Abstract
Objectives:
The current study tries to assess the causative factors of dysphagia and omit them to find the exact contribution of TEE for this symptom among patients who suffer from elective open cardiac surgery in different age ranges in both sexes.Methods:
In this observational study, 100 patients between 30-80 years of age with ASA < III and EF > 40% who were candidate for elective open cardiac surgery in a referral hospital in Tehran in 2011 were recruited. The patients were divided into two groups based on TEE performance; patients who needed to perform TEE based on medical indication were considered the case group and the other patients who did not have indication for TEE, formed the control group.Results:
Total frequency of dysphagia was 13% in all patients disregarding TEE performance while 6 (12%) and 7 (14%) of controls and cases showed this symptom respectively. Odynophagia was the other symptom to be assessed for its frequency in this study and showed 13% total frequency considering all participants disregarding the groups. This symptom was reported exactly similar to dysphagia which was 6 (12%) in controls and 7 (14%) in cases. The participants’ gender was not effective on the distribution of dysphagia where 6 (11.3%) females and 7 (14.9%) males were involved with no significant difference.Conclusions:
Intraoperative trans-esophageal echocardiography during cardiac surgeries has greater usefulness than complications and is worth using in this case as well.Keywords
Transesophageal Echocardiography Open Cardiac Surgery Dysphagia Odynophagia
1. Background
Several techniques of patient monitoring are already used during open cardiac surgeries among which trans-esophageal echocardiography (TEE) is probably the most important one which is growing to be more attractive over the world. TEE is mainly an intraoperative diagnostic tool to facilitate the procedure as well as on time complication detection. Most applications for TEE are monitoring of myocardial ischemia, valve repair or replacement, congenital cardiac disorders or defects, aortic dissection, cardiac tumors or other several conditions (1). Like other invasive procedures, this diagnostic technique may have complications that would be chiefly oral and dental trauma, laryngeal dysfunction, compression on the aorta or bronchi in children, upper GI bleeding, esophageal penetration, dysphagia and odynophagia (2, 3). The mentioned complications usually increase in cardiac surgery due to cardiopulmonary bypass, hemodynamic instability, hypothermia, and longer time of TEE use (4, 5). Dysphagia has been raised as an increasing complication globally due to wide TEE usage during operations and this technique is usually blamed as an independent risk factor for dysphagia (6). Dysphagia is actuallan important complication which is also effective on hospital stay and consequent costs and morbidities (7).
TEE is not the only cause of dysphagia and it is occasionally needed to determine other causes like the procedure of intubation and define an incidence of dysphagia directly due to TEE in order to control the predisposing factors in the future. A study by Rousou et al. showed 7.8 times more frequency of dysphagia when TEE was used compared with operations without TEE (5). TEE was also introduced as an independent factor of odynophagia resulting in swalloing disorders, especially in elderly individuals (8). Cardiac surgeries have been reported to have the risk of dysphagia up to 18% in some trials when TEE was used (6). This prevalence is obviously lower than what Chin et al. claimed (> 60%) through their work. They reported 28.6% incidence of dysphagia if TEE probe was off after the primary echocardiography but was replaced at the end of operation (9).
The current study tries to assess the causative factors of dysphagia and omit them to find the exact contribution of TEE for this symptom among patients who suffer from elective open cardiac surgery in different age ranges in both sexes.
2. Methods
In this observational study, 100 patients between 30 - 80 years of age with ASA < III and EF > 40% who were candidate for elective open cardiac-surgery in a referral hospital in Tehran in 2011 were recruited. Patients with a history of dysphagia, tracheal pressure more than 25 mmHg, people who have experienced multiple attempts for tracheal intubation or TEE placement in addition to addicts and diabetics as well as individuals who were intubated for > 12 hours were removed from the study selection considering the exclusion criteria. The patients were divided into two groups based on TEE performance, patients who need to perform TEE based on medical indication were considered case group and the other patients who did not have indication for TEE, formed the control group. The colleagues who gathered the data were perfectly trained. When the operation finished and the patients were transferred to ICU, they were extubated before their condition and complaints for dysphagia were assessed after 24 hours of operation.
