Abstract
Background:
Protozoa have the ability to replace the human lung. Over recent years, the incidence of pulmonary infections caused by these microorganisms has increased, particularly in individuals with an immunodeficiency. The use of appropriate diagnostic methods is particularly important in the identification of parasites in pulmonary secretions.Objectives:
The present study aimed to evaluate and compare PCR-based diagnostic methods with the gold standard method to detect three pathogenic protozoa, including Toxoplasma, Cryptosporidium, and Microsporidia in bronchoalveolar lavage (BAL) samples obtained from immunocompromised patients with chronic obstructive pulmonary disease.Methods:
A BAL sample of immunodeficient patients suffering from chronic obstructive pulmonary disease (COPD) was examined by direct microscopy and PCR methods.Results:
In this study, we examined 64 patients with immunodeficiency accompanied by COPD. Microsporidia were not identified in the samples. Direct methods identified three and nine cases of Toxoplasma and Cryptosporidium, respectively. However, the molecular method identified two and two cases of pulmonary infection with these parasites.Conclusions:
Determining the standard diagnostic method for parasites is dependent on factors, such as the type of specimen and the type of parasite. Based on the results of the present study, the direct microscopic method is the optimal diagnostic method for Toxoplasma and Cryptosporidium in BAL samples.Keywords
Bronchoalveolar Lavage (BAL) Immunocompromised Patient Cryptosporidium Chronic Obstructive Pulmonary Disease (COPD) Toxoplasma
1. Background
The potential of protozoan parasites for entry and replacement in the human lung has been reported in some studies (1, 2). Up to now, few cases of respiratory infections caused by parasites have been reported, which may be attributed to the difficulty associated with detecting parasitic agents in respiratory specimens. However, over recent years, there has been an increase in the reports of lung infections caused by parasites (3-5). Most parasitic lung infections are asymptomatic, but it has been reported that if the immune system is weakened, these infections can be accompanied by symptoms (1, 2). The most prevalent parasites causing lung infections are Toxoplasma, Cryptosporidium, and sometimes Acanthamoeba and Microsporidia (1, 2). Researchers have studied the effectiveness of several diagnostic methods for identifying these parasites. For instance, Niyyati et al. (6), Perez-Santonja et al. (7), and Boggild et al. (8) evaluated and compared different diagnostic methods for identifying Acanthamoeba keratitis. Saigal et al. (9) and Khanaliha et al. (10) assessed the direct microscopic and molecular methods for the identification of Microsporidia in fecal samples, and Ozkoc et al. (3) compared the same methods for the identification of the same parasite in bronchoalveolar lavage (BAL) samples.
Mercado et al. (11) compared the potential of the Ziehl Neelsen and molecular methods in the detection of Cryptosporidium in sputum samples. Bourdin et al. (12) investigated the potential of molecular and immunoblotting methods in the diagnosis of Toxoplasma in blood and ocular specimens of patients with ocular toxoplasmosis and compared them with the control group. Lavrard et al. (13) compared the efficiency of three diagnostic methods to detect pulmonary toxoplasmosis in BAL samples. To identify infectious agents in the lung, the appropriate sample is generally the secretion of the lower respiratory tract obtained through the BAL technique (14, 15). Various methods have also been used to identify parasites in lung specimens (2, 3). However, the value of these methods in detecting these parasites is yet to be elucidated in BAL specimens.
2. Objectives
In our country, studies on respiratory parasitic infections are scarce and far between. The present study aimed to evaluate and compare two diagnostic methods to detect some pathogenic protozoa in BAL samples obtained from immunocompromised patients with chronic obstructive pulmonary disease (COPD).
3. Methods
3.1. Sampling
Our study population included those who had both impairments of the immune system and respiratory disorders, approved by specialists. We excluded people who had no respiratory symptoms and people whose impairment of the immune system was not approved.
3.2. Respiratory Secretion Preparation
Written informed consent was obtained from the selected patients, and they completed a questionnaire containing the demographic information and the history of background disease. The pulmonary secretions of each patient were then obtained by the BAL technique (16). Fresh samples were immediately transferred to the laboratory, and the testing process was initiated on them.
3.3. Experiments
3.3.1. Direct Microscopic Diagnosis
Two smears were provided from each sample and stained by Ziehl Neelsen and Giemsa methods for direct microscopic diagnosis. The Ziehl-Neelsen stained smears were used to diagnose Cryptosporidium (1) and Microsporidia (17). The Giemsa stained smears were used to diagnose Toxoplasma (18).
