Abstract
Background:
The neonatal mortality rate remains high in developing countries despite the significant reduction in under-five mortality globally. Therefore, periodic evaluations on the causes of mortality are an aspect of health status, which could be performed to improve the neonatal mortality rate.Objectives:
The present study aimed to determine the pattern and causes of neonatal mortality in the Federal Medical Center in Owo, Ondo State, Southwest Nigeria.Methods:
This retrospective study was conducted using the hospital records of the neonates admitted over a five-year period from 1st of January 2015 to 31st of December 2019.Results:
In total, 2,065 neonates were admitted, including 208 cases of neonatal deaths. Mortality occurred in 127 males (61.1%) and 81 females (38.9%), with the male-to-female ratio of 1.6:1. Among the recorded deaths, 114 cases (54.8%) occurred within the first 24 hours of admission, while 94 neonates (45.2%) died after 24 hours of admission. In addition, the mortality rate was higher among outborn neonates (n = 120; 57.7%) compared to inborn neonates (n = 88; 42.3%). The major causes of neonatal deaths included birth asphyxia (46.6%), prematurity (23.1%), and sepsis (17.8%). The overall mortality rate over the five-year period was 10.1%, which is equivalent to 19 deaths per 1,000 live births.Conclusions:
According to the results, preventable diseases such as birth asphyxia, prematurity, and sepsis remain the major causes of neonatal mortality, of which neonatal deaths occur mostly within 24 hours of admission.Keywords
1. Background
Neonatal mortality remains high despite the significant reduction in under-five mortality in recent years (1). Globally, neonatal deaths account for 40% of under-five mortalities, and 75% of these mortalities occur within the first seven days of life, while 40% occur in the first 24 hours (2, 3). The survival of an infant is largely dependent on the incidents during the neonatal period (4).
In developed countries, congenital anomalies have been reported to be the major cause of neonatal mortality, while in developing countries, preventable causes such as perinatal asphyxia, neonatal sepsis, and neonatal jaundice still account for most cases of neonatal mortality (5, 6). Neonatal deaths have reduced significantly in developed countries due to the improvement in the healthcare system (7).
According to the Nigeria Demographic and Health survey (2018 NDHS), infant mortality rate declined within 10 years (from 75 deaths per 1,000 live births in 2008 to 67 deaths per 1,000 live births in 2018) with no significant change in the neonatal mortality rate in the same decade (40 deaths per 1,000 live births in 2008 versus 39 deaths per 1,000 live births in 2018) (8). The burden of neonatal mortality in Nigeria accounted for 6% of the global neonatal deaths in 2005 (4), while the country moved from the third to the second position in terms of the highest number of neonatal deaths in the world between 2000 - 2010 (9).
Knowledge of the pattern of admissions and deaths in hospitalized neonates reflects the major causes, as well as the available standard of care for neonates in a particular region. In order to reduce neonatal mortality as stated in the Sustainable Development Goal 3, it is imperative to identify the common causes of neonatal mortality so as to proffer solutions. Furthermore, the knowledge of the causative disease and mortality patterns from the periodic audit of neonatal admissions and deaths could help determine the effects of the current practices to mitigate neonatal mortality, as well as the challenges against neonatal survival in the environment, so that appropriate and effective preventive measures could be taken.
In the southwest of Nigeria, data are scarce regarding the common causes of neonatal mortality.
2. Objectives
The present study aimed to investigate the pattern of neonatal admissions and causes of neonatal mortality in a tertiary health center in the southwest of Nigeria. The research findings could largely contribute to the planning of effective interventions for reducing the morbidity and mortality of newborns.
3. Methods
3.1. Study Design
This descriptive-retrospective study was conducted over a five-year period from the 1st of January 2015 to 31st of December 2019.