This study was approved by our local ethic committee according to the Helsinki Declaration of the world medical association (2000).
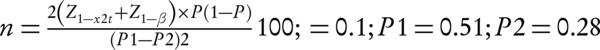
Statistics: demographics, surgical and TEE information, symptoms and outcomes were based on the considered variables entered in SPSS 21 for Windows, and were analyzed by t-test and Chi-square whenever needed. Central tendency indices were reported and compared using t-test and the frequencies in addition to qualitative analysis were done by Chi-square test. Considering the study power of 0.8, CI = 95% and α = 0.05, the sample size was calculated by the following formula:
3. Results
This study recruited 100 patients including 50 cases who performed TEE and 50 controls without TEE placement. The mean age for patients was 49.18 ± 16.48 totally with a range of 14 - 79 years.
The mean age was one year more in controls though there was no significant difference between the groups in terms of age (P value = 0.886). Females made up the majority of the participants (53%) including 26 controls and 27 cases with no sexual differences between the studied groups. Table 1 shows the basic information for participants regarding their groups.
| Exposed to TEE | Unexposed to TEE | P Value | ||
|---|---|---|---|---|
| Sex | Male | 23 (46) | 24 (48) | 0.500 |
| Female | 27 (54) | 26 (52) | ||
| Age | 48.63 ± 16.14 | 49.73 ± 16.96 | 0.886 | |
| Operation time, min | 482.7 ± 59.59 | 480 ± 62.03 | 0.537 |
Total frequency of dysphagia was 13% in all patients disregarding the performance of TEE while 6 (12%) and 7 (14%) from controls and cases showed the symptom, respectively. As the significance is shown in Table 2, there was no difference in the groups for the frequency of dysphagia after the tests. (P value = 0.50). Odynophagia was the other symptom to be assessed for its frequency in this study and showed 13% total frequency considering all patients disregarding the groups. This symptom was reported exactly similar to dysphagia that was 6 (12%) in controls and 7 (14%) in cases. The participants’ gender was not effective on the distribution of dysphagia where 6 (11.3%) females and 7 (14.9%) males were involved with no significant difference (P value = 0.41).
Distribution of the Consequences in Both Groups
| Exposed to TEE | Unexposed to TEE | P Value | Male | Female | P Value | |
|---|---|---|---|---|---|---|
| Dysphagia | 7 (14) | 6 (12) | 0.500 | 7 (14.9) | 6 (11.3) | 0.407 |
| Odynophagia | 7 (14) | 6 (12) | 0.500 | 7 (14.9) | 6 (11.3) | 0.407 |
4. Discussion
Our study showed no more esophageal complications by TEE compared to regular surgeries without TEE. TEE is not very invasive when compared with other diagnostic modalities in this field. Insertion and manipulation of the ultrasound probe may result in oropharyngeal, esophageal and gastric trauma (10, 11). Lennon et al. published a study in 2005 through which major upper GI complications were monitored after cardiac surgery for 30 days to assess the role of TEE in this matter. They suggested that GI complications were totally higher in TEE users than patients without TEE insertion (1.2% vs. 0.29%) (12). Forty one patients were recruited by a team led by Hulyalkar during the 1990's who underwent cardiac surgery and were assessed for bleeding or symptoms like dysphagia, anorexia or sore throat. Similar to the current study, they found no other risk of mentioned problems in patients who used TEE (13). Later in 2009, a report was introduced by Piercy et al. that showed 6 TEE complications in a 2-year period of time to suggest more frequent TEE complications in elderly patients (> 70 years of age) with a relative risk of 3.7 in men and 6.5 in women. They also reported 2 deaths out of 10,000 patients using TEE during cardiac surgery. The team suggested finally not to use TEE routinely in cardiac surgery because of its 1/1000 risk of complications (14).