3.3.2. PCR
The remaining samples were used for the PCR assay to diagnose the three protozoan parasites. First, the DNA was extracted by the phenol-chloroform method (19). Afterward, the genus-specific primers of four kinds of protozoa were used for PCR amplification. Table 1 presents the sequences of specific primers to diagnose the parasites. A Master Mix kit (CinnaGen Co.) was used to optimize the PCR assays. A final volume of 25 µL was used for amplification in an Eppendorf thermocycler (Eppendorf AG, Germany). The programs were used according to the following table (Table 2). Finally, the PCR products were assessed by 1.5% agarose under ultraviolet light. Of note, the positive control of Cryptosporidium and Microsporidia was kindly awarded by Dr. Majid Pirestani (Parasitology and Entomology Department, Tarbiat Modares University, Tehran, Iran), and Toxoplasma was provided by Dr. Saeedeh Shojaee (Department of Parasitology, Tehran University of Medical Sciences, Tehran, Iran).
Characteristics of the Primers Used in the Present Study
The PCR Amplification Program for Each Protozoan
| Parasite | Initial Denaturing Temperature (Time) | Number of Amplification Cycles | Denaturing Temperature (Time) | Annealing Temperature (Time) | Extension Temperature (Time) | Final Extension Temperature (Time) |
|---|---|---|---|---|---|---|
| Toxoplasma | 94°C (5 min) | 35 | 94°C (30 s) | 58°C (30 s) | 72°C (30 s) | 72°C (10 min) |
| Cryptosporidium | 94°C (5 min) | 32 | 94°C (45 s) | 55°C (40 s) | 72°C (60 s) | 72°C (7 min) |
| Microsporidia | 94°C (10 min) | 35 | 94°C (30 s) | 62°C (30 s) | 72°C (30 s) | 72°C (10 min) |
3.3.3. Sensitivity and Specificity Assessment
The sensitivity and specificity of the PCR-based diagnostic method were separately calculated and compared with the standard gold method of each parasite.
4. Results
In this study, we examined 64 patients with immunodeficiency accompanied by COPD. Table 3 presents the results of the examination of BAL specimens with direct and PCR methods to identify Toxoplasma, Cryptosporidium, and Microsporidia parasites. Noteworthy, Microsporidia was not identified in the samples using these two diagnostic methods.
Frequency of Three Parasitic Protozoa in Patients with Immunodeficiency Accompanied by COPD Based on Direct and PCR Methods
| Direct Microscopic Diagnosis | PCR | |||
|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |
| Toxoplasma | 3 | 61 | 2 | 62 |
| Cryptosporidium | 9 | 55 | 2 | 62 |
| Microsporidia | 0 | 64 | 0 | 64 |
The sensitivity and specificity of the PCR-based method compared to the gold standard method for Toxoplasma and Cryptosporidium are summarized in Table 4. As observed, the sensitivity and specificity of the PCR-based method were 66.7% and 100% for Toxoplasma and 11.1% and 98.2% for Cryptosporidium.
Sensitivity and Specificity of the PCR Method Compared to the Gold Standard (Direct Method) for Toxoplasma and Cryptosporidium in BAL Samples of Immunocompromised Patients
| Direct Method (Gold Standard) | |||
|---|---|---|---|
| Positive | Negative | Total | |
| PCR (Toxoplasma) | |||
| Positive | 2 | 0 | 2 |
| Negative | 1 | 61 | 62 |
| Total | 3 | 61 | 64 |
| PCR (Cryptosporidium) | |||
| Positive | 1 | 1 | 2 |
| Negative | 8 | 54 | 62 |
| Total | 9 | 55 | 64 |
5. Discussion
The increase in the identification of various immune system disorders worldwide has revealed the incidence of more disseminated parasitic infections, such as pulmonary infections (24-26). These infections require special attention because significantly more immunocompromised cases have been reported in recent years (1). Misdiagnosis of these infections can lead to treatment failure and death (1). In this regard, the standardization of differential diagnostic methods seems to be the first step for identifying the types of parasites that cause respiratory infections. Today, there are facilities for direct microscopic examination (staining), and there exist culture and PCR-based methods for identifying different types of parasites (27). These methods are routinely used for the laboratory detection of COPD causative agents in the samples of pulmonary secretions (28). The efficiency of a diagnostic method may change based on the type of specimen; therefore, it is necessary to design and conduct studies to evaluate the effectiveness of various techniques for different types of specimens, like the current study.
