Abstract
Abstract:
Hydatid disease is caused by Echinococcus spp. especially Echinococcus granulosus that is the most common cause of hydatid disease in humans. This disease occurs either through direct contact with infected dogs or indirectly from the ingestion of contaminated water or food with eggs of worms. The most common site in human is the liver (59-75%), followed in frequency by lung (27%), kidney (3%) and bone (1-4%). The authors report a case of the pelvic bone hydatidosis in a 27-years old patient, appearing with pain and a mass in the pelvic region.Keywords
1. Introduction
Hydatid disease is still endemic in several regions including Iran (1, 2, 3).Though skeletal involvements are usually secondary to hepatic or pulmonary hydatidosis, but maybe, occurs as the primary disease. The most commonly affected sites in bone are the vertebrae, pelvis, and the skull. The vertebrae are the most commonly affected ones (50%), followed by the pelvis (25%) and the long bones (15-25%) (4). This disease can present as a solitary or polycystic disease. In both types of hydatid cyst, pressure absorption of the bone, in addition thinning and fracturing and extension through the soft tissues occurs (5). Hydatid disease of the bone is often asymptomatic for a long duration and is usually detected after a sudden fracture, secondary infection or neurovascular impingement Hydatid disease is caused by Echinococcus spp. especially Echinococcus granulosus that is the most common cause of hydatid disease in humans. This disease occurs either through direct contact with infected dogs or indirectly from the ing estion of contaminated water or food with eggs of worms. The most common site in human is the liver (59-75%), followed in frequency by lung (27%), kidney (3%) and bone (1-4%). The authors report a case of the pelvic bone hydatidosis in a 27-years old patient, appearing with pain and a mass in the pelvic region. caused by compression (6, 7). Progressive changes may resemble tumor formation with an expansive cystic appearance. A definite preoperative diagnosis without histological examination is often difficult, as there are not pathognomonic signs. There are no specific radiographic signs in affected bone; in the later stages, lytic lesions with trabeculated pattern, with or without sclerosis May be seen. Radiographic findings, perhaps misdiagnosed as those of other lesions and immunologic test, are of limited value (8).
2. Case Report
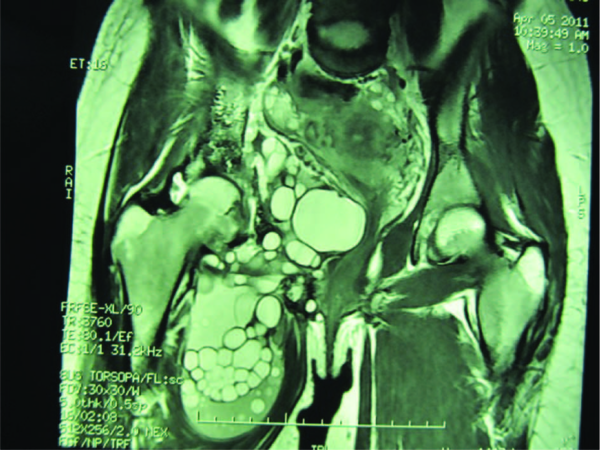
A 27-years old woman presented with a three-month history of a pain and a mass in the pelvic region prominent in right lower quadrant extended to near symphysis pu-bis. Pain relieved only by administration of narcotics (9). She first was referred to this center for tumor work-up and management of an aggressive tumor; but by paraclinical studies we found she may be affected by hydatidosis. Radiologic study revealed multiple lytic lesion of right superior and inferior pubic rami with no reactive sclerosis (Figure 1). MRI and CT scan showed also multiple cysts in bones of rami, ischium and their surrounded soft tissues (Figure 2). Bone hydatid disease lacks a typical linical appearance and image characteristics on an x ray or CT scan are similar to those of tuberculosis, metastases and giant cell tumor or bone cysts. However, MRI does show distinctive diagnostic features of bone hydatid disease, especially in the spine (10) via illioinguinal approach, we saw many translucent cysts of Echinococcus in different sizes.
