Abstract
Introduction:
Dilated pulmonary artery can increase the postoperative airway complications after the simultaneous repair of aortic arch anomalies and cardiovascular lesions with large left to right shunt. It is claimed that the anterior translocation of pulmonary artery will reduce the airway compression.Case Presentation:
Here we report 3 cases including an 11-month-old infant with ventricular septal defect (VSD) and coarctation, a 2-month-old infant with interrupted aortic arch (IAA) and VSD, and a neonate with aortopulmonary window (APW) in combination with coarctation in which all had a one stage repair of their lesions. Translocation of the right pulmonary artery (RPA) branch was performed in two patients, however with different postoperative courses that merit pondering over their fate.Conclusions:
RPA anterior translocation could be considered as an additional palliation in some patients with coarctation repair from midsternotomy approach.Keywords
Coarctation of Aorta Bronchial Stenosis Midsternotomy Pulmonary Artery Translocation
1. Introduction
Simultaneous repair of coarctation and other cardiovascular lesions with large left to right shunts through median sternotomy may cause airway complication in the early postoperative period especially in small infants. To avoid the complication of airway compression in such cases, there are reports of anterior translocation of the right pulmonary artery (RPA) branch (1).
Here we report the fate of three cases of aortic arch repair through median sternotomy who were high risk for postoperative airway complication due to a dilated right pulmonary artery. This procedure is recommended instead of anterior aortopexy which might be ineffective or even dangerous in coarctation repair through median sternotomy (2).
2. Case Presentation
2.1. Case 1
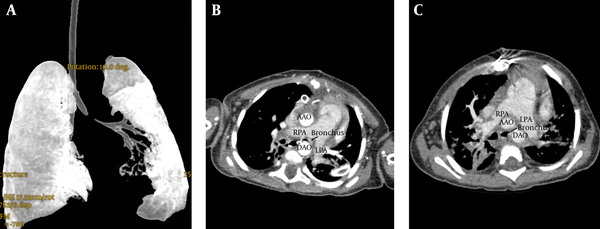
An 11-month-old female infant, 7.4 kg weight was referred to our hospital for cardiac surgery. Echocardiography showed a large perimembranous ventricular septal defect (VSD), severe discrete type coarctation with narrowing of the transverse arch and confluent dilated pulmonary artery branches. Catheterization and angiography confirmed the echocardiographic findings in addition to a reactive pulmonary hypertension. We decided to approach the VSD and coarctation in a one stage repair through median sternotomy. Under hypothermic cardiopulmonary bypass VSD was closed through tricuspid valve with a Gore-Tex patch. After total circulatory arrest the coarctation and transverse arch repair was performed. However, postoperatively the patient could not be weaned from mechanical ventilation because of continuous elevated CO2 in serial arterial blood gases (ranging from 58 to 83 mmHg). Despite aggressive physiotherapy, chest X-Ray showed persistent collapse of the left lung. Fluoroscopy ruled out the diaphragmatic paralysis. CT angiography and virtual CT bronchography showed the compressive effect of the dilated RPA on the left main bronchus (Figure 1A and B). Hence we decided to perform the anterior RPA translocation to relieve the airway compression (Figure 1C). The day after RPA translocation she was extubated and finally discharged after a total of 25 days hospital stay including 12 days of ICU admission.