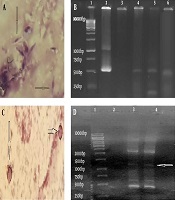
In the present study, all BAL samples were examined by two methods to compare the sensitivity and specificity of each method for identifying different kinds of protozoa. Our observations showed that the sensitivity of PCR for identifying Toxoplasma and Cryptosporidium was 66.7% and 11.1%, respectively (Figure 1). Furthermore, Microsporidia was not detected in BAL samples by PCR and direct microscopic methods. In a study, Lavrard et al. (13) analyzed BAL samples from HIV patients for Toxoplasma infection. The researcher did not report any difference in the efficiency of direct microscopic and PCR methods in identifying this parasite, which is contrary to the present study, where the direct method was more sensitive.
Due to the similarity of the specimens and the diagnostic method in both studies, it seems that a human error led to the difference in the results. In another study, Morgan et al. assessed the potential of PCR and direct microscopic method (acid-fast staining) to identify Cryptosporidium in fecal samples. In contrast to our study, they showed that compared with routine microscopic methods, the PCR method was more efficient in identifying Cryptosporidium in this type of specimen (29). However, in a review study of respiratory cryptosporidiosis, Sponseller et al. (30) reached a conclusion similar to ours. More specifically, they reported that the direct microscopic methods (acid-fast and Giemsa) were more efficient than PCR in identifying Cryptosporidium in BAL samples. It seems that the difference between the samples (stool and BAL) led to the difference between the results of the present study and Morgan et al.’s study (29).
Identification of Toxoplasma and Cryptosporidium. A, Toxoplasma tachyzoites in the BAL sample by staining method (Giemsa staining, 100×); B, Toxoplasma identification by PCR method [Lane 1, marker (thermo-scientific SM0313); Lane 2, positive control; Lane 3, negative control; Lanes 4-6, positive samples with specific fragment for Toxoplasma (~529 bp)]; C, Cryptosporidium oocysts in the BAL sample by staining method (Ziehl Neelsen staining, x100); D: Cryptosporidium identification by PCR method [Lane 1, marker (thermo-scientific SM0313); Lane 2, negative control; Lane 3, positive control; Lane 4, positive sample with specific fragment for Cryptosporidium (~1325 bp)]
![Identification of Toxoplasma and Cryptosporidium. A, Toxoplasma tachyzoites in the BAL sample by staining method (Giemsa staining, 100×); B, Toxoplasma identification by PCR method [Lane 1, marker (thermo-scientific SM0313); Lane 2, positive control; Lane 3, negative control; Lanes 4-6, positive samples with specific fragment for Toxoplasma (~529 bp)]; C, Cryptosporidium oocysts in the BAL sample by staining method (Ziehl Neelsen staining, x100); D: Cryptosporidium identification by PCR method [Lane 1, marker (thermo-scientific SM0313); Lane 2, negative control; Lane 3, positive control; Lane 4, positive sample with specific fragment for Cryptosporidium (~1325 bp)] Identification of Toxoplasma and Cryptosporidium. A, Toxoplasma tachyzoites in the BAL sample by staining method (Giemsa staining, 100×); B, Toxoplasma identification by PCR method [Lane 1, marker (thermo-scientific SM0313); Lane 2, positive control; Lane 3, negative control; Lanes 4-6, positive samples with specific fragment for Toxoplasma (~529 bp)]; C, Cryptosporidium oocysts in the BAL sample by staining method (Ziehl Neelsen staining, x100); D: Cryptosporidium identification by PCR method [Lane 1, marker (thermo-scientific SM0313); Lane 2, negative control; Lane 3, positive control; Lane 4, positive sample with specific fragment for Cryptosporidium (~1325 bp)]](https://services.brieflands.com/cdn/serve/31578/09440e0907fe1032fe319cecd0854df2c0709511/jjm-13-12-111038-i001-preview.png)
Recent studies have confirmed that PCR is an accurate method for identifying and determining Cryptosporidium species. Nonetheless, when the number of parasites is low, they cannot be detected by PCR. Primers also play a role in the sensitivity and specificity of the test. The newly designed primers seem to be effective in detecting a small number of Cryptosporidium parasites in fecal specimens (31). However, for more accurate conclusions, these primers should be tested on other samples, as well.
