Abstract
Context:
Over the last decades, the prevalence of overweight (BMI > 25) and obesity (BMI > 30) is being the most important health challenge in urban populations. The relationship between obesity and the individual’s temperament has not been studied yet.Evidence Acquisition:
This review aimed to study the causes of obesity, especially in middle-aged people, according to the new evidence of conventional medicine and findings of Traditional Persian Medicine (TPM) physicians cited in their books. Databases including PubMed, Scopus, and Iran Medex were also searched with keywords obesity and overweight for recent evidence in conventional medicine.Results:
Based on the traditional Persian medicine findings, dystemprament or disequilibrium in Mizaj may promote obesity in middle-aged and elderly people. The attenuation of innate heat and intrinsic moisture in middle age could increase the chance of overweight and obesity. Recent studies in modern nutrition reveal a linear relationship between diminishing the basal metabolic rate and increasing age, especially in middle age. Accordingly, cold-wet-tempered people have more efficient energy homeostasis than hot-dry-tempered people that is similar to individuals with Firmicutes gut microbiota predominance. People living in high altitudes and cold-dry climates maintain their innate heat better than people living in wet climates. It is in accordance with the increasing brown adipose tissue thermogenesis in cold exposure, which decreases the chance of obesity.Conclusions:
Based on traditional Persian medicine school, it is hypothesized that increasing age and diminishing innate heat besides the accumulation of phlegm (moisture) in the gastrointestinal tract of middle-aged individuals may be influential in altering gut microbiota and consequently obesity. It seems that there may be a correlation between cold/wet Mizaj and risk factors of obesity.Keywords
Obesity Overweight Middle Age Traditional Persian Medicine Nutrition
1. Context
Understanding the pathophysiology of obesity should be reconsidered due to either the complex mechanism or the growing trend of obesity prevalence. Overweight and obesity are defined as the abnormal accumulation of fat, threatening health (1). Recent 20-year surveys reveal a double rise in overweight among children and adolescents (2-4). According to WHO data in 2016, the overweight population (BMI > 25 kg/m2) and obese people (BMI > 30 kg/m2) greater than 18-years-old amounted to more than 1.9 billion and 600 million, respectively. The prevalence of overweight and obesity in adult populations increased from 6% in 1980 to 12% in 2008 (5). It is predicted that obesity will affect 60% of male adolescents, 50% of female adults, and 25% of children up to 2050 in the United States, England, and most European nations. The prevalence of obesity is estimated at 21.7% in Iranians above 18 years and 6.1% in populations below 18 (6). The growing trend of overweight in children in recent decades is a warning sign of increasing the worldwide disability-adjusted life-years (DALYs) in the near future (7). Despite enormous research on obesity management among different medical research specialties, evidence shows that the trend of obesity upsurges in developed and developing countries. Although a few new topics have been opened in the recent decade in the mechanism of obesity, such as the role of brown adipose tissue, diet, energy expenditure, climate, microbiota, homeostasis, and contribution of hormonal plasma such as leptin, epigenetic, etc., neither optimal medical guidelines nor treatment protocols have been developed for obesity management yet (8).
Hippocrates (circa 460 - 377 B.C.) and Galen (129 - 199), the pioneers of humoral medicine, believe in the relationship between body temperament and health. Based on traditional medicine schools, including Unani, Persian, Chinese, and Ayurveda, people could be classified based on their dominant temperament, and accordingly, the maintenance of temperament equilibrium, especially hotness and coldness, warrants their health (9, 10). Avicenna (973 - 1037 AD), the great Persian physician, in his masterpiece Canon, a comprehensive textbook of medicine, presents humoral medicine in a newer form, the Theory of Temperament or Mizaj (7, 8). Persian medieval physicians believe that disequilibrium among four qualities, including hotness, coldness, wetness, and dryness is the main cause of dystemperament (diathesis) and disease states. Accordingly, everybody experiences different temperaments (Mizaj) throughout life. People in childhood have hot-wet Mizaj, while the youth, middle-aged, and old-aged individuals own hot-dry, cold-dry, and cold-wet Mizaj, respectively (9, 10).
2. Evidence Acquisition
This review aimed to study the causes of obesity, especially in middle-aged people, according to the new evidence of conventional medicine and findings of traditional Persian medicine (TPM) physicians cited in their books. Databases including PubMed, Scopus, and Iran Medex were also searched with keywords obesity and overweight for recent evidence in conventional medicine.
3. Results
3.1. Obesity in Viewpoint of Avicenna
Obesity, in the viewpoint of Avicenna is regarded as the disease of structure and amount, in which the body increases in quantity. Saman-e-mofrat or overt obesity is considered a disease because it per se disturbs normal body function and may be complicated with other disorders. Overt obesity results in the limitation of body movements, wastes accumulation, and disturbance in vital body function (10).
3.1.1. Dystemperament Approach
Soo-e-Mizaj or dystemperament (diathesis) is the imbalance of Mizaj in an organ, leading to disturbance in the normal function of the afflicted body organ (11).