Despite the fact that some look at TEE as a diagnostic modality with more or less higher complications, the majority of authors realize that TEE would be grossly advised in terms of intraoperative cardiovascular monitoring and patient management, especially in hemodynamic field (15-17). A study by Almeida revealed 82% TEE satisfaction rate in patients in 1999 (15) and some even raise TEE as one of the greatest advances in direct and fast visualization of structural anatomy of the heart and great vessels in addition to homodynamic and functional evaluation of the cardiovascular system and consequently resulting in perfect formulation of a surgical strategy and decision making (16). For instance, Yumoto et al. reported 2.4% altered surgical repair method in 2002 based on TEE findings during cardiac surgery in children (18). This rate grows to more than 9% when > 12,000 cardiac surgery cases are studied by Eltzschig et al. in 1990 - 2005 to advise TEE in patients undergoing combined CABG and valve procedures which were, in turn, influenced by 12.3% in the case of making alternative decisions (19) as some other studies claim (20-22).
In 2015, TEE was studied in 656 patients with end-stage liver disease in terms of major gastro-esophageal and hemorrhagic complications to find that the technique was not associated with increased likelihood of the mentioned side effects after liver transplantation (23). Sore throat has not been named as a serious or common side effect of TEE during cardiac surgery (24).
One of the biggest studies to assess the safety of TEE in cardiac surgery is Kallmeyer’s which was done on 7200 patients in a single center to show only 0.2% morbidity and 0% mortality and name severe odynophagia as the most common complication with only 0.1% rate (2). They also reported 0.03% dental injury, 0.03% endotracheal tube malpositioning, 0.03% upper GI bleeding and 0.01% esophageal perforation that show a rather safe procedure. Some authorities have focused on recurrent laryngeal nerve palsy that would be a postoperative complication of TEE and nasogastric tube insertion. In this regard, Sakai et al. showed rate of PLNP with TEE has not increased although females had more frequent RLNP compared to those without TEE after cardiac surgery (25). This is while, at the same time, Kawahito et al. suggested that TEE is not responsible for postoperative RLNP after cardiac surgery while surgical manipulation and elongated surgery, cardiopulmonary bypass and tracheal intubation are the most common causative factors in this matter (26).
However, TEE sounds to be perfectly accepted by the majority of surgeons globally regarding its obviously grater usefulness than complications (27).
Through 10 years from 2001 to 2011, Viana et al. revealed an overall 30-day mortality rate of 33% and GI complication rate of 1.1% among > 5000 patients with cardiac surgery. This shows uncommon GI complications after cardiac surgery but high mortality rate disregarding whether TEE is used or not. So, the related complications need to be studied more carefully when we plan to find the special contribution of TEE in this regard (28).
Finally, from its first introduction into clinical practice in 1970’s, TEE has been mostly raised as a helpful intraoperative diagnostic tool, especially in high risk patients (29) and cardiac arrest (29-31) as well as a successful technique for immediate assessment of surgical outcomes to monitor and manage the operation and even change the plan or make new decisions if needed. (20-22).
4.1. Conclusions
Intraoperative trans-esophageal echocardiography has greater usefulness during cardiac surgeries than complications and is worth using in this case as well.
References
-
1.
Bonow RO, Carabella BA, Chatterjee K. ACC/AHA guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. American Heart Association Web Site; 2006. Available from: http://www.americanheart.org.
-
2.
Kallmeyer IJ, Collard CD, Fox JA, Body SC, Shernan SK. The safety of intraoperative transesophageal echocardiography: a case series of 7200 cardiac surgical patients. Anesth Analg. 2001;92(5):1126-30. [PubMed ID: 11323333].
-
3.
Brinkman WT, Shanewise JS, Clements SD, Mansour KA. Transesophageal echocardiography: not an innocuous procedure. Ann Thorac Surg. 2001;72(5):1725-6. [PubMed ID: 11722072].
-
4.
Cote G, Denault A. Transesophageal echocardiography-related complications. Can J Anaesth. 2008;55(9):622-47. [PubMed ID: 18840593]. https://doi.org/10.1007/BF03021437.
-
5.
Rousou JA, Tighe DA, Garb JL, Krasner H, Engelman RM, Flack J3, et al. Risk of dysphagia after transesophageal echocardiography during cardiac operations. Ann Thorac Surg. 2000;69(2):486-9. discussion 489-90. [PubMed ID: 10735685].
