical behavior Therapy-based model of borderline personality disorder (Crowell, Beauchaine, Linehan, 2009).
Psychopathological mentalization-based model of borderline personality disorder (Fonagy, Luyten, 2009).
Research evidence in this area is limited. attachment styles (10-12). and reflective function (10, 13) are improved as a result of transference-focused psychotherapy (TFP) during treatment (10), short-term dynamic psychotherapy (13, 14), and successful individual psychotherapy and group psychotherapy (11).The result of studies indicated that DBT (15) and TFP (16) increased in reflective function. The results of the studies revealed that DBT, systems training for emotional predictability, problem-solving were effective (17) and DBT and TFP in improving social cognition (18).
Most of the efficacy of therapies on the improvement of symptoms of BPD has been studied. Some scientists have considered DBT and MBT as two treatments of different origins, each of which works in a different way to improve BPD.
2. Objectives
Most studies have focused on the effectiveness of therapeutic approaches, but in this study, we investigated the structures that influence the process of symptom recovery from the perspective of mentalization-based treatment.
3. Methods
The research design was a single-blind randomized controlled clinical trial. This study was conducted on 60 patients diagnosed with BPD by a psychiatrist. They were examined by a semi-structured clinical interview. Data were collected from March 2017 to June 2017. All screening and performance procedures were performed daily in a hospital in Shiraz. Patients were selected by the targeted sampling method according to inclusion criteria.
The inclusion criteria were 1) being in the age range of 18 to 27, 2) having at least diploma education, and 3) being diagnosed with BPD by a psychiatric. The exclusion criteria included 1) not being primarily diagnosed with disease except for BPD, 2) being dependent on a substance (but not substance abuse), 3) receiving any other psychotherapy treatment, and 4) being admitted to psychiatric wards during treatment. Study information was given to patients, and they signed an informed consent form before participating in the study. They received assurances that their data would be kept confidential and withdrawal from the study at any time would not influence their treatment process.
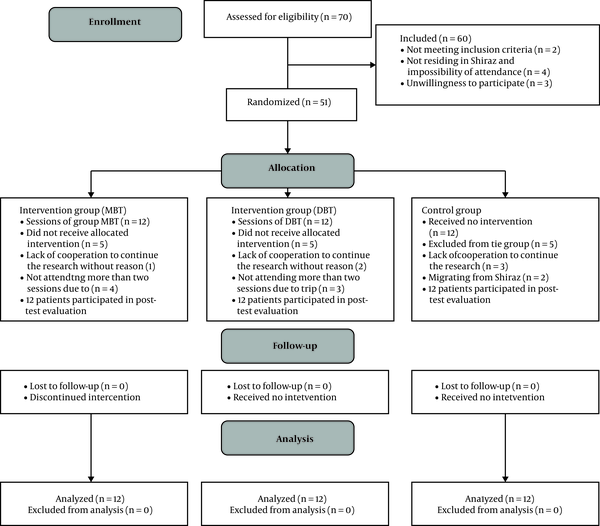
The intervention group received group therapy based on MBT and DBT, while the control group received no intervention. The sample size was determined as 36 (12 individuals per group) (Figure 3). To increase the accuracy of the study, the sample size was considered 12, which was calculated based on the iteration method and research conducted by Sinnaeve et al. (2018) (19).
Consort flowchart of the study population, MBT: mentalization based treatment DBT: dialectical behavior therapy.
3.1. Instrumentation
1- Demographic checklist on age, education level, marital status, and the type and dose of drugs.
2- Revised Adult Attachment Scale (RAAS): Adult Attachment Scale created by Collins and Reid (1990) and revised by Reid (1996). This scale has three subscales that are secure, avoidant, and ambivalent attachment styles. The internal consistency of Cronbach's alpha method in the original version was 0.75, 0.72, and 0.69, respectively. The correlation of each item with the corresponding factor was at the desired level (20). The reliability of the Persian version with the one-month test-retest method for secure, avoidant, and ambivalent attachment style was 0.81, 0.78, and 0.85, respectively (21). In the present study, the internal consistency of Cronbach's alpha method, insecure, avoidant, and ambivalent attachment styles was 0.72, 0.71, and 0.79, respectively.