3.1.1.1. Temperament of Age Groups
The human being is firstly developed from the penetration of the male sperm in the female ovule in the fetal period that is the transmission of innate heat and intrinsic moisture from the parents, according to the description of physicians of Persian medicine. According to the TPM theory, life expectancy is directly related to the degree of intrinsic moisture, and accordingly, innate heat is acquired from the parents, and the maintenance of the intrinsic heat warrants longevity. Death is the result of innate moisture depletion or innate heat quench by diseases or fatal casualties (12). Regarding the quality and quantity of intrinsic heat and moisture, human life is divided into four stages:
- Growth period: It starts with birth and ends near 30-years-old, which is characterized by growth and accordingly higher amounts of intrinsic moisture and heat. A newborn possesses the most amounts of moisture and consequently the most degree of growth due to the highest amounts of heat production. Persian physicians believe that an imbalance between moisture and heat may cause failure to thrive in childhood.
- Youth period: It includes the age range of 30 - 40 years with a balanced ratio of moisture to heat in which the heat quality is like childhood heat quality, but the intrinsic moisture is lower than in childhood. This implicates growth to stop and dominance of hotness and dryness in the youth period.
- Middle age period: It is the age range of 40 - 60 years in which body stamina gradually diminishes because of the decreasing amount of heat and moisture quantitatively and qualitatively.
- Old age period: It includes the age of 60 years and higher in which stamina and strength diminish apparently, and intrinsic heat and moisture are in the least level compared to the other life periods, which leads to GI weakness and consequently, disturbing absorption of essential elements and nutrients (10, 12, 13).
3.1.1.2. Causes of Obesity Based on Temperament Theory
According to TPM sources, obesity can be considered as a disease belonging to all the aforementioned groups of diseases. As a point of fact, the main cause of obesity is increasing moisture in the body, whether it is because of fattiness (cold-wet temperament) or muscularity (hot-wet temperament). Accordingly, obesity may be regarded as a diathesis or dystemperament with an abundance of moisture (13, 14).
According to Avicenna's view in the Canon of Medicine, everybody needs food to replace the substances that are lost in the process of metabolism and physical activity. Hararat-e-qarizi or innate heat is needed for all of these processes (15, 16). In middle age, the innate heat is lower than in young age although it is still more than in elderly. For this reason, the accumulation of humidity is more prominent in middle age than in younger age because of diminishing innate heat and accordingly decreasing physical activity and total body metabolism. Meanwhile, their retentive force is not yet compromised compared to the elderly (15, 16). In the elderly, the retentive force is attenuated, and the depletion of body substances (energy loss) is greater than in middle-aged persons and young adults. Decreased intrinsic force and intact retentive force seem to be the main cause of obesity in middle age (12, 15).
3.1.2. Lifestyle Modification in Obesity
In general, medieval Persian physicians recommend nutritional measures and proper physical activity for obesity control. Avicenna and other TPM physicians believe in the importance of correcting the lifestyle and decreasing the calorie intake as the first step of obesity management. Decreasing the volume and calories of the meals should be observed; however, it should be gradual and with precaution regarding patients’ stamina and tolerance (13).
Barley bread, hot spices, herbal medicines in meals, vegetables, and grains, salty, and hot taste dry foods are considered slimming foods because of dehumidifying effects on the body moisture. Bitter foods are usually low-calorie foods with the least nutritional value, but they usually possess medicinal and calefactory effects. Bitter taste foods extenuate and segmentate the body phlegm and partially compensate for the harmful effects of sweets (13). Hot-tempered condiments usually heat up the body even more than bitter foods. These foods disintegrate and extenuate dense foods like bitter foods. Umami (tasteless) foods like cucumber and squash induce coldness and humidity in the body and should be used with modificators like hot and bitter condiments (13). Avoiding indulgence in meat and sweets consumption should be recommended to middle-aged groups. Foods that are both fatty and sweet like halva are considered dense foods and usually take a long time to be digested. Sour foods like vinegar have slimming effects, but their excessive consumption should be prohibited because they cause coldness of the liver and consequently phlegm accumulation in the body, leading to obesity (13).
Physical activity is a crucial issue regarding obesity control; however, the attenuation of innate heat and declining body metabolism of middle-aged people may limit their capabilities in increasing physical activity as well as young adults. Since decreasing weight needs enormous exercise and intensive physical activities, considering middle-aged limitations, the physical activity programs should be tailored based on the tolerance and stamina of the individuals by increasing the heart rate without prevailing extreme fatigue (17). As Avicenna mentions in the Canon of Medicine, a sedentary lifestyle and indulgence in sleep lead to the accumulation of moisture and phlegm in the body. On the other hand, middle-aged people need less sleep to maintain their body homeostasis and should avoid too much sleep (13).