3.2. Study Setting
The study was carried out in the neonatal unit of the Pediatric Department of the Federal Medical Center (FMC) Owo, located in Ondo State, Nigeria. The FMC in Owo is a tertiary hospital owned by the Federal Government and is strategically located to receive referrals from the catchment areas, including Ondo, Ekiti, Osun, Kogi, and Edo states, Nigeria. The hospital has an obstetrics unit that admits high-risk deliveries from other healthcare institutions in the catchment areas. The neonatal unit is a 20-bedded ward, which is divided into the Inborn and Outborn units. The inborn unit has 10 beds and receives admission from the labor ward, labor ward theatre, and postnatal ward. The Outborn Unit has 10 beds and admits neonates from home, primary and secondary healthcare centers, and other referral centers. The neonatal unit is supervised by two consultants, two senior registrars, four registrars, four interns, and 15 nurses that run the shifts.
3.3. Sampling
Clinical diagnosis was based on medical history, physical examination, and laboratory results. Gestational age was assessed based on the last menstrual period, and the new Ballard score chart was used in the case of the women who were unsure of their date (10). The neonates delivered alive before the gestational age of 37 completed weeks were considered preterm. Birth weight was classified in accordance with the World Health Organization (WHO) weight classification (11). Blood culture and cerebrospinal fluid analysis was performed to isolate pathogenic organisms for the diagnosis of neonatal sepsis and meningitis, respectively. The neonates who died within 0 - 7 completed days of life were defined as early neonatal death, while those who died within 7 - 28 days of life were defined as late neonatal death (12).
Data on neonatal jaundice were available in the clinical assessment records and had been confirmed by laboratory investigation. Congenital anomalies were based on clinical grounds with some evaluations where feasible. Perinatal asphyxia was diagnosed in the neonates with the one- and five-minute Apgar scores of < 7, those who were unresponsive to stimuli, and the neonates with unexplained convulsion by other causes (13). As for the neonates who had been born outside health facilities with unknown Apgar scores, details were obtained from the mother on factors such as crying immediately after birth, floppiness, loss of consciousness, presence of convulsion, and loss of neonatal reflexes. Other assessments were based on physicians’ judgment as noted in the patient case files.
3.4. Data Collection Tools
Data on the admission registers, discharge registers, death register, delivery register, and case files of the neonates were obtained from the medical records department of the hospital.
3.5. Data Collection Method
The available records of the neonates aged 0 - 28 days, who were admitted under the care of the Department of Pediatrics over the study period, were assessed to extract the relevant data. Data obtained from the records included age, gender, length of hospital stay, weight at admission, final diagnosis, and age at death. The length of hospital stay before death was calculated from the date of admission to the date of death. The final diagnoses were based on the clinical features and laboratory test reviewed by at least a senior registrar or a consultant pediatrician. The total number of the live births was obtained from the Department of Obstetrics and Gynecology, and neonatal deaths were discussed at the mortality and morbidity meeting carried out weekly by the Department of Pediatrics.
3.6. Ethical Considerations
The study protocol was approved by the Health Research Ethics Committee of the FMC Owo in the Ondo state, Nigeria (registration number: FMC/OW/380/VOL.XCI/200).
3.7. Statistical Analysis
Data analysis was performed in SPSS version 22.0 using frequency, means, standard deviations, and cross tabulations. The means and proportions were compared using student’s t-test, and the rate was expressed per 1,000. The P-value of less than 0.05 was considered significant.
4. Results
In total, 2,070 neonates were admitted during the study period, and the total mortality was 213, with five cases (2.3%) defined as postnatal death, which were excluded from the study. The total admissions for the study were estimated at 2,065 neonates, with the total neonatal mortality of 208. The neonatal deaths included 127 males (61.1%) and 81 females (38.9%) with the male-to-female ratio of 1.6:1. The mean age at death was 6.3 + 7.2 days, and 143 neonates (68.8%) died within seven days of life (early neonatal death), while 65 neonates (31.2%) died after seven days of life and within 28 days (late neonatal death). In addition, 114 deaths (54.8%) occurred within the first 24 hours of admission, and 94 neonatal death (45.2%) after 24 hours of admission. The mean duration of admission at death was 3.6 + 5.0 days, and both inborn and outborn neonates were admitted. Among 208 mortalities, 88 cases (42.3%) were inborn neonates, and 120 cases (57.7%) were outborn neonates.