3- Reflective Function Questionnaire for Adult (RFQA): The Reflective Function Questionnaire is a 54-item self-report questionnaire designed to measure. The internal consistency was reported to be 0.77 using Cronbach's alpha method for the overall score. The correlation of each item with the total score for the whole scale (r = 0.29, P ≤ 0.001) was at the desired level (22). This questionnaire was translated and validated in this study. The reliability of this scale was also examined through internal consistency, with Cronbach’s alpha, which was significant (α = 0.71). Confirmatory factor analyses used for assessing validity supported the one-dimensional model (RMSEA = 0.07).
4- Eye Test-Test Revised Version: It consists of 36 different states of artists’ eyes region developed to measure social cognition in adults. The respondent should choose the option out of 4 options that best describes the mental state. Test-retest reliability was significant (r = 0.68, P ≤ 0.001). To evaluate the validity, correlation with social skill was used (r = 0.43, P ≤ 0.001) (23). In the Persian version, the reliability using Cronbach’s alpha was significant (α = 0.72). To evaluate the validity, correlation with social skill was used (r = 0.27, P ≤ 0.001) (24). In this study, Cronbach's alpha was 0.72.
5- Beck Anxiety Inventory (BAI): The BAI is a self-report assessment of anxiety symptoms and consists of 21 items. It was developed by Beck et al. (1988) (25). This inventory was translated and validated by Kaviani H, Mousavi (2008). In the Persian version, the internal consistency of Cronbach's alpha was 0.92, and its validity was appropriate (r = 0.72, P < 0.001) (26). In this study, Cronbach's alpha was 0.87.
6- Beck Depression Inventory-II (BDI-II): The BDI-II is a self-report depression scale developed by Beck AT et al. (1996) to measure different aspects of depression. The BDI-II consists of 21 items. The internal consistency of Cronbach's alpha was 0.92 in outpatients. Also, there was a significant correlation between the BDI score and BAI (r = -0.60, P < 0.01) (27). This inventory was translated and validated by Rahimi (2014). In the Persian version, the internal consistency of Cronbach's alpha was 0.87, and convergent validity with the general health questionnaire (GHQ) was 0.73 (28). In this study, Cronbach's alpha was 0.89.
The session of the DBT was in accordance with the Linehan’s guidelines (1993) (29) and MBT sessions relayed on Bateman, Fonagy's (2006) instruction (30). We used ANCOVA to compare the effectiveness of the intervention in the experimental groups with the controls. All statistical analyses were performed with the SPSS version 16 software. The significance level was P < 0.05.
4. Results
All of the participants were diagnosed with BPD and were residing in Shiraz. The age range of the subjects was between 18 and 27 years old. The results of ANOVA test revealed that the groups had no significant difference in terms of dose of the drugs (topiramate: F = 0.60, P = 0.55; lithium: F = 0.56, P = 0.57; gabapentin: F = 0.11, P = 0.89; lamotrigine: F = 0.05, P = 0.94; welbutrin: F = 0.07, P = 0.92; alprazolam: F = 0.02, P = 0.97; propranolol: F = 0.63, P = 0.53). Data analysis revealed that the groups had no significant difference in demographic variables (Table 1) and BAI (F = 0.003, P = 0.9), and BDI-II (F = 0.43, P = 0.6).
Descriptive Characteristics
| Variable | MBT Group | DBT Group | Control Group | P-Value |
|---|---|---|---|---|
| Age (y), mean ± SD | 23.75 ± 2.22 | 22.08 ± 2.15 | 22.00 ± 2.52 | 0.1 |
| Sex, No. (%) | 0.7 | |||
| Male | 5 (41.66) | 3 (25) | 3 (25) | |
| Female | 7 (33.58) | 9 (75) | 9 (75) | |
| Marriage, No. (%) | 0.6 | |||
| Single | 9 (75) | 10 (83.33) | 10 (83.33) | |
| Married | 2 (16.66) | 0 (0) | 1 (8.33) | |
| Divorced | 1 (8.33) | 2 (16.66) | 1 (8.33) | |
| Education, No. (%) | 0.08 | |||
| Diploma | 0 (0) | 1 (8.33) | 4 (33.33) | |
| Bachelor | 9 (75) | 8 (66.66) | 7 (58.33) | |
| Master | 3 (25) | 3 (25) | 1 (8.33) |
The mean and standard deviation of the research variables are observable at different stages (Table 2).