Compressive Effect of the Dilated RPA on the Left Main Bronchus on Virtual CT Bronchography (A) and CT Angiography (B) that Was Relieved After Anterior RPA Translocation (C)
2.2. Case 2
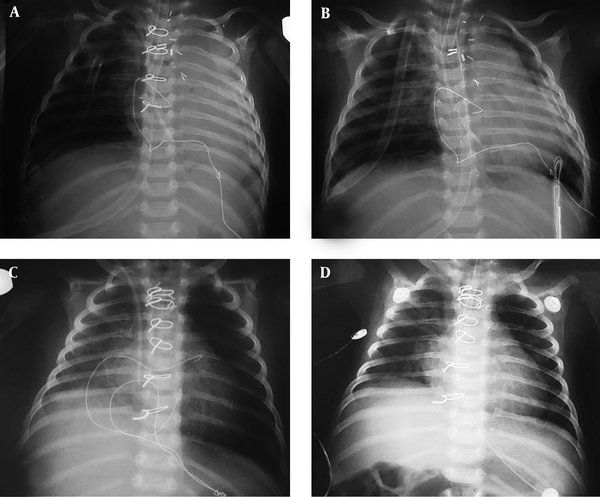
A 2-month-old female infant weighing 3.5 kilograms was admitted due to poor feeding and tachypnea. Echocardiography demonstrated a large inlet to outlet VSD with an interrupted aortic arch (IAA) and dilated pulmonary artery branches. Multislice CT angiography showed IAA type B with an aberrant right subclavian artery (RSCA) in addition to aneurysmal dilated pulmonary artery branches. Fluorescent in situ hybridization (FISH) revealed the microdeletion of 22q11.2 in favor of Digeorge syndrome. After median sternotomy, the large VSD was repaired by Gore-Tex patch, the aberrant RSCA was dissected and the interruption was repaired by an end to side anastomosis between descending and ascending aorta. Then anterior translocation of the RPA was done using the flap-door technique. However postoperative chest radiographies in ICU showed persistent left lung collapse (Figure 2A) and elevated arterial PCO2 (58 mmHg) despite the anterior translocation of RPA. Fluoroscopy ruled out the diaphragmatic paralysis. Finally 10 days postoperation the patient was weaned and extubated by physiotherapy and supportive airway management with an ICU stay of 24 days. During the hospital admission, all of her blood and tracheal cultures were negative and the last chest X-Ray showed the resolution of left lung collapse (Figure 2B).
A and B Left Lung Collapse After the Repair of IAA from Midsternotomy Despite Anterior Translocation of RPA. C and D, Postoperative Air Entrapment in the Left Lung of a Patient Who Underwent Surgery for COA and APW Due to a Checked Valve Compressive Mechanism. He Was Managed Only By Chest Physiotherapy Without Anterior Translocation of RPA
2.3. Case 3
A 23-day-old male neonate was presented with tachypnea and tachycardia. His weight was 3.2 kilograms. Echocardiography revealed aortopulmonary window (APW) in addition to a discrete type coarctation of the aorta. The PA branches were dilated. The correction of APW and repair of coarctation were performed via median sternotomy at one stage. We missed to perform RPA anterior translocation in this patient. Four days postoperation he was extubated. However, his chest radiographies showed air entrapment in the left lung due to a checked valve compressive mechanism (Figure 2C). Arterial blood gas showed elevated PCo2 (66 mmHg). Diaphragmatic paralysis was ruled out. He was considered a candidate for anterior RPA translocation procedure. However gradually with supportive airway management, the left lung air entrapment was resolved (Figure 2D) and PCo2 was declined. Hence, we could wean and extubate the patient. He was in hospital for 22 days with an ICU stay of 14 days.
3. Discussion
The right pulmonary artery and the left main bronchus are the two major anatomical components with close proximity passing under the aortic arch space. In cases of left to right shunt with pulmonary hypertension the dilated pulmonary artery has compressive effect on the left main bronchus that is more prominent in infants with smaller airways (3). Although the pulmonary artery pressure and hence the compressive effect of it on the airway is reduced after the closure of left to right shunts, the bowstring effect of the repaired arch is added particularly in patients with an unusual anterior location of the descending aorta. Moreover the complicated lung parenchyma may cause a vicious cycle that does not let the drop in pulmonary artery pressure and therefore the compressive effect of the RPA on the left main bronchus will continue.