3.1.3. Herbal Remedies in Obesity Management from the Perspective of TPM
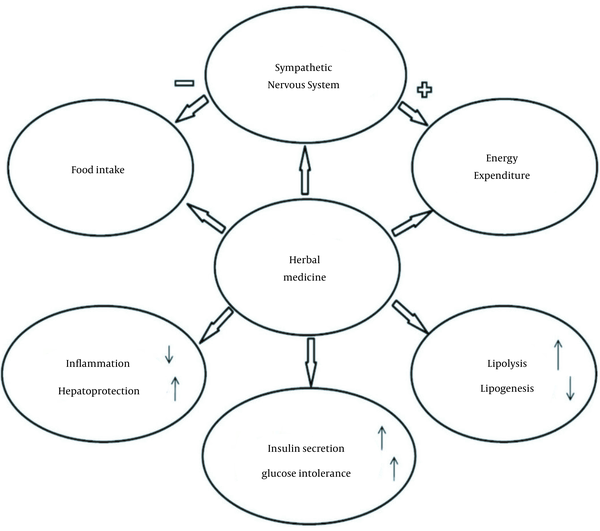
Evidence has shown that herbal medicine may be effective in obesity management, but the mechanisms are not explicit. Many herbal medicines with potential weight loss effect were mentioned in TPM sources. As shown in Table 1, there are different herbal types with different implications (18, 19). Accordingly, Figure 1 shows the potential mechanisms of herbal medicine for obesity management.
Herbal Remedies in Obesity Management
| Family | Scientific Name | Traditional Persian Name | Temperament | Part Used | Usage Form |
|---|---|---|---|---|---|
| Rutaceae | Ruta graveolens L. | Sodab | Hot and dry | Seed/leaves | Edible |
| Rubiaceae | Coffea arabica L. | Bonn’ | Hot and dry | Seed | Edible |
| Oleaceae | Olea europaea L. | Zaytoon | Hot and dry | Fruit | Edible |
| Papilionaceae | Trachylobium horneannianum Hayne. | Sandaros | Hot and dry | Resin | Edible |
| Poaceae | Hordeum vulgare L. | Shaeer | Cold and dry | Seed | Edible |
| 1-Combretaceae, 2-Combretaceae, 3-Phyllanthaceae | 1-Terminalia chebula, 2-Terminalia bellerica, 3-Emblica officinalis | Itrifal e Saghir (comprises three compounds) | Cold and dry | Fruit | Edible |
| Apiaceae | Trachyspermum ammi | Nankhah | Hot and dry | Seed | Edible |
| Piperaceae | Piper nigrum L. | Felfel | Hot and dry | Seed | Edible |
| Umbelliferae | Bonium persicum | Kammun | Hot and dry | Seed | Edible |
| Umbelliferae | Apium graveolens L. | Karafs | Hot and dry | Seed | Edible |
| Umbelliferae | Foeniculum vulgare | Razianaj | Hot and dry | Seed | Edible |
| Umbelliferae | Pimpinella anisum L. | Anisun | Hot and dry | Seed | Edible |
| Lamiaceae | Zataria multiflora | Sa'tar | Hot and dry | leaves | Edible |
| Lamiaceae | Origanum majorana L. | Marzanjush | Hot and dry | leaves | Edible |
| Lamiaceae | Allium sativum | Sou’m | Hot and dry | Bulb | Topical/edible |
| Vitaceae | Vitis vinifera L. | Khall’ | Cold and dry | Fruit vinegar | Topical/edible |
| Moraceae | Ficus laccifera Roxb. | Lok’e maghsul | Hot and dry | Resin | Topical |
| Costaceae | Costus sp. | Ghost | Hot and dry | Roots | Topical |
| Compositae | Matricaria chamomilla | Babubadj | Hot and dry | Flower /leaves | Topical |
| Apiaceae | Anethum graveolens | Shebatt | Hot and dry | leaves | Topical |
Potential mechanisms of herbal medicine for obesity management
3.1.4. Climate in Obesity Management from the Perspective of TPM
Avicenna states that there is an inward flux of heat from the body surface toward the internal organs in the cold seasons. It results in a better metabolism and gastrointestinal (GI) functionality in the cold seasons compared to warm seasons. In the cold season, vasoconstriction keeps the intrinsic heat in the inner parts of the body, which facilitates better waste evacuation out of the body by defecation and urination (13). The temperament of people in related places is affected by different climates and different geographical regions. Accordingly, people living in mountains and high altitudes have cold-dry Mizaj and people living in places located between the sea in the north and mountains in the south have cold-wet Mizaj. Besides, people living in the desert and tropical regions accede to hot-dry and hot-wet Mizaj, respectively (13).
3.2. Obesity in Modern Nutrition and Science
3.2.1. Brown and White Adipose Tissue
Experimental animal studies strongly suggest an inverse association between the propensity of white to brown adipose tissue and the increased chance of diet-related obesity in rodents (20). In cold exposure, the hypothalamic thermoregulatory area receives impulses from dermal cold receptors leading to norepinephrine release by the sympathetic nerve terminals which activates brown adipose tissue (BAT) thermogenic process and increasing lipolysis (21). Besides, BAT increases the expression of type 2 deiodinase, which converts t4 to t3. A high-calorie diet and certain nutrients can activate BAT in rodents that seem to act as a protective factor in dealing with calorie/diet-induced obesity (21). Ozguven et al. found that activated brown adipose tissue quantity positively affects the liver function test and lipid profile in adults. Also, BAT can reduce total cholesterol and LDL levels but it has no effect on the level of HDL and triglyceride (22).