Table 1 shows the causes of death during the study period. Birth asphyxia accounted for almost half of the mortalities, while one case (0.5%) died of neonatal tetanus. Surgical cases were five neonates (2.4%), including two cases of Hirschsprung’s disease, one case of jejunal atresia, one case of gastroschisis, and one case of encephalocoele. In addition, Lassa fever accounted for two deaths (1.0%).
Causes of Neonatal Mortality
| Diagnosis | No. (%) |
|---|---|
| Birth asphyxia | 97 (46.6) |
| Prematurity | 48 (23.1) |
| Sepsis | 37 (17.8) |
| Jaundice | 9 (4.3) |
| Surgical cases | 5 (2.4) |
| Meningitis | 4 (1.9) |
| Lassa fever | 2 (1.0) |
| Tetanus | 1 (0.5) |
| Othera | 5 (2.4) |
| Total | 208 (100.0) |
The neonatal mortality per year is presented in Table 2. Accordingly, one-quarter of the deaths occurred in 2019, and approximately 15% of the deaths were reported in 2018. The findings indicated that more deaths were recorded in the outborn unit compared to the inborn unit. Figure 1 depicts the neonatal mortality rate per year. According to the obtained results, the highest neonatal mortality rate was reported in 2017 (31 per 1,000 live births), while 2018 had the lowest neonatal mortality rate (11 per 1,000 live births). The overall neonatal mortality rate per 1,000 live birth over the five-year period of the study was 19 per 1,000 live births.
Neonatal Mortality Per Year
| Year | Inborn, No. (%) | Outborn, No. (%) | Total, No. (%) |
|---|---|---|---|
| 2015 | 21 (23.9) | 24 (20.0) | 45 (21.6) |
| 2016 | 19 (21.6) | 18 (15.0) | 37 (17.8) |
| 2017 | 26 (29.5) | 19 (15.8) | 45 (21.6) |
| 2018 | 9 (10.2) | 21 (17.5) | 30 (14.4) |
| 2019 | 13 (14.8) | 38 (31.7) | 51 (24.5) |
| Total | 88 (100) | 120 (100) | 208 (100) |
The neonatal mortality rate per year
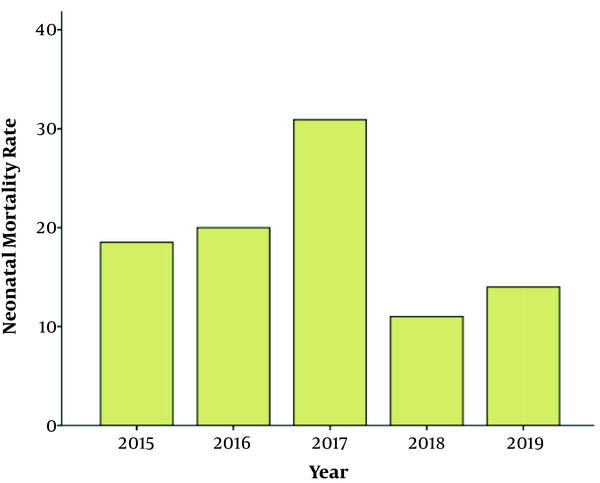
The recorded neonatal mortality per year were reported to be 9.3% in 2015, 10.3% in 2016, 11.7% in 2017, 8.1% in 2018, and 11.0% in 2019. The total neonatal mortality over the five-year period of this review was 10.1%. Notably, five postnatal deaths were recorded due to sepsis (n = 3), birth asphyxia (n = 1), and acute kidney injury (n = 1).