Destructive Area of Pelvic Bone Especially In Left Side of Hemipelvis

Daugther Cyst Affecting Bone in Bone and Soft Tissues of Pelvis
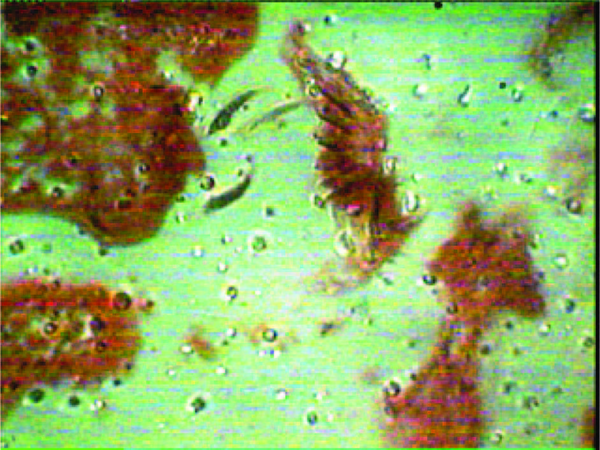
We extracted all cysts and resected involved bone of ramus as possible and the patient's mobility was preserved. We used formalin in the operative field to prevent extension of scolicies of Echinococcus.Histopathological evidences revealed characteristic trilamellar hydatid cystwall and scolices of Echinococcus granulosus scattered amidst fragments of bone and erosion of bone were seen (Figure 3). An ultrasonography of the abdomen and Roentgenography of the chest was performed and did not reveal hydatid cyst in the lung or the liver. The patient was treated with albendazole for three cycles at a dose of 400mg twice a day for six weeks followed by a two- week rest without therapy. The patient was followed for 12 months with no recurrence of the lesion. The disease in the bone and joint begins once the blood-borne scolex settles there. The disease is a very slow process and thus, diseases are seldom diagnosed in the early period of infestation. There are fragmentation and conglomeration of the daughter cyst. The bone has mechanical resistance to cysts. Due to the pressure of the cyst, bone is absorbed and then cyst expands uniformly in the soft tissues. Intervertebral disc has the least resistance to growth (11, 12). The disease must be suspected in cystic lesions of bone, especially in endemic areas such as Iran, as it may easily be mis iagnosed. It can mimic simple bone cyst, tuberculosis, aneurismal bone cyst, giant cell tumors, malignant fibrous histiocytoma, myeloma and chondrosarcoma (10). Diagnosis of bone hydatidosis is based on imaging nd laboratory studies and sometimes is established after surgery (13, 14).
Photomicrograph (100×) Showing Scolex in Pelvic Bone
Hydatid disease of bone is an infiltrating, diffuse, slow and progressive process, all of these characteristics justified the often-delayed diagnosis. Pelvic locations are particularly difficult to treat (15). Because of the poor results with medical treatment, bone hydatidosis must be treated with wide excision (1, 16). The best treatment for bone Echinococcosis is resection of the involved bone or to amputate it. Curettage and instilling solutions such as hypertonic saline, 1% formalin, or 0.5% silver nitrate have been tried. In suspected cases of Echinococcosis, diagnostic biopsy or aspiration is contraindicated. Operative management should include careful planning and meticulous technique to avoid spillage of the cyst contents, which may cause spread of the disease.
0If spillage occurs, the application of cetyltrimethylammonium bromide (Cetrimide), 2% formalin, or 1% iodine can reduce the danger of spreading (17). We used formalin in this patient. The purpose of this article is to alert orthopedic surgeons of this rare condition to emphasize the fact that the disease should be suspected in cystic lesions affecting any organ in the body, especially in endemic areas of the world and open and percutaneous needle biopsies should be avoided in such cases and is a differential diagnosis of cystic tumor in endemic areas.
Acknowledgements
References
-
1.
Arti H, Darani HY. Fibular hydatid cyst. Indian J Orthop. 2007;41(3):244-5. https://doi.org/10.4103/0019-5413.33692.