As known, BAT possesses an enriched innervation with the sympathetic nervous system; it is highly vascularized and contains many droplets of lipids and numerous mitochondria compared to white adipocytes that contain a single large droplet and a few mitochondria (21). Mice on a high-fat diet deficient in tryptophan hydroxylase 1, a serotonin regulator, are protected from obesity and non-alcoholic fatty liver (23). Cold exposure increases BAT thermogenesis through sympathetic activity and norepinephrine release (24). It seems that the thermogenic activity of BAT is because of a high amount of mitochondria and uncoupling protein 1 expression (21).
White adipose tissue (WAT), the most abundant adipose tissue in the body, contributes a major role in the regulation of body energy expenditure and serves as a reservoir for excess fat intake (25). Increasing peripheral serotonin is related to obesity based on new research (23). There is a relationship between the depots of adipose tissues and the risk of cardiovascular disease (CVD): Adipose tissue depots in BAT and thoracic perivascular adipose tissue (PVAT) are protective, and abdominal PVAT and WAT increase the risk of CVD (25).
3.2.2. Diet and Energy Expenditure
Following the industrial revolution and the arrival of advanced agricultural machinery, processed food came into a routine diet and greatly changed the caloric intake compared to the previous decades (26). These changes increased inclination to the consumption of higher-calorie foods with lower nutritional values and consequently lower use of fresh green vegetables and fruits (27). The result has been lower physical activity and a sedentary lifestyle accompanied by taking high calorie foods containing high amounts of fat (28). Higher income and urbanization of societies led to the replacement of traditional foods by high amounts of complex carbohydrates and fibers by high-calorie foods including simple carbohydrates, fats, and processed animal products. It is a general assumption that diets containing > 30% of fat can induce obesity in the community (29).
There are few studies pertaining to energy expenditure and weight control. As a matter of fact, overweight, as a kind of energy imbalance, arises when energy intake is more than energy expenditure (30). Adding capsaicin to meals causes satiety and may be effective in the control of obesity through decreasing calorie intake (30). Propionyl L-carnitine (PLC) contributes to cellular energy expenditure and fatty acid oxidation, and it may have a protective effect on the vascular endothelium (31). An animal study showed that PLC could lower the weight of obese rats (31). The major source of adenosine triphosphate (ATP) production is mitochondria (32). Besides, body heat starts to diminish with increasing age, which is more obvious in the elderly; however, increasing weight is a warning sign in middle age. Thermogenic herbal medicines such as Safflower are suitable remedies for weight control. Safflower simultaneously could control constipation, according to PM sources (33).
3.2.3. Microbiota and Energy Homeostasis in Obesity Management
The gut microbiome has been considered a promoter (booster) agent among the factors affecting obesity, i.e., nutrition, lifestyle, genetics, and environment. Microbiota is identified in Merriam-Webster as any “microscopic organisms (including bacteria, archaea, protists, fungi, and viruses) of a particular environment”. Some investigations have shown that the human’s microbiota populations, up to 100 trillion microbes, are composed of five phyla, including Bacteroidetes, Firmicutes, Actinobacteria, Proteobacteria, and Verrucomicrobia (34). Gut microbiota contributes to a symbiosis with human hosts and plays a crucial role in energy homeostasis and metabolism. The relative size of Firmicutes versus Bacteroidetes population, the dominant phyla of human guts, has an association with obesity in rodents (35). Bacteroidetes and Firmicutes form around 90% of the total bacterial species (34, 36). Gut microbiota is known as a collection of microorganisms located in the gastrointestinal tract. Besides the hosted nature, endogenous and exogenous events can affect and modify the compositions of this microbial population (37).
During the past decades, a significant correlation has been found between gut microbiota and obesity, but the relations between them remain unknown. It has been shown that the pattern of the bacterial population varies between lean and obese people so that the number of Firmicutes increases in obese and type 2 diabetic patients (36-40) although later studies failed to confirm this finding (41). Some studies revealed significantly higher diversity of microbiota among obese individuals. Recent studies found different intestinal microbiomes in obese and non-obese individuals (42). However, it should be noted that intestinal bacteria play an important role in providing energy and regulating host metabolism (43) by decomposition of plant polysaccharides and fibers (44). More specifically, Le Chatelier et al. showed that individuals with a low diversity of gut microbiota are more likely to develop diseases such as overall adiposity, insulin resistance, and dyslipidemia than those with high bacterial richness. This finding demonstrates that the composition of the gut microbiome and diversity of intestinal flora determine the healthy/diseased states (45). The difference between gut microbiomes in adolescents and adults and their relationships with obesity or weight loss is controversial. Recent studies showed the distinct microbiota of obese adolescents and adults compared to the non-obese population, which implies the synergistic impacts of the microbiome and increasing age on the development of middle-aged obesity. Faecalibacterium prausnitzii is one of the most important bacteria presented in the western world diet that plays a role in the failure of obese people in losing weight. It is also an important factor in host metabolism, which facilitates the absorption of non-absorbable carbohydrates in the gut (46, 47).