5. Discussion
The present study aimed to determine the pattern and causes of neonatal mortality in a tertiary hospital in the Southwest of Nigeria. According to the findings, more deaths were recorded among males compared to females, which is consistent with the similar studies conducted in Nigeria (14 - 17) and Pakistan (18). This might be due to the fact that male neonates are generally more susceptible to infections than females as studies have revealed that the diseases linked to the X chromosome are less common in female infants than males, which is indicative of the genetic influence on neonatal infection (19). It may also be associated with the priority placed on the male child in this part of the world, which in turn prompts health-seeking behaviors.
In the present study, more than 50% of the neonatal deaths occurred within the first 24 hours of admission, which is consistent with the previous studies in this regard (20, 21). This finding also supports the fact that in most of the patients with a late referral to the hospital in a critical state of health, delays at various levels of health-seeking should be addressed, such as delayed decision to seek care and delay in reaching the healthcare facility.
According to the findings of the current research, the leading causes of neonatal mortality were birth asphyxia, prematurity, and sepsis. This is consistent with the studies conducted in Umuahia (22) and other regions of Nigeria (23-26). Birth asphyxia was the most common cause of death (46.6%) in the present study, which is in line with the findings reported in Lagos (14), Kano (15), and Benin (27). This could be attributed to the poor antenatal care (ANC), delivery attendance by unskilled personnel, and poor referral system, which should be improved by educating the populace, encouraging proper ANC visitations, training of healthcare providers on effective obstetric care and neonatal resuscitation, availability of facilities for neonatal resuscitation at delivery centers, and appropriate referral systems to avoid delays at various levels. On the other hand, our findings in this regard are inconsistent with the results obtained in Jos (20) and Pakistan (28), where prematurity has been reported to be the most common cause of neonatal mortality. The mortality rate in the current research was higher among the outborn neonates compared to the inborn neonates, which is consistent with the previous studies (22-24).
According to our findings, Lassa fever accounted for two neonatal deaths, and this number could be higher due to the fact that the study center is in a Lassa fever endemic zone and the features of Lassa fever could easily be misdiagnosed as neonatal sepsis. However, data are scarce regarding Lassa fever as a cause of neonatal mortality. Notably, the FMC of Owo is a leading Lassa fever treatment center in Nigeria.
In the present study, neonatal tetanus accounted for one death, and the observed rate was lower than the reported rates in the studies performed in Umuahia (22) and Benin (29). The discrepancy might be due to the government-driven efforts to raise awareness and increase the immunization of pregnant women in order to reduce the incidence of neonatal tetanus.
In the current research, the neonatal mortality rate was determined to be 19 deaths per 1,000 live births over the five-year period and 11 deaths per 1,000 live births in 2018, which was significantly lower than the national average neonatal mortality rate reported in 2018 (39 deaths per 1,000 live birth) (8). This could be explained by the availability of specialist care, proper obstetric facilities, and presence of neonatal resuscitative equipment for prompt and qualitative care at this centre, which may not be available at lower levels of health care.
The overall mortality over the study period in the current research was 10.1%, which was lower than the findings in Delta (20.3%) (30), Calabar (19.3%) (31), and Umuahia (16.0%) (22). The difference in this regard could be due to the fact that the present study was carried out in a tertiary center, and most neonatal deaths occur at home and primary or secondary healthcare facilities. Another reason for the discrepancy could be the increased knowledge of patient care and availability of medical facilities over time.
5.1. Conclusions
According to the results, birth asphyxia was the major cause of neonatal mortality, with most deaths occurring within 24 hours of admission. The overall neonatal mortality rate per 1,000 live births over the five-year study period was 19 per 1,000 live births. Therefore, the training of healthcare providers is recommended on obstetric care and resuscitation, while the availability of adequate facilities should also be prompted at every level, in order to minimize the rate of neonatal deaths.
5.2. Limitations of the Study
Since this was a retrospective study, some of the data obtained from the registers and case files might not have been accurate; for instance, the initial diagnosis of some patients might have differed from the final diagnosis without being reflected in the records. In addition, the records might not have been properly documented due to clerical errors, especially when electronic medical recording is yet to commence in this center.