-
6.
Kohr LM, Dargan M, Hague A, Nelson SP, Duffy E, Backer CL, et al. The incidence of dysphagia in pediatric patients after open heart procedures with transesophageal echocardiography. Ann Thorac Surg. 2003;76(5):1450-6. [PubMed ID: 14602266].
-
7.
Ferraris VA, Ferraris SP, Moritz DM, Welch S. Oropharyngeal dysphagia after cardiac operations. Ann Thorac Surg. 2001;71(6):1792-5. discussion 1796. [PubMed ID: 11426749].
-
8.
Hogue CW, Lappas GD, Creswell LL, Ferguson TB, Sample M, Pugh D, et al. Swallowing dysfunction after cardiac operations: Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995;110(2):517-22. https://doi.org/10.1016/s0022-5223(95)70249-0.
-
9.
Chin JH, Lee EH, Choi DK, Choi IC. A modification of the trans-oesophageal echocardiography protocol can reduce post-operative dysphagia following cardiac surgery. J Int Med Res. 2011;39(1):96-104. [PubMed ID: 21672312]. https://doi.org/10.1177/147323001103900112.
-
10.
Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D'Ambra MN, Eltzschig HK. Safety of transesophageal echocardiography. J Am Soc Echocardiogr. 2010;23(11):1115-27. quiz 1220-1. [PubMed ID: 20864313]. https://doi.org/10.1016/j.echo.2010.08.013.
-
11.
Min JK, Spencer KT, Furlong KT, DeCara JM, Sugeng L, Ward RP, et al. Clinical features of complications from transesophageal echocardiography: a single-center case series of 10,000 consecutive examinations. J Am Soc Echocardiogr. 2005;18(9):925-9. [PubMed ID: 16153515]. https://doi.org/10.1016/j.echo.2005.01.034.
-
12.
Lennon MJ, Gibbs NM, Weightman WM, Leber J, Ee HC, Yusoff IF. Transesophageal echocardiography-related gastrointestinal complications in cardiac surgical patients. J Cardiothorac Vasc Anesth. 2005;19(2):141-5. [PubMed ID: 15868517].
-
13.
Hulyalkar AR, Ayd JD. Low risk of gastroesophageal injury associated with transesophageal echocardiography during cardiac surgery. J Cardiothorac Vasc Anesth. 1993;7(2):175-7. [PubMed ID: 8477022].
-
14.
Piercy M, McNicol L, Dinh DT, Story DA, Smith JA. Major complications related to the use of transesophageal echocardiography in cardiac surgery. J Cardiothorac Vasc Anesth. 2009;23(1):62-5. [PubMed ID: 19058977]. https://doi.org/10.1053/j.jvca.2008.09.014.
-
15.
Almeida J. [Transesophageal echocardiography in the operating room]. Rev Port Cardiol. 1999;18(5):531-9. [PubMed ID: 10418267].
-
16.
Junior CG, Botelho ES, Diego LA. Intraoperative monitoring with transesophageal echocardiography in cardiac surgery. Rev Bras Anestesiol. 2011;61(4):495-512. [PubMed ID: 21724013]. https://doi.org/10.1016/S0034-7094(11)70058-7.
-
17.
Romano P, Mangion JM. The role of intraoperative transesophageal echocardiography in heart transplantation. Echocardiography. 2002;19(7 Pt 1):599-604. [PubMed ID: 12376016].
-
18.
Yumoto M, Katsuya H. Transesophageal echocardiography for cardiac surgery in children. J Cardiothorac Vasc Anesth. 2002;16(5):587-91. [PubMed ID: 12407611].
-
19.
Eltzschig HK, Rosenberger P, Loffler M, Fox JA, Aranki SF, Shernan SK. Impact of intraoperative transesophageal echocardiography on surgical decisions in 12,566 patients undergoing cardiac surgery. Ann Thorac Surg. 2008;85(3):845-52. [PubMed ID: 18291154]. https://doi.org/10.1016/j.athoracsur.2007.11.015.