Mean and Standard Deviation of MBT and DBT
| Variable | Pre-test, Mean ± SD | Posttest , Mean ± SD | Follow-up, Mean ± SD |
|---|---|---|---|
| Secure attachment | |||
| MBT | 18.50 ± 4.60 | 19.33 ± 1.49 | 21.25 ± 6.95 |
| DBT | 19.33 ± 3.79 | 19.25 ± 2.80 | 19.25 ± 2.56 |
| Control | 21.58 ± 3.87 | 18.41 ± 3.17 | 17.91 ± 2.57 |
| Avoidant attachment | |||
| MBT | 18.58 ± 2.27 | 10.66 ± 1.61 | 16.33 ± 1.92 |
| DBT | 17.50 ± 3.45 | 15.91 ± 2.87 | 18.66 ± 2.18 |
| Control | 17.75 ± 3.74 | 19.66 ± 2.10 | 18.58 ± 2.15 |
| Ambivalent attachment | |||
| MBT | 21.75 ± 4.95 | 17.16 ± 3.32 | 19.75 ± 4.15 |
| DBT | 22.41 ± 3.72 | 21.50 ± 2.50 | 22.50 ± 3.00 |
| Control | 20.41 ± 4.81 | 20.25 ± 4.55 | 20.50 ± 4.16 |
| Mentalization | |||
| MBT | 152.91 ± 44.05 | 96.58 ± 25.12 | 102.25 ± 21.80 |
| DBT | 137.66 ± 35.23 | 125.25 ± 35.91 | 138.16 ± 35.99 |
| Control | 142.41 ± 46.20 | 145.41 ± 42.10 | 167.16 ± 36.14 |
| Social cognition | |||
| MBT | 20.83 ± 3.37 | 22.91 ± 3.17 | 22.66 ± 2.87 |
| DBT | 18.91 ± 3.87 | 19.58 ± 2.99 | 19.41 ± 2.57 |
| Control | 19.41 ± 3.89 | 18.58 ± 3.70 | 17.75 ± 2.66 |
ANCOVA analysis revealed significant differences between the groups in terms of avoidant and ambivalent attachments, mentalization, and social cognition in the post-test. Just insecure attachment, the difference was not significant. Changes in mentalization and social cognition were stable from the post-test to follow-up. Also, changes in avoidant and ambivalent attachments, mentalization, and social cognition were significant from the pre-test to follow-up (Table 3).
Comparison of Variables Among the Groups by ANOVA
| Variable | Group | P-Value, (Pretest vs Posttest) | P-Value, (Pretest vs Follow-up) | P-Value, (Posttest vs Follow-up) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | P | eta | F | P | eta | F | P | eta | ||
| Secure attachment | MBT | 0.45 | 0.6 | 0.03 | - | - | - | - | - | - |
| DBT | ||||||||||
| Control | ||||||||||
| Avoidant attachment | MBT | 44.05 | 0.0001 | 0.74 | 5.41 | 0.01 | 0.25 | 1.15 | 0.3 | 0.06 |
| DBT | ||||||||||
| Control | ||||||||||
| Ambivalent attachment | MBT | 31.38 | 0.0001 | 0.67 | 11.71 | 0.0001 | 0.43 | 0.75 | 0.4 | 0.04 |
| DBT | ||||||||||
| Control | ||||||||||
| Mentalization | MBT | 35.86 | 0.0001 | 0.69 | 56.13 | 0.0001 | 0.77 | 7.14 | 0.003 | 0.30 |
| DBT | ||||||||||
| Control | ||||||||||
| Social cognition | MBT | 14.93 | 0.0001 | 0.48 | 176.22 | 0.0001 | 0.71 | 4.35 | 0.02 | 0.21 |
| DBT | ||||||||||
| Control | ||||||||||
Post hoc results demonstrated that DBT was effective in improving avoidant and ambivalent attachment styles, mentalization, and social cognition, but MBT was more effective. Improvement in avoidant and ambivalent attachment styles was not stable from the post-test to follow-up. MBT made more changes than DBT from the pre-test to follow-up in both. MBT showed more changes from the pre-test to follow-up, and improvement was more stable than DBT in mentalization and social cognition (Table 4).