5.3. Research Implications
1) Pattern of perinatal mortality could be further studied as it is a better reflection of health care in neonates.
2) A longitudinal prospective study of neonatal mortality is suggested.
Acknowledgements
References
-
1.
Save the Children International. State of the world's mothers: surviving the first day. London: Save the Children; 2013.
-
2.
World Health Organization (WHO). The Lancet neonatal Survival Series. Geneva, Switzerland: WHO; 2005.
-
3.
World Health Organization (WHO). Neonatal and perinatal mortality: country, regional and global estimates. Geneva, Switzerland: WHO; 2006.
-
4.
Lawn JE, Cousens S, Zupan J, Lancet Neonatal Survival Steering T. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891-900. [PubMed ID: 15752534]. https://doi.org/10.1016/S0140-6736(05)71048-5.
-
5.
Jehan I, Harris H, Salat S, Zeb A, Mobeen N, Pasha O, et al. Neonatal mortality, risk factors and causes: a prospective population-based cohort study in urban Pakistan. Bull World Health Organ. 2009;87(2):130-8. [PubMed ID: 19274365]. [PubMed Central ID: PMC2636189]. https://doi.org/10.2471/blt.08.050963.
-
6.
Yadav S, Kumar A, Khinchi YR. Profile of Neonatal sepsis. J Col Med Sci Nepal. 2010;6(2):1-6. https://doi.org/10.3126/jcmsn.v6i2.3609.
-
7.
Sridhar PV, Thammanna PS, Sandeep M. Morbidity pattern and hospital outcome of neonates admitted in a tertiary care teaching hospital, Mandya. Int J Sci Stud. 2015;3(6):126-9.
-
8.
National Population Commission (NPC) [Nigeria] and ICF. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria and Rockville Maryland, USA: NPC and ICF; 2019.
-
9.
Lawn JE, Kinney MV, Black RE, Pitt C, Cousens S, Kerber K, et al. Newborn survival: a multi-country analysis of a decade of change. Health Policy Plan. 2012;27 Suppl 3:iii6-28. [PubMed ID: 22692417]. https://doi.org/10.1093/heapol/czs053.
-
10.
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard Score, expanded to include extremely premature infants. J Pediatr. 1991;119(3):417-23. [PubMed ID: 1880657]. https://doi.org/10.1016/s0022-3476(05)82056-6.
-
11.
World Health Organization. Promoting Optimal Fetal Development: Report of a Technical Consultation. Geneva: World Health Organization; 2006. 3 p.
-
12.
UNICEF; WHO. Levels and trends in child mortality. New York, USA: The World Bank, UN; 2014.
-
13.
Memon S, Shaikh S, Bibi S. To compare the outcome (early) of neonates with birth asphyxia in-relation to place of delivery and age at time of admission. J Pak Med Assoc. 2012;62(12):1277-81. [PubMed ID: 23866472].
-
14.
Ezeaka VC, Ogunbase AO, Awongbemi OT, Grange AO. Why our children die: a review of paediatric mortality in a tertiary centre in Lagos, Nigeria. Niger Q J Hospital Med. 2005;13(1). https://doi.org/10.4314/nqjhm.v13i1.12502.
-
15.
Mukhtar-Yola M, Iliyasu Z. A review of neonatal morbidity and mortality in Aminu Kano Teaching Hospital, northern Nigeria. Trop Doct. 2007;37(3):130-2. [PubMed ID: 17716492]. https://doi.org/10.1258/004947507781524683.
-
16.
Ochoga MO, Abah RO, Idoko A, Dabit JO, Ebonyi A, Okpe ES. Pattern of Diseases and Outcomes of Neonatal Admission in Benue State University Teaching Hospital, Makurdi, Nigeria. J Bio Res Clin Pract. 2018;1(1):74-80. https://doi.org/10.46912/jbrcp.37.
-
17.