-
2.
Papanikolaou A. Osseous hydatid disease. Trans R Soc Trop Med Hyg. 2008;102(3):233-8. https://doi.org/10.1016/j.trstmh.2007.09.012.
-
3.
Yuksel M, Demirpolat G, Sever A, Bakaris S, Bulbuloglu E, Elmas N. Hydatid disease involving some rare locations in the body: a pictorial essay. Korean J Radiol. 2007;8(6):531-40. https://doi.org/10.3348/kjr.2007.8.6.531.
-
4.
Calvo AM, Cires JM, Monton S, Sarasibar H, Lasanta P, Artazcoz FJ. [Inguinal tumor: a rare occurrence of hydatid disease. A case report]. An Sist Sanit Navar. 2007;30(3):475-9. https://doi.org/10.4321/S1137-66272007000500013.
-
5.
Khan JA, Devkota P, Acharya BM, Pradhan NM, Shreshtha S. Bony hydatid disease of superior pubic ramus with extension into pelvis and proximal thigh. J Nepal Med Assoc. 2008;47(171):139-41.
-
6.
Kalkan E, Cengiz SL, Cicek O, Erdi F, Baysefer A. Primary spinal intradural extramedullary hydatid cyst in a child. J Spinal Cord Med. 2007;30(3):297-300. [PubMed ID: 17684899].
-
7.
Patond KR, Srivastava SK, Kumar N. Musculoskeletal hydatidosis. India Pract. 1991;54:299-302.
-
8.
Das S, Kalyani R, Kumar U, Kumar HM. A varied presentation of hydatid cyst: a report of four cases with review of literature. Indian J Pathol Microbiol. 2007;50(3):550-2.
-
9.
Arti HR, Mehdinasab SA. The comparison effects of intra-articular injection of different opioids on postoperative pain relieve after arthroscopic anterior cruciate ligament reconstruction: A randomized clinical trial study. J Res Med Sci. 2011;16(9):1176-82. [PubMed ID: 22973386].
-
10.
Song XH, Ding LW, Wen H. Bone hydatid disease. Postgrad Med J. 2007;83(982):536-42. https://doi.org/10.1136/pgmj.2007.057166.
-
11.
Mattern CJ, Gardner MJ, Grose A, Helfet DL. Case report: Echinococcus disease of the bone presenting as a femoral shaft nonunion. Clin Orthop Relat Res. 2007;458:220-5. [PubMed ID: 17159572].
-
12.
Proychev VI, Tzankov A. Solitary hydatid cyst in the tibia. Ann Trop Med Parasitol. 2007;101(6):551-3. [PubMed ID: 17716440]. https://doi.org/10.1179/136485907X193842.
-
13.
Alldred AJ, Nisbet NW. Hydatid Disease of Bone in Australasia. J Bone Joint Surg Br. 1964;46:260-7. [PubMed ID: 14167635].
-
14.
Vasilevska V, Zafirovski G, Kirjas N, Janevska V, Samardziski M, Kostadinova-Kunovska S, et al. Imaging diagnosis of musculoskeletal hydatid disease. Prilozi. 2007;28(2):199-209. [PubMed ID: 18356790].
-
15.
Gdoura F, Trigui M, Zribi W, Ellouze Z, Bouzidi R, Ayedi K, et al. Pelvic bone hydatidosis. Orthop Traumatol Surg Res. 2010;96(1):85-9. https://doi.org/10.1016/j.otsr.2009.04.020.
-
16.
Zlitni M, Ezzaouia K, Lebib H, Karray M, Kooli M, Mestiri M. Hydatid cyst of bone: diagnosis and treatment. World J Surg. 2001;25(1):75-82. https://doi.org/10.1007/s002680020010.
-
17.
Mihalko MJ, Martinez SF. Tuberculosis and other unusual infection. In: Campbell WC, Canale ST, Beaty JH, editors. Campbell's operative orthopaedics. Philadelphia: Penns: Mosby/Elsevier;