Post-hoc Analysis for Mean Changes in the Post-test and Follow-up
| Variable | Post-test vs Pre-test | Pre-test vs Follow-up | Post-test vs Follow-up | |||
|---|---|---|---|---|---|---|
| Mean Difference | P-Value | Mean Difference | P-Value | Mean Difference | P-Value | |
| Avoidant attachment | ||||||
| MBT | ||||||
| DBT | -5.49 | 0.0001 | -2.45 | 0.008 | - | - |
| Control | -9.15 | 0.0001 | -2.46 | 0.008 | - | - |
| DBT | ||||||
| MBT | 5.49 | 0.0001 | 2.45 | 0.008 | - | - |
| Control | -3.66 | 0.001 | -0.003 | 0.9 | - | - |
| Control | ||||||
| MBT | 9.15 | 0.0001 | 2.46 | 0.008 | - | - |
| DBT | 3.66 | 0.001 | 0.003 | 0.9 | - | - |
| Ambivalent attachment | ||||||
| MBT | ||||||
| DBT | -3.18 | 0.0001 | -2.09 | 0.0001 | - | - |
| Control | -4.10 | 0.0001 | -1.75 | 0.001 | - | - |
| DBT | ||||||
| MBT | 3.81 | 0.0001 | 2.09 | 0.0001 | - | - |
| Control | -0.29 | 0.6 | 0.34 | 0.4 | - | - |
| Control | ||||||
| MBT | 4.10 | 0.0001 | 1.75 | 0.001 | - | - |
| DBT | 0.29 | 0.6 | -0.34 | 0.4 | - | - |
| Mentalization | ||||||
| MBT | ||||||
| DBT | -39.90 | 0.0001 | -45.87 | 0.0001 | -12.16 | 0.04 |
| Control | -56.56 | 0.0001 | -71.77 | 0.0001 | -24.45 | 0.001 |
| DBT | ||||||
| MBT | 39.90 | 0.0001 | 45.87 | 0.0001 | 12.16 | 0.04 |
| Control | -16.66 | 0.02 | -25.89 | 0.001 | -12.29 | 0.04 |
| Control | ||||||
| MBT | 56.56 | 0.0001 | 71.77 | 0.0001 | 24.45 | 0.001 |
| DBT | 16.66 | 0.02 | 25.89 | 0.001 | 12.29 | 0.04 |
| Social cognition | ||||||
| MBT | ||||||
| DBT | 1.79 | 0.005 | 1.96 | 0.0001 | 0.85 | 0.1 |
| Control | 3.19 | 0.0001 | 3.96 | 0.0001 | 1.80 | 0.006 |
| DBT | ||||||
| MBT | -1.79 | 0.005 | -1.96 | 0.0001 | -0.85 | 0.1 |
| Control | 1.40 | 0.02 | 2.00 | 0.0001 | 0.94 | 0.08 |
| Control | ||||||
| MBT | -3.19 | 0.0001 | -3.96 | 0.0001 | -1.80 | 0.006 |
| DBT | -1.40 | 0.02 | -2.00 | 0.0001 | -0.94 | 0.08 |
5. Discussion
The results indicated that the two treatments were effective in improving avoidant and ambivalent attachment styles, mentalization, and social cognition. These changes were stable to follow-up in mentalization and social cognition. They led to positive changes in these variables from pre-test to follow-up.
Changes in attachment style can be a consequence and goal of treatment. Research findings suggest that focusing on the relationship between the therapist and patient and/or the use of interpretation, especially in patients with personality disorders, may be a mechanism for altering the attachment structure. A range of treatments, such as MBT and DBT, may also be effective in achieving changes in the attachment style (31).
During the process of MBT or any effective treatment that improves reflective function, secure attachment can be formed; as a consequence, the mentalization capacity increases (32). Psychotherapy, regardless of the type of treatment and disorder, potentially provides an interactive platform for creating attachment in which individuals understand each other. Thinking about feelings, thoughts, and beliefs in an acceptable setting leads to resolved conflicts in mind and an improvement in the attachment style (33).