4. Conclusions
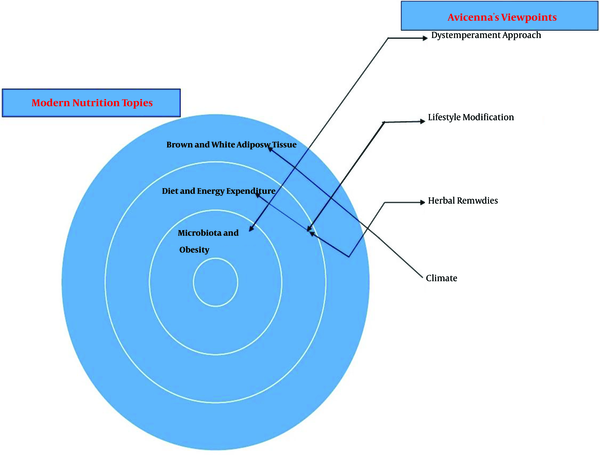
Obesity in middle age is influenced by Mizaj. In this regard, the traditional theory may help to explore for better understanding obesity management. Obesity in middle age can enhance the likelihood of metabolic syndrome and increase the risk of CVD. The increase of food intake and decrease of the basal metabolic rate can enhance the prevalence of overweight and obesity in middle age. Considering this new approach towards obesity, it is influenced by diverse factors such as brown adipose tissue, energy expenditure, climate, habit, diet, microbiota, homeostasis, hormones, and epigenetics. In addition, temperament equilibrium based on the Avicenna theory can have an important effect on obesity in middle age. Therefore, it is essential to explore other theories to improve obesity management (Figure 2).
Potential conceptual relationship between traditional Persian medicine and modern nutrition in obesity
Based on traditional medicine findings, dystemprament or disequilibrium in Mizaj may promote obesity in middle-aged and elderly people. Middle-aged individuals possess less innate heat compared to youngsters, and it is an implication for decreasing their physical activity and transforming their excess calorie needs to abdominal PVT and WAT, which is a risk factor for CVD. On the other hand, scientific evidence shows that age is one of the most important factors in energy metabolism. The basal metabolic rate drops almost linearly with age. The decrease in the basal metabolic rate generally requires a reduction in calorie intake (48). In addition, skeletal musculature is a fundamental organ that consumes the most energy in the normal human body. As a result of aging, skeletal muscles deterioration takes place, which includes enhanced intramuscular fat infiltration, fibrosis, and a decline in the size and amount of muscle fibers (25, 46, 49). Interestingly, Jorjani, in his great book, Treasure of Kharazm Shahi, describes hot-wet-tempered individuals with wide chests and necks (50). It is in line with recent studies that cite protective effects of depots of BAT in the neck and thoracic PVAT for CVD (25). According to TPM sources, people living in high altitudes and cold-dry climates maintain their innate heat better, which is in accordance with increasing BAT thermogenesis in cold exposure.
There is a correlation between the density of the Bactroidetes population in the gut and fecal concentrations of short-chain free fatty acids (butyrate, acetate, and propionate), which contribute to energy homeostasis. They serve as energy sources for the liver and peripheral tissues, which are diminished in obese people. Short-chain free fatty acids bind to free fatty acid receptor 3 in the gut, which, in turn, activates the sympathetic nervous system (35).
Considering TPM manuscripts and recent studies, hot-tempered individuals show higher sympathetic nervous system activity than cold-tempered people (51). According to TPM sources, hot-dry-tempered people are usually slimmer compared to cold-wet-tempered individuals. In sum, it seems that cold-tempered people have lower basal metabolic rates and more efficient energy homeostasis in comparison with hot-tempered people who are similar to those with Firmicutes gut microbiota predominance. They usually have more inclination to weight gain than people with Bactroidetes gut microbiota predominance, which lose weight easier. More recently, it has been reported that temperament (mood and behavior) was associated with gut microbiota (52). Based on TPM texts, the individuals’ temperament is associated with their Mizaj, so one can assume a relationship between gut microbiota and temperament. However, further research should be conducted to prove the relation of gut microbiota with Mizaj and BMI.
Nowadays, the use of herbal medicine to treat obesity is of much attention. Unfortunately, there are scarce studies about the active ingredients of herbal medicine and their mechanism of action so far. However, some studies suggest that weight-reducing effect of some herbal preparation might be via reducing endoplasmic reticulum stress and increasing leptin sensitivity or through decreasing cytokine expression in the liver and adipose tissue (53).
As TPM is a holistic approach to medicine, its proposed interventions for obesity and overweight need a similar look. The TPM physicians treat most diseases according to the diagnosis of Mizaj that is the diagnosis of quadruple qualities – hotness, coldness, wetness, and dryness – and includes Mizaj of the patient, Mizaj of the disease state, Mizaj of prescribed medicinal herbs, and Mizaj of the season and place in the time of disease state. In sum, considering the average data deduced from Mizaj parameters, it determines the plan of the physicians for the start-point and endpoint of medical intervention and diagnosis. Obesity and overweight in conventional medicine have multiple etiologies comprised genotype and gene expression, microbiota, socioeconomic status, diet, environment, and psychological factors. It seems that there may be a correlation between cold/wet Mizaj and some risk factors of obesity, including microbiota. Moreover, based on TPM school basics, it is hypothesized that increasing age and diminishing innate heat besides the accumulation of phlegm (moisture) in the GI tract of middle-aged individuals may be influential in altering gut microbiota and consequently obesity. Conducting well-designed experimental studies and clinical trials will shed light on these claims.