Saigal et al. (9) and Mena et al. (32) evaluated the direct microscopic and nested PCR methods in the detection of intestinal microsporidiosis. In their study, the sensitivity and specificity of the molecular method were reported to be higher than those of the staining methods. In both studies, two staining methods were compared to detect Microsporidia. Based on the results, the modified trichrome staining had more sensitivity and specificity compared to the calcofluor staining method. Ozkoc et al. (3) and Tabatabaie et al. (33) conducted a similar study on BAL samples and obtained similar results to the previous study. In our study, Microsporidia was not detected in any specimen. In Iran, the prevalence of Microsporidia in immunocompromised patients was 8.18% (34). Given that the gastrointestinal and pulmonary cases of Microsporidia are most often reported in immunocompromised individuals, it is possible that the result of our study was false-negative. Differences in the type of specimens, incorrect choice of staining method, and factors such as DNA extraction and examiner experience (in identifying Microsporidia) can be effective in obtaining such results.
5.1. Conclusions
Determining a standard diagnostic method for parasites depends on factors, such as the type of specimen and the type of parasite. Based on the results of the present study, the direct microscopic method is the best diagnostic method for Toxoplasma and Cryptosporidium in BAL samples. There was only a slight difference between the results of direct microscopic examination and PCR in the diagnosis of Toxoplasma; therefore, to achieve more accurate results, it is suggested that such studies be repeated with larger sample sizes and different specimen types.
Acknowledgements
References
-
1.
Martinez-Giron R, Esteban JG, Ribas A, Doganci L. Protozoa in respiratory pathology: A review. Eur Respir J. 2008;32(5):1354-70. [PubMed ID: 18978136]. https://doi.org/10.1183/09031936.00022008.
-
2.
Cheepsattayakorn A, Cheepsattayakorn R. Parasitic pneumonia and lung involvement. Biomed Res Int. 2014;2014:874021. [PubMed ID: 24995332]. [PubMed Central ID: PMC4068046]. https://doi.org/10.1155/2014/874021.
-
3.
Ozkoc S, Bayram Delibas S, Akisu C. Evaluation of pulmonary microsporidiosis in iatrogenically immunosuppressed patients. Tuberk Toraks. 2016;64(1):9-16. [PubMed ID: 27266280]. https://doi.org/10.5578/tt.10207.
-
4.
Petersen E, Edvinsson B, Lundgren B, Benfield T, Evengard B. Diagnosis of pulmonary infection with Toxoplasma gondii in immunocompromised HIV-positive patients by real-time PCR. Eur J Clin Microbiol Infect Dis. 2006;25(6):401-4. [PubMed ID: 16767490]. https://doi.org/10.1007/s10096-006-0156-5.
-
5.
Poirot JL, Deluol AM, Antoine M, Heyer F, Cadranel J, Meynard JL, et al. Broncho-pulmonary cryptosporidiosis in four HIV-infected patients. J Eukaryot Microbiol. 1996;43(5):78S-9S. [PubMed ID: 8822872]. https://doi.org/10.1111/j.1550-7408.1996.tb05007.x.
-
6.
Niyyati M, Lorenzo-Morales J, Mohebali M, Rezaie S, Rahimi F, Babaei Z, et al. Comparison of a PCR-based method with culture and direct examination for diagnosis of Acanthamoeba keratitis. Iran J Parasitol. 2009:38-43.
-
7.
Perez-Santonja JJ, Kilvington S, Hughes R, Tufail A, Matheson M, Dart JK. Persistently culture positive acanthamoeba keratitis: In vivo resistance and in vitro sensitivity. Ophthalmology. 2003;110(8):1593-600. [PubMed ID: 12917179]. https://doi.org/10.1016/S0161-6420(03)00481-0.
-
8.
Boggild AK, Martin DS, Lee TY, Yu B, Low DE. Laboratory diagnosis of amoebic keratitis: Comparison of four diagnostic methods for different types of clinical specimens. J Clin Microbiol. 2009;47(5):1314-8. [PubMed ID: 19321727]. [PubMed Central ID: PMC2681827]. https://doi.org/10.1128/JCM.00173-09.
-
9.
Saigal K, Khurana S, Sharma A, Sehgal R, Malla N. Comparison of staining techniques and multiplex nested PCR for diagnosis of intestinal microsporidiosis. Diagn Microbiol Infect Dis. 2013;77(3):248-9. [PubMed ID: 23993212]. https://doi.org/10.1016/j.diagmicrobio.2013.07.004.
-
10.