Anterior translocation of the right pulmonary artery by connecting the RPA to the main pulmonary artery with a large trapdoor flap will relieve the airway compression postoperatively. It is claimed that this maneuver will reduce the duration of postoperative mechanical ventilation (4). All of our patients had one stage repair of left-to-right shunt defect and arch anomaly through median sternotomy. The first case with COA and VSD could not be weaned from the ventilator until the anterior translocation of the RPA was done for her. Soon after RPA anterior translocation, PCO2 retention and the left lung collapse were resolved. In the second patient with Digeorge syndrome, a case of IAA and VSD, although we prophylactically transferred the RPA to the anterior, postoperative collapse of the left lung occurred in the absence of diaphragmatic paralysis. Hence this maneuver could not hamper the occurrence of left lung collapse. However our patient might have had a longer ICU admission and more airway complications on the background of immune deficiency if RPA translocation was not performed. And finally the third case with APW and COA was handled without this maneuver at a similar period of ICU admission. The left main bronchus compressive features were resolved only with chest physiotherapy and mechanical ventilation management. Regarding the postoperative course of our patients we think that the anterior translocation of the right pulmonary artery should not be done in all patients who are candidates for one-stage repair of arch anomaly and left-to-right shunt cardiac lesion through median sternotomy. Hence we recommend considering this maneuver in selected individuals for example in patients with Digeorge syndrome. In this syndrome, which is more commonly seen in patients with aortic arch anomaly, prolonged postoperative mechanical ventilation and its associated pneumonia will be life threatening (5). Thus RPA anterior translocation that shortens the postoperative mechanical ventilation period will be helpful for airway management of these syndromic patients. The lower age with small airway diameters, the evidence of an abnormally anterior located descending aorta and the compressive narrowing of the left main bronchus in the preoperative CT angiography are the other risk factors that must be considered for anterior translocation of the RPA.
In summary RPA anterior translocation might be necessary and lifesaving in some patient with midline coarctation repairs such as our first case, but that does not necessarily eliminate the risk of postoperative left main bronchus compression as our second case and is not mandatory in all coarctation repairs from the midline like the third case. Although the complications of the translocated RPA such as its negligible stenosis, it may cause some limitation for future surgical manipulation on the aortic valve and ascending aorta, for example a bicuspid aortic valve and a dilated ascending aorta that may accompany aortic coarctation. More studies with larger sampler sizes are necessary to conclude whether RPA anterior translocation will be helpful or not in this cohort of patients.
References
-
1.
Jhang WK, Park JJ, Seo DM, Goo HW, Gwak M. Perioperative evaluation of airways in patients with arch obstruction and intracardiac defects. Ann Thorac Surg. 2008;85(5):1753-8. [PubMed ID: 18442579]. https://doi.org/10.1016/j.athoracsur.2008.01.059.
-
2.
Chang YH, Sung SC, Kim H, Choo KS, Lee HD, Park JA. Anterior translocation of the right pulmonary artery to avoid airway compression in aortic arch repair. Ann Thorac Surg. 2013;96(6):2198-202. [PubMed ID: 24034207]. https://doi.org/10.1016/j.athoracsur.2013.06.079.
-
3.
Talwar S, Sharma P, Choudhary SK, Kothari SS, Gulati GS, Airan B. Le-Compte's maneuver for relief of bronchial compression in atrial septal defect. J Card Surg. 2011;26(1):111-3. [PubMed ID: 21235629]. https://doi.org/10.1111/j.1540-8191.2010.01183.x.
-
4.
Chang YH, Sung SC, Kim H, Lee HD. Anterior translocation of the right pulmonary artery for relief of airway compression in the repair of distal aortopulmonary window and interrupted aortic arch. Ann Thorac Surg. 2012;93(6):e159-61. [PubMed ID: 22632536]. https://doi.org/10.1016/j.athoracsur.2011.12.027.
-
5.
Yeoh TY, Scavonetto F, Hamlin RJ, Burkhart HM, Sprung J, Weingarten TN. Perioperative management of patients with DiGeorge syndrome undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28(4):983-9. [PubMed ID: 24461359]. https://doi.org/10.1053/j.jvca.2013.10.025.