References
-
1.
World Health Organization. Obesity: Preventing and managing the global epidemic: Report of a WHO consultation on obesity. Geneva, Switzerland: World Health Organization; 1997.
-
2.
Kaplan JL, Walker WA. Early gut colonization and subsequent obesity risk. Curr Opin Clin Nutr Metab Care. 2012;15(3):278-84. [PubMed ID: 22327336]. https://doi.org/10.1097/MCO.0b013e32835133cb.
-
3.
Ades PA, Savage PD. Obesity in coronary heart disease: An unaddressed behavioral risk factor. Prev Med. 2017;104:117-9. [PubMed ID: 28414064]. [PubMed Central ID: PMC5640469]. https://doi.org/10.1016/j.ypmed.2017.04.013.
-
4.
Wang J, Tang H, Zhang C, Zhao Y, Derrien M, Rocher E, et al. Modulation of gut microbiota during probiotic-mediated attenuation of metabolic syndrome in high fat diet-fed mice. ISME J. 2015;9(1):1-15. [PubMed ID: 24936764]. [PubMed Central ID: PMC4274436]. https://doi.org/10.1038/ismej.2014.99.
-
5.
Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10(1):22. [PubMed ID: 23167948]. [PubMed Central ID: PMC3543235]. https://doi.org/10.1186/1478-7954-10-22.
-
6.
Rahmani A, Sayehmiri K, Asadollahi K, Sarokhani D, Islami F, Sarokhani M. Investigation of the prevalence of obesity in Iran: A systematic review and meta-analysis study. Acta Med Iran. 2015;53(10):596-607. [PubMed ID: 26615371].
-
7.
Chen HH, Tseng YJ, Wang SY, Tsai YS, Chang CS, Kuo TC, et al. The metabolome profiling and pathway analysis in metabolic healthy and abnormal obesity. Int J Obes. 2015;39(8):1241-8. [PubMed ID: 25907313]. https://doi.org/10.1038/ijo.2015.65.
-
8.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766-81. [PubMed ID: 24880830]. [PubMed Central ID: PMC4624264]. https://doi.org/10.1016/S0140-6736(14)60460-8.
-
9.
Chiappelli F, Prolo P, Cajulis OS. Evidence-based research in complementary and alternative medicine I: History. Evid Based Complement Alternat Med. 2005;2(4):453-8. [PubMed ID: 16322801]. [PubMed Central ID: PMC1297495]. https://doi.org/10.1093/ecam/neh106.
-
10.
Nimrouzi M, Salehi A, Kiani H. Avicenna's medical didactic poem: Urjuzehtebbi. Acta Med Hist Adriat. 2015;13 Suppl 2:45-56. [PubMed ID: 26959631].
-
11.
Shirbeigi L, Zarei A, Naghizadeh A, Vaghasloo MA. The concept of temperaments in traditional Persian medicine. Trad Integr Med. 2017;2(3):143-56.
-
12.
Nimrouzi M, Zarshenas MM. Management of anorexia in elderly as remarked by medieval Persian physicians. Acta Med Hist Adriat. 2015;13 Suppl 2:115-28. [PubMed ID: 26959636].
-
13.
Avicenna H. [The Canon of medicine]. Tehran, Iran: University of Tehran Publishing; 1978. Persian.
-
14.
Nimrouzi M, Zarshenas MM. Functional constipation in children: non-pharmacological approach. J Integr Med. 2015;13(2):69-71. [PubMed ID: 25797636]. https://doi.org/10.1016/S2095-4964(15)60152-2.
-
15.
Vaghasloo MA, Naghizadeh A, Babashahi N. The concept of the Haar-re-Gharizi and Hararate Gharizi: The innate hot [Substance] and heat. Trad Integr Med. 2017;2(1):3-8.
-
16.
Nimrouzi M, Bemani M, Zare M, Zazerani M, Soltanabadi N, Fathi M, et al. [Role of body temperature on health: Traditional and conventional]. Medical History. 2014;6(19):29-44. Persian.
-
17.
Ebadiani M, Siahpoosh MB, Nasrabadi AN, Hosseini GS, Isfahani MM. Rhazes’s opinion about relationship between physical activity and eating food. Trad Integr Med. 2017;2(3):99-101.
-
18.
Kamali SH, Khalaj AR, Hasani-Ranjbar S, Esfehani MM, Kamalinejad M, Soheil O, et al. Efficacy of 'Itrifal Saghir', a combination of three medicinal plants in the treatment of obesity; A randomized controlled trial. Daru. 2012;20(1):33. [PubMed ID: 23351558]. [PubMed Central ID: PMC3559014]. https://doi.org/10.1186/2008-2231-20-33.
-
19.