Khanaliha K, Mirjalali H, Mohebali M, Tarighi F, Rezaeian M. Comparison of three staining methods for the detection of intestinal Microspora spp. Iran J Parasitol. 2014;9(4):445-51. [PubMed ID: 25759724]. [PubMed Central ID: PMC4345082].
-
11.
Mercado R, Buck GA, Manque PA, Ozaki LS. Cryptosporidium hominis infection of the human respiratory tract. Emerg Infect Dis. 2007;13(3):462-4. [PubMed ID: 17552101]. [PubMed Central ID: PMC2725888]. https://doi.org/10.3201/eid1303.060394.
-
12.
Bourdin C, Busse A, Kouamou E, Touafek F, Bodaghi B, Le Hoang P, et al. PCR-based detection of Toxoplasma gondii DNA in blood and ocular samples for diagnosis of ocular toxoplasmosis. J Clin Microbiol. 2014;52(11):3987-91. [PubMed ID: 25210066]. [PubMed Central ID: PMC4313235]. https://doi.org/10.1128/JCM.01793-14.
-
13.
Lavrard I, Chouaid C, Roux P, Poirot JL, Marteau M, Lemarchand B, et al. Pulmonary toxoplasmosis in HIV-infected patients: Usefulness of polymerase chain reaction and cell culture. Eur Respir J. 1995;8(5):697-700. [PubMed ID: 7544741].
-
14.
Peretz A, Geffen Y, Socea SD, Pastukh N, Graffi S. Comparison of fluorescence microscopy and different growth media culture methods for Acanthamoeba keratitis diagnosis. Am J Trop Med Hyg. 2015;93(2):316-8. [PubMed ID: 25962772]. [PubMed Central ID: PMC4530754]. https://doi.org/10.4269/ajtmh.15-0193.
-
15.
Collins AM, Rylance J, Wootton DG, Wright AD, Wright AK, Fullerton DG, et al. Bronchoalveolar lavage (BAL) for research; obtaining adequate sample yield. J Vis Exp. 2014;(85). [PubMed ID: 24686157]. [PubMed Central ID: PMC4157694]. https://doi.org/10.3791/4345.
-
16.
Singletary ML, Phillippi-Falkenstein KM, Scanlon E, Bohm RJ, Veazey RS, Gill AF. Modification of a common BAL technique to enhance sample diagnostic value. J Am Assoc Lab Anim Sci. 2008;47(5):47-51. [PubMed ID: 18947171]. [PubMed Central ID: PMC2691541].
-
17.
Joseph J, Murthy S, Garg P, Sharma S. Use of different stains for microscopic evaluation of corneal scrapings for diagnosis of Microsporidial keratitis. J Clin Microbiol. 2006;44(2):583-5. [PubMed ID: 16455916]. [PubMed Central ID: PMC1392708]. https://doi.org/10.1128/JCM.44.2.583-585.2006.
-
18.
Barcan LA, Dallurzo ML, Clara LO, Valledor A, Macias S, Zorkin E, et al. Toxoplasma gondii pneumonia in liver transplantation: Survival after a severe case of reactivation. Transpl Infect Dis. 2002;4(2):93-6. [PubMed ID: 12220246]. https://doi.org/10.1034/j.1399-3062.2002.t01-1-00006.x.
-
19.
Solymane H, Eslamirad Z, Bayat M, Hajihossein R. Molecular detection of Toxoplasma gondii oocytes in the soil from the public parks of the Arak City, Iran. Res Mol Med. 2014;2(1):35-8. https://doi.org/10.18869/acadpub.rmm.2.1.35.
-
20.
Homan WL, Vercammen M, De Braekeleer J, Verschueren H. Identification of a 200- to 300-fold repetitive 529 bp DNA fragment in Toxoplasma gondii, and its use for diagnostic and quantitative PCR. Int J Parasitol. 2000;30(1):69-75. [PubMed ID: 10675747]. https://doi.org/10.1016/s0020-7519(99)00170-8.
-
21.
Xiao L, Escalante L, Yang C, Sulaiman I, Escalante AA, Montali RJ, et al. Phylogenetic analysis of Cryptosporidium parasites based on the small-subunit rRNA gene locus. Appl Environ Microbiol. 1999;65(4):1578-83. [PubMed ID: 10103253]. [PubMed Central ID: PMC91223]. https://doi.org/10.1128/AEM.65.4.1578-1583.1999.
-
22.