Attachment to the group can, in turn, change the patients' attachment styles.34 Indeed, one of the ways that facilitate the process of change, especially in group therapy, is the formation of an attachment during the treatment process (34, 35).
Reflective function results from the process of development, allowing the child to respond not only to the behavior of others, but also to an understanding of beliefs, feelings, desires, manifestations, plans, and so on. This improvement can occur in the treatment process. Establishing a secure attachment relationship between the therapist and patients increases the awareness of mental status (36).
During the treatment process, the patient's reflective function increases at two levels. The first level is the ability to experience and reflect on what the person is feeling at the moment. The higher level is understanding the mental states of oneself and others in a general context and the relationship between oneself and others. This level of ability indicates the creation of an integrated sense of self and others. This level of reflexive function is achieved when the therapist proceeds from the stage of clarifying the patient's perceptions of himself and others at the moment to confronting the patient with their conflicts between different mental statuses and interpreting their reasons (10).
Overmentalization through emotional dysregulation and impulsiveness affects interpersonal relationships. Therefore, focusing on emotion regulation and mentalization can be effective in improving interpersonal problems. DBT focuses on emotion regulation, and MBT can directly play an effective role in improving interpersonal problems in patients with BPD by improving their mental status (37).
Given the role of emotion regulation and impulsiveness in social cognitive impairment, interventions designed to improve emotion control, such as DBT and Systems Training for Emotional Predictability and Problem Solving can be effective in improving social cognition (38). When a secure attachment has been established, confronting with feelings, thoughts, and beliefs helps to correct the contradictions in one's mind, and this leads to an improvement in one's cognition and social cognition in relationships. This factor is seen in MBT (33). The persistence of psychological pathology in BPD results from a pervasive limitation in assessing stressful social situations, which can be due to limitations in the capacity of mentalization. Improving reflective function can also increase social cognition (39).
There are some limitations in the present study that might have affected our findings. First of all, the demographic characteristics except for age were disregarded in selecting the cases. Secondly, the gender of subjects was not considered in the analysis. Thirdly, the number of cases was small, so caution should be taken when generalizing the results. Future studies could assess the contributions of potential variables of the effectiveness of MBT and DBT, such as comorbid Axis-I disorders, BPD severity, gender, and treatment adherence. Identification of the underlying mechanisms of the therapy and whether it works as a result of its rationale are suggested to be considered in future researches to improve the functioning. MBT can be used in adolescent groups exposed to the risk of BPD.
5.1. Conclusion
MBT and DBT, as two effective methods of treating BPD, are also effective in improving attachment styles, mentalization, and social cognition. However, the changes caused by MBT were more stable.
References
-
1.
Stoffers-Winterling JM, Storebo OJ, Vollm BA, Mattivi JT, Nielsen SS, Kielsholm ML, et al. Pharmacological interventions for people with borderline personality disorder. Cochrane Database Syst Rev. 2018. [PubMed Central ID: PMC6491315]. https://doi.org/10.1002/14651858.Cd012956.
-
2.
Hutsebaut J, Debbane M, Sharp C. Designing a range of mentalizing interventions for young people using a clinical staging approach to borderline pathology. Borderline Personal Disord Emot Dysregul. 2020;7:6. [PubMed ID: 32190330]. [PubMed Central ID: PMC7068993]. https://doi.org/10.1186/s40479-020-0121-4.
-
3.
Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. The Lancet. 2011;377(9759):74-84. https://doi.org/10.1016/s0140-6736(10)61422-5.
-
4.
Soeteman DI, Verheul R, Busschbach JJ. The burden of disease in personality disorders: diagnosis-specific quality of life. J Pers Disord. 2008;22(3):259-68. [PubMed ID: 18540798]. https://doi.org/10.1521/pedi.2008.22.3.259.
-
5.
Korzekwa MI, Dell PF, Links PS, Thabane L, Webb SP. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr Psychiatry. 2008;49(4):380-6. [PubMed ID: 18555059]. https://doi.org/10.1016/j.comppsych.2008.01.007.
-
6.
Swenson CR, Choi-Kain LW. Mentalization and dialectical behavior therapy. Am J Psychother. 2015;69(2):199-217. [PubMed ID: 26160623]. https://doi.org/10.1176/appi.psychotherapy.2015.69.2.199.
-
7.
Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan's theory. Psychol Bull. 2009;135(3):495-510. [PubMed ID: 19379027]. [PubMed Central ID: PMC2696274]. https://doi.org/10.1037/a0015616.
-
8.
Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Dev Psychopathol. 2009;21(4):1355-81. [PubMed ID: 19825272]. https://doi.org/10.1017/S0954579409990198.
-
9.
Khabir L. Group therapy based on mentalization and dialectical behavior on attachment styles, mentalization, social cognition, and clinical symptoms in patients with borderline personality disorder. Shiraz, Iran: Shiraz University; 2019. Available from: https://en.irct.ir/trial/39064.
-
10.
Levy KN, Meehan KB, Kelly KM, Reynoso JS, Weber M, Clarkin JF, et al. Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. J Consult Clin Psychol. 2006;74(6):1027-40. [PubMed ID: 17154733]. https://doi.org/10.1037/0022-006X.74.6.1027.
-
11.
Kinley JL, Reyno SM. Attachment style changes following intensive short-term group psychotherapy. Int J Group Psychother. 2013;63(1):53-75. [PubMed ID: 23252815]. https://doi.org/10.1521/ijgp.2013.63.1.53.
-
12.
Lilliengren P, Falkenstrom F, Sandell R, Mothander PR, Werbart A. Secure attachment to therapist, alliance, and outcome in psychoanalytic psychotherapy with young adults. J Couns Psychol. 2015;62(1):1-13. [PubMed ID: 25222907]. https://doi.org/10.1037/cou0000044.
-
13.
Khademi M, Hajiahmadi M, Faramarzi M. The role of long-term psychodynamic psychotherapy in improving attachment patterns, defense styles, and alexithymia in patients with depressive/anxiety disorders. Trends Psychiatry Psychother. 2019;41(1):43-50. [PubMed ID: 30994785]. https://doi.org/10.1590/2237-6089-2017-0144.
-
14.
Travis LA, Bliwise NG, Binder JL, Horne-Moyer H. Changes in clients' attachment styles over the course of time-limited dynamic psychotherapy. Psychotherapy. 2001;38(2):149-59. https://doi.org/10.1037/0033-3204.38.2.149.
-
15.
Fischer-Kern M, Doering S, Taubner S, Horz S, Zimmermann J, Rentrop M, et al. Transference-focused psychotherapy for borderline personality disorder: change in reflective function. Br J Psychiatry. 2015;207(2):173-4. [PubMed ID: 25999334]. https://doi.org/10.1192/bjp.bp.113.143842.
-
16.
Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry. 2007;164(6):922-8. [PubMed ID: 17541052]. https://doi.org/10.1176/ajp.2007.164.6.922.
-
17.
Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: A randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165(4):468-78. [PubMed ID: 18281407]. [PubMed Central ID: PMC3608469]. https://doi.org/10.1176/appi.ajp.2007.07071079.
-
18.
de Groot ER, Verheul R, Trijsburg RW. An integrative perspective on psychotherapeutic treatments for borderline personality disorder. J Pers Disord. 2008;22(4):332-52. [PubMed ID: 18684048]. https://doi.org/10.1521/pedi.2008.22.4.332.
-
19.
Sinnaeve R, van den Bosch LMC, Hakkaart-van Roijen L, Vansteelandt K. Effectiveness of step-down versus outpatient dialectical behaviour therapy for patients with severe levels of borderline personality disorder: a pragmatic randomized controlled trial. Borderline Personal Disord Emot Dysregul. 2018;5:12. [PubMed ID: 30002832]. [PubMed Central ID: PMC6040072]. https://doi.org/10.1186/s40479-018-0089-5.
-
20.
Teixeira RCR, Ferreira JHBP, Howat-Rodrigues ABC. Collins and read revised adult attachment scale (RAAS) validity evidences. Psico. 2019;50(2). https://doi.org/10.15448/1980-8623.2019.2.29567.
-
21.
Saaidian Asl M, Khanzadeh M, Hasani J, Edrisi F. Factor structure and psychometric properties of the persian version of state adult attachment scale (SAAS). J Res Psychol Health. 2012;6(1):66-78.
-
22.