Azam Khan M. [The great elixir]. Tehran, Iran: Institute of Meical History, Islamic Medicine and Complementary Medicine; Iran Medical University; 2008. Persian.
-
20.
Sidossis L, Kajimura S. Brown and beige fat in humans: Thermogenic adipocytes that control energy and glucose homeostasis. J Clin Invest. 2015;125(2):478-86. [PubMed ID: 25642708]. [PubMed Central ID: PMC4319444]. https://doi.org/10.1172/JCI78362.
-
21.
Betz MJ, Enerback S. Human brown adipose tissue: What we have learned so far. Diabetes. 2015;64(7):2352-60. [PubMed ID: 26050667]. https://doi.org/10.2337/db15-0146.
-
22.
Ozguven S, Ones T, Yilmaz Y, Turoglu HT, Imeryuz N. The role of active brown adipose tissue in human metabolism. Eur J Nucl Med Mol Imaging. 2016;43(2):355-61. [PubMed ID: 26283505]. https://doi.org/10.1007/s00259-015-3166-7.
-
23.
Crane JD, Palanivel R, Mottillo EP, Bujak AL, Wang H, Ford RJ, et al. Inhibiting peripheral serotonin synthesis reduces obesity and metabolic dysfunction by promoting brown adipose tissue thermogenesis. Nat Med. 2015;21(2):166-72. [PubMed ID: 25485911]. [PubMed Central ID: PMC5647161]. https://doi.org/10.1038/nm.3766.
-
24.
Cypess AM, Weiner LS, Roberts-Toler C, Franquet Elia E, Kessler SH, Kahn PA, et al. Activation of human brown adipose tissue by a beta3-adrenergic receptor agonist. Cell Metab. 2015;21(1):33-8. [PubMed ID: 25565203]. [PubMed Central ID: PMC4298351]. https://doi.org/10.1016/j.cmet.2014.12.009.
-
25.
van Dam AD, Boon MR, Berbee JFP, Rensen PCN, van Harmelen V. Targeting white, brown and perivascular adipose tissue in atherosclerosis development. Eur J Pharmacol. 2017;816:82-92. [PubMed ID: 28347739]. https://doi.org/10.1016/j.ejphar.2017.03.051.
-
26.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3-21. [PubMed ID: 22221213]. [PubMed Central ID: PMC3257829]. https://doi.org/10.1111/j.1753-4887.2011.00456.x.
-
27.
Slavin JL, Lloyd B. Health benefits of fruits and vegetables. Adv Nutr. 2012;3(4):506-16. [PubMed ID: 22797986]. [PubMed Central ID: PMC3649719]. https://doi.org/10.3945/an.112.002154.
-
28.
Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131(3):871S-3S. [PubMed ID: 11238777]. https://doi.org/10.1093/jn/131.3.871S.
-
29.
Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B Biol Sci. 2010;365(1554):2793-807. [PubMed ID: 20713385]. [PubMed Central ID: PMC2935122]. https://doi.org/10.1098/rstb.2010.0149.
-
30.
Janssens PL, Hursel R, Westerterp-Plantenga MS. Capsaicin increases sensation of fullness in energy balance, and decreases desire to eat after dinner in negative energy balance. Appetite. 2014;77:44-9. [PubMed ID: 24630935]. https://doi.org/10.1016/j.appet.2014.02.018.
-
31.
Mingorance C, Duluc L, Chalopin M, Simard G, Ducluzeau PH, Herrera MD, et al. Propionyl-L-carnitine corrects metabolic and cardiovascular alterations in diet-induced obese mice and improves liver respiratory chain activity. PLoS One. 2012;7(3). e34268. [PubMed ID: 22457831]. [PubMed Central ID: PMC3311627]. https://doi.org/10.1371/journal.pone.0034268.
-
32.
Harper ME, Seifert EL. Thyroid hormone effects on mitochondrial energetics. Thyroid. 2008;18(2):145-56. [PubMed ID: 18279015]. https://doi.org/10.1089/thy.2007.0250.
-
33.
Toma W, Guimarães LL, Brito ARMS, Santos AR, Cortez FS, Pusceddu FH, et al. Safflower oil: An integrated assessment of phytochemistry, antiulcerogenic activity, and rodent and environmental toxicity. Rev Bras Farmacogn. 2014;24(5):538-44. https://doi.org/10.1016/j.bjp.2014.09.004.
-
34.
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464(7285):59-65. [PubMed ID: 20203603]. [PubMed Central ID: PMC3779803]. https://doi.org/10.1038/nature08821.
-
35.
Rosenbaum M, Knight R, Leibel RL. The gut microbiota in human energy homeostasis and obesity. Trends Endocrinol Metab. 2015;26(9):493-501. [PubMed ID: 26257300]. [PubMed Central ID: PMC4862197]. https://doi.org/10.1016/j.tem.2015.07.002.
-
36.
Tang WH, Kitai T, Hazen SL. Gut microbiota in cardiovascular health and disease. Circ Res. 2017;120(7):1183-96. [PubMed ID: 28360349]. [PubMed Central ID: PMC5390330]. https://doi.org/10.1161/CIRCRESAHA.117.309715.