Yu JR, Lee SU, Park WY. Comparative sensitivity of PCR primer sets for detection of Cryptosporidium parvum. Korean J Parasitol. 2009;47(3):293-7. [PubMed ID: 19724705]. [PubMed Central ID: PMC2735697]. https://doi.org/10.3347/kjp.2009.47.3.293.
-
23.
Ghorbanzadeh B, Sadraie J, Emadi Kuchak H. Diagnosis of Cryptosporidium and intestinal Microsporidia in HIV/AIDS patients with staining and PCR methods on 16srRNA gen. J Arak Univ Med Sci. 2012;15(7):37-47.
-
24.
Pilania RK, Chaudhary H, Jindal AK, Rawat A, Singh S. Current status and prospects of primary immunodeficiency diseases in Asia. Genes Dis. 2020;7(1):3-11. [PubMed ID: 32181271]. [PubMed Central ID: PMC7063407]. https://doi.org/10.1016/j.gendis.2019.09.004.
-
25.
Modell V, Orange JS, Quinn J, Modell F. Global report on primary immunodeficiencies: 2018 update from the Jeffrey Modell Centers Network on disease classification, regional trends, treatment modalities, and physician reported outcomes. Immunol Res. 2018;66(3):367-80. [PubMed ID: 29744770]. https://doi.org/10.1007/s12026-018-8996-5.
-
26.
Ferreira MS. Infections by protozoa in immunocompromised hosts. Mem Inst Oswaldo Cruz. 2000;95 Suppl 1:159-62. [PubMed ID: 11142706]. https://doi.org/10.1590/s0074-02762000000700026.
-
27.
Ndao M. Diagnosis of parasitic diseases: Old and new approaches. Interdiscip Perspect Infect Dis. 2009;2009:278246. [PubMed ID: 20069111]. [PubMed Central ID: PMC2804041]. https://doi.org/10.1155/2009/278246.
-
28.
Wessels E, Schelfaut JJ, Bernards AT, Claas EC. Evaluation of several biochemical and molecular techniques for identification of Streptococcus pneumoniae and Streptococcus pseudopneumoniae and their detection in respiratory samples. J Clin Microbiol. 2012;50(4):1171-7. [PubMed ID: 22278834]. [PubMed Central ID: PMC3318541]. https://doi.org/10.1128/JCM.06609-11.
-
29.
Morgan UM, Pallant L, Dwyer BW, Forbes DA, Rich G, Thompson RC. Comparison of PCR and microscopy for detection of Cryptosporidium parvum in human fecal specimens: Clinical trial. J Clin Microbiol. 1998;36(4):995-8. [PubMed ID: 9542924]. [PubMed Central ID: PMC104676]. https://doi.org/10.1128/JCM.36.4.995-998.1998.
-
30.
Sponseller JK, Griffiths JK, Tzipori S. The evolution of respiratory Cryptosporidiosis: evidence for transmission by inhalation. Clin Microbiol Rev. 2014;27(3):575-86. [PubMed ID: 24982322]. [PubMed Central ID: PMC4135895]. https://doi.org/10.1128/CMR.00115-13.
-
31.
Bairami Kuzehkanan A, Rezaeian M, Zeraati H, Mohebali M, Meamar AR, Babaei Z, et al. A sensitive and specific PCR based method for identification of Cryptosporidium Sp. Using new primers from 18S ribosomal RNA. Iran J Parasitol. 2011;6(4):1-7. [PubMed ID: 22347307]. [PubMed Central ID: PMC3279906].
-
32.
Mena CJ, Barnes A, Castro G, Guasconi L, Burstein VL, Beccacece I, et al. Microscopic and PCR-based detection of microsporidia spores in human stool samples. Rev Argent Microbiol. 2020. [PubMed ID: 32595002]. https://doi.org/10.1016/j.ram.2020.04.005.
-
33.
Tabatabaie F, Abrehdari Tafreshi Z, Shahmohammad N, Pirestani M. Molecular detection of microsporidiosis in various samples of Iranian immunocompromised patients. J Parasit Dis. 2015;39(4):634-8. [PubMed ID: 26688625]. [PubMed Central ID: PMC4675584]. https://doi.org/10.1007/s12639-014-0432-8.
-
34.
Ghoyounchi R, Ahmadpour E, Spotin A, Mahami-Oskouei M, Rezamand A, Aminisani N, et al. Microsporidiosis in Iran: A systematic review and meta-analysis. Asian Pac J Trop Med. 2017;10(4):341-50. [PubMed ID: 28552104]. https://doi.org/10.1016/j.apjtm.2017.03.017.