Fonagy P, Luyten P, Moulton-Perkins A, Lee YW, Warren F, Howard S, et al. Development and validation of a self-report measure of mentalizing: The reflective functioning questionnaire. PLos One. 2016;11(7). e0158678. [PubMed ID: 27392018]. [PubMed Central ID: PMC4938585]. https://doi.org/10.1371/journal.pone.0158678.
-
23.
Baron‐Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The “reading the mind in the eyes” test revised version: A study with normal adults, and adults with asperger syndrome or high‐functioning autism. J Child Psychol Psychiatry. 2003;42(2):241-51. https://doi.org/10.1111/1469-7610.00715.
-
24.
Nejati V, Zabihzadeh A, Maleki G, Tehranchi A. Mind reading and mindfulness deficits in patients with major depression disorder. Procedia Soc Behav Sci. 2012;32:431-7. https://doi.org/10.1016/j.sbspro.2012.01.065.
-
25.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893-7. [PubMed ID: 3204199]. https://doi.org/10.1037//0022-006x.56.6.893.
-
26.
Kaviani H, Mousavi AS. Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI). Tehran Univ Med J. 2008;65(2):136-40.
-
27.
Beck AT, Steer RA, Brown G. Manual for the beck depression inventory-II. San Antonio, TX, USA: Psychological Corporation; 1996. Available from: https://www.brown.edu/academics/public-health/research/mens-health-initiative/bdiii.
-
28.
Rahimi C. Application of the beck depression inventory-II in Iranian university students. CPAP. 2014;2(10):173-88.
-
29.
Linehan MM. Skills training manual for treating borderline personality disorder. New York, USA: Guilford Press; 1993.
-
30.
Bateman A, Fonagy P. Mentalization-based treatment for personality disorders: A practical guide. Oxford, England: Oxford University Press; 2016. https://doi.org/10.1093/med:psych/9780199680375.001.0001.
-
31.
Levy KN, Ellison WD, Scott LN, Bernecker SL. Attachment style. J Clin Psychol. 2011;67(2):193-203. [PubMed ID: 21108315]. https://doi.org/10.1002/jclp.20756.
-
32.
De Oliveira C, Rahioui H, Smadja M, Gorsane MA, Louppe F. [Mentalization based treatment and borderline personality disorder]. Encephale. 2017;43(4):340-5. [PubMed ID: 27431343]. https://doi.org/10.1016/j.encep.2016.02.020.
-
33.
Fonagy P, Bateman AW. Mentalizing and borderline personality disorder. J Ment Health. 2009;16(1):83-101. https://doi.org/10.1080/09638230601182045.
-
34.
Marmarosh CL. Empirical research on attachment in group psychotherapy: moving the field forward. Psychotherapy (Chic). 2014;51(1):88-92. [PubMed ID: 24059737]. https://doi.org/10.1037/a0032523.
-
35.
Masin-Moyer M, Engstrom M, Solomon P. A comparative effectiveness study of a shortened trauma recovery empowerment model and an attachment-informed adaptation. Violence Against Women. 2020;26(5):482-504. [PubMed ID: 30943122]. https://doi.org/10.1177/1077801219836730.
-
36.
Cologon J, Schweitzer RD, King R, Nolte T. Therapist reflective functioning, therapist attachment style and therapist effectiveness. Adm Policy Ment Health. 2017;44(5):614-25. [PubMed ID: 28132188]. https://doi.org/10.1007/s10488-017-0790-5.
-
37.
Euler S, Nolte T, Constantinou M, Griem J, Montague P, Fonagy P. Interpersonal problems in borderline personality disorder: Associations with mentalizing, emotion regulation, and impulsiveness. J Pers Disord. 2019:1-17. https://doi.org/10.1521/pedi_2019_33_427.
-
38.
Roepke S, Vater A, Preissler S, Heekeren HR, Dziobek I. Social cognition in borderline personality disorder. Front Neurosci. 2012;6:195. [PubMed ID: 23335877]. [PubMed Central ID: PMC3543980]. https://doi.org/10.3389/fnins.2012.00195.
-
39.
Kalisch R, Muller MB, Tuscher O. A conceptual framework for the neurobiological study of resilience. Behav Brain Sci. 2015;38. e92. [PubMed ID: 25158686]. https://doi.org/10.1017/S0140525X1400082X.