Okechukwu AA, Achonwa A. Morbidity and mortality patterns of admissions into the Special Care Baby Unit of University of Abuja Teaching Hospital, Gwagwalada, Nigeria. Niger J Clin Pract. 2009;12(4):389-94. [PubMed ID: 20329678].
-
18.
Ali SR, Ahmed S, Lohana H. Disease patterns and outcomes of neonatal admissions at a secondary care hospital in pakistan. Sultan Qaboos Univ Med J. 2013;13(3):424-8. [PubMed ID: 23984028]. [PubMed Central ID: PMC3749027].
-
19.
Libert C, Dejager L, Pinheiro I. The X chromosome in immune functions: when a chromosome makes the difference. Nat Rev Immunol. 2010;10(8):594-604. [PubMed ID: 20651746]. https://doi.org/10.1038/nri2815.
-
20.
Toma B, Ige O, Abok I, Onwuanaku C, Abah R, Donli A. Pattern of neonatal admissions and outcome in a tertiary institution in north central Nigeria. J Med Trop. 2013;15(2). https://doi.org/10.4103/2276-7096.123590.
-
21.
Also U, Gwarzo G. Patterns of morbidity and mortality among neonates seen in a tertiary hospital. Sahel Med J. 2020;23(1). https://doi.org/10.4103/smj.smj_21_19.
-
22.
B E. Pattern of Neonatal Mortality in a Teritiary Health Facility in Umuahia, South East, Nigeria. Int J Trop Dis Health. 2014;4(2):136-46. https://doi.org/10.9734/ijtdh/2014/4985.
-
23.
Ezechukwu CC, Ugochukwu EF, Egbuonu I, Chukwuka JO. Risk factors for neonatal mortality in a regional tertiary hospital in Nigeria. Niger J Clin Pract. 2004;7(2):50-2.
-
24.
Onwuanaku CA, Okolo SN, Ige KO, Okpe SE, Toma BO. The effects of birth weight and gender on neonatal mortality in north central Nigeria. BMC Res Notes. 2011;4:562. [PubMed ID: 22195995]. [PubMed Central ID: PMC3279327]. https://doi.org/10.1186/1756-0500-4-562.
-
25.
Lawoyin TO, Onadeko MO, Asekun-Olarimoye EO. Neonatal mortality and perinatal risk factors in rural southwestern Nigeria: a community-based prospective study. West Afr J Med. 2010;29(1):19-23. [PubMed ID: 20496333]. https://doi.org/10.4314/wajm.v29i1.56183.
-
26.
Oladokun RE, Orimadegun AE, Oluwu JA. A ten-year review of neonatal deaths in the special care baby unit at the University College Hospital, Ibadan. Niger J Paediatr. 2006;31(4). https://doi.org/10.4314/njp.v31i4.12098.
-
27.
Omoigberale AI, Sadoh WE, Nwaneri DU. A 4 year review of neonatal outcome at the University of Benin Teaching Hospital, Benin City. Niger J Clin Pract. 2010;13(3):321-5. [PubMed ID: 20857794].
-
28.
Parkash J, Das N. Pattern of admissions to neonatal unit. J Coll Physicians Surg Pak. 2005;15(6):341-4. [PubMed ID: 15924838].
-
29.
Adeyemo F, Abioye T, Felicia A, Usunobun A. Incidence of neonatal tetanus in a Nigerian State Hospital, Benin, Nigeria. J Health Res Rev. 2016;3(3). https://doi.org/10.4103/2394-2010.193187.
-
30.
Ugwu GIMG. Pattern of morbidity and mortality in the newborn special care unit in a tertiary institution in the Niger Delta region of Nigeria: A two year prospective study. Glob Adv Res J Med Med Sci. 2012;1(6):133-8.
-
31.
Udo JJ, Anah MU, Ochigbo SO, Etuk IS, Ekanem AD. Neonatal morbidity and mortality in Calabar, Nigeria: a hospital-based study. Niger J Clin Pract. 2008;11(3):285-9. [PubMed ID: 19140371].