-
20.
Mishra M, Chauhan R, Sharma KK, Dhar A, Bhise M, Dhole S, et al. Real-time intraoperative transesophageal echocardiography--how useful? Experience of 5,016 cases. J Cardiothorac Vasc Anesth. 1998;12(6):625-32. [PubMed ID: 9854658].
-
21.
Sousa RC, Garcia-Fernandez MA, Moreno M, Tizon M, Valdeviesos M, Rubio M, et al. [The contribution and usefulness of routine intraoperative transesophageal echocardiography in cardiac surgery. An analysis of 130 consecutive cases]. Rev Port Cardiol. 1995;14(1):15-27. [PubMed ID: 7695952].
-
22.
Bryan AJ, Barzilai B, Kouchoukos NT. Transesophageal echocardiography and adult cardiac operations. Ann Thorac Surg. 1995;59(3):773-9. [PubMed ID: 7887737]. https://doi.org/10.1016/0003-4975(94)00818-3.
-
23.
Myo Bui CC, Worapot A, Xia W, Delgado L, Steadman RH, Busuttil RW, et al. Gastroesophageal and hemorrhagic complications associated with intraoperative transesophageal echocardiography in patients with model for end-stage liver disease score 25 or higher. J Cardiothorac Vasc Anesth. 2015;29(3):594-7. [PubMed ID: 25661642]. https://doi.org/10.1053/j.jvca.2014.10.030.
-
24.
Owall A, Stahl L, Settergren G. Incidence of sore throat and patient complaints after intraoperative transesophageal echocardiography during cardiac surgery. J Cardiothorac Vasc Anesth. 1992;6(1):15-6. [PubMed ID: 1543845].
-
25.
Sakai T, Terao Y, Miyata S, Hasuo H, Haseba S, Yano K. [Postoperative recurrent laryngeal nerve palsy following a transesophageal echocardiography]. Masui. 1999;48(6):656-7. [PubMed ID: 10402823].
-
26.
Kawahito S, Kitahata H, Kimura H, Tanaka K, Oshita S. Recurrent laryngeal nerve palsy after cardiovascular surgery: relationship to the placement of a transesophageal echocardiographic probe. J Cardiothorac Vasc Anesth. 1999;13(5):528-31. [PubMed ID: 10527219].
-
27.
Huang CH, Lu CW, Lin TY, Cheng YJ, Wang MJ. Complications of intraoperative transesophageal echocardiography in adult cardiac surgical patients - experience of two institutions in Taiwan. J Formos Med Assoc. 2007;106(1):92-5. [PubMed ID: 17282978]. https://doi.org/10.1016/S0929-6646(09)60223-0.
-
28.
Viana FF, Chen Y, Almeida AA, Baxter HD, Cochrane AD, Smith JA. Gastrointestinal complications after cardiac surgery: 10-year experience of a single Australian centre. ANZ J Surg. 2013;83(9):651-6. [PubMed ID: 23530720]. https://doi.org/10.1111/ans.12134.
-
29.
Schmid E, Nowak M, Unertl K, Rosenberger P. [Intraoperative echocardiography: impact on surgical decision-making]. Anaesthesist. 2009;58(11):1123-35. [PubMed ID: 19787301]. https://doi.org/10.1007/s00101-009-1620-2.
-
30.
Memtsoudis SG, Rosenberger P, Loffler M, Eltzschig HK, Mizuguchi A, Shernan SK, et al. The usefulness of transesophageal echocardiography during intraoperative cardiac arrest in noncardiac surgery. Anesth Analg. 2006;102(6):1653-7. [PubMed ID: 16717302]. https://doi.org/10.1213/01.ane.0000216412.83790.29.
-
31.
Schulmeyer MC, Santelices E, Vega R, Schmied S. Impact of intraoperative transesophageal echocardiography during noncardiac surgery. J Cardiothorac Vasc Anesth. 2006;20(6):768-71. [PubMed ID: 17138077]. https://doi.org/10.1053/j.jvca.2006.05.004.