-
37.
Sekirov I, Russell SL, Antunes LC, Finlay BB. Gut microbiota in health and disease. Physiol Rev. 2010;90(3):859-904. [PubMed ID: 20664075]. https://doi.org/10.1152/physrev.00045.2009.
-
38.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: Human gut microbes associated with obesity. Nature. 2006;444(7122):1022-3. [PubMed ID: 17183309]. https://doi.org/10.1038/4441022a.
-
39.
Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102(31):11070-5. [PubMed ID: 16033867]. [PubMed Central ID: PMC1176910]. https://doi.org/10.1073/pnas.0504978102.
-
40.
Karlsson FH, Tremaroli V, Nookaew I, Bergstrom G, Behre CJ, Fagerberg B, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99-103. [PubMed ID: 23719380]. https://doi.org/10.1038/nature12198.
-
41.
Walters WA, Xu Z, Knight R. Meta-analyses of human gut microbes associated with obesity and IBD. FEBS Lett. 2014;588(22):4223-33. [PubMed ID: 25307765]. [PubMed Central ID: PMC5050012]. https://doi.org/10.1016/j.febslet.2014.09.039.
-
42.
Del Chierico F, Abbatini F, Russo A, Quagliariello A, Reddel S, Capoccia D, et al. Gut microbiota markers in obese adolescent and adult patients: Age-dependent differential patterns. Front Microbiol. 2018;9:1210. [PubMed ID: 29922272]. [PubMed Central ID: PMC5996250]. https://doi.org/10.3389/fmicb.2018.01210.
-
43.
Clarke SF, Murphy EF, Nilaweera K, Ross PR, Shanahan F, O'Toole PW, et al. The gut microbiota and its relationship to diet and obesity: New insights. Gut Microbes. 2012;3(3):186-202. [PubMed ID: 22572830]. [PubMed Central ID: PMC3427212]. https://doi.org/10.4161/gmic.20168.
-
44.
Chiu CM, Huang WC, Weng SL, Tseng HC, Liang C, Wang WC, et al. Systematic analysis of the association between gut flora and obesity through high-throughput sequencing and bioinformatics approaches. Biomed Res Int. 2014;2014:906168. [PubMed ID: 25202708]. [PubMed Central ID: PMC4150407]. https://doi.org/10.1155/2014/906168.
-
45.
Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541-6. [PubMed ID: 23985870]. https://doi.org/10.1038/nature12506.
-
46.
Haro C, Rangel-Zuniga OA, Alcala-Diaz JF, Gomez-Delgado F, Perez-Martinez P, Delgado-Lista J, et al. Intestinal microbiota is influenced by gender and body mass index. PLoS One. 2016;11(5). e0154090. [PubMed ID: 27228093]. [PubMed Central ID: PMC4881937]. https://doi.org/10.1371/journal.pone.0154090.
-
47.
Kasai C, Sugimoto K, Moritani I, Tanaka J, Oya Y, Inoue H, et al. Comparison of the gut microbiota composition between obese and non-obese individuals in a Japanese population, as analyzed by terminal restriction fragment length polymorphism and next-generation sequencing. BMC Gastroenterol. 2015;15:100. [PubMed ID: 26261039]. [PubMed Central ID: PMC4531509]. https://doi.org/10.1186/s12876-015-0330-2.
-
48.
Shimokata H, Kuzuya F. [Aging, basal metabolic rate, and nutrition]. Nihon Ronen Igakkai Zasshi. 1993;30(7):572-6. Japanese. [PubMed ID: 8361073]. https://doi.org/10.3143/geriatrics.30.572.
-
49.
Yoon MA, Hong SJ, Ku MC, Kang CH, Ahn KS, Kim BH. Multiparametric MR imaging of age-related changes in healthy thigh muscles. Radiology. 2018;287(1):235-46. [PubMed ID: 29239712]. https://doi.org/10.1148/radiol.2017171316.
-
50.
Jorjani E. [Treasure of Kharazm Shah]. 1st ed. Tehran, Iran: Iranian Medical Academy; 2001. Persian.
-
51.
Abbasnezhad A, Masoumzadeh M, Rasekhi H, Irani H, Kianmehr M. The effect of hot-and cold-natured foods on the vital signs in the human. Indian J Forensic Med Toxicol. 2019;13(1):344. https://doi.org/10.5958/0973-9130.2019.00067.7.
-
52.
Aatsinki AK, Lahti L, Uusitupa HM, Munukka E, Keskitalo A, Nolvi S, et al. Gut microbiota composition is associated with temperament traits in infants. Brain Behav Immun. 2019;80:849-58. [PubMed ID: 31132457]. https://doi.org/10.1016/j.bbi.2019.05.035.
-
53.
Liu Y, Sun M, Yao H, Liu Y, Gao R. Herbal medicine for the treatment of obesity: An overview of scientific evidence from 2007 to 2017. Evid Based Complement Alternat Med. 2017;2017:8943059. [PubMed ID: 29234439]. [PubMed Central ID: PMC5632873]. https://doi.org/10.1155/2017/8943059.