Abstract
Background:
Studies on education with peer support for improving diabetes care among diabetes patients are relatively rare in developing countries, including Bangladesh.Objectives:
The purpose of the present study was to compare the effectiveness of diabetes education by health professionals versus peers for achieving targeted diabetes care among people with type 2 diabetes.Methods:
With a quasi-experimental design, 133 type 2 diabetes patients [hemoglobin A1c (HbA1c) > 8%] were screened conveniently from the Outpatient Department of BIRDEM (the Tertiary Hospital of Diabetic Association of Bangladesh). Sixty-seven participants were guided by four professionals and 66 by eight peer educators. Following a predesigned curriculum, four professionals and eight peers provided two-hour diabetes education, once to the participants at the time of their enrollment. The changes observed in fasting blood glucose (FBG), HbA1c, weight, systolic blood pressure (SBP), diastolic blood pressure (DBP), knowledge, and lifestyles were compared after 12 weeks of the intervention and psychological support among 124 (59 for professionals and 65 for peers) participants. The mean age was (53.4 ± 10.4) years.Results:
In the peer-educated group, after the intervention, levels of FBG (3.9 ± 3.1 versus 6.7 ± 0.7), HbA1c (8.04 ± 1.1 versus 9.1 ± 1.5), and DBP (81.86 ± 13.1 versus 87.29 ± 8.2) decreased significantly (P < 0.05) compared to the health professional-educated group. After receiving education, levels of HbA1c, FBG, and SBP decreased significantly (P < 0.05) in both groups. The mean knowledge improved significantly (P = 0.0001) among the peer-guided participants. Approximately 6%, 65%, and 25% had good, average, and poor (GAP) knowledge about diabetes respectively before the intervention, whereas 15%, 63%, and 20% had GAP knowledge after the intervention.Conclusions:
The findings suggest that it is feasible to train peer educators with the necessary knowledge and skills to facilitate diabetes self-management.Keywords
Type 2 Diabetes Peer Support Diabetes Self-Management Education Health Education Bangladesh
1. Background
The prevalence of type 2 diabetes among adults in the South-East Asia region was estimated as 8.5% in 2015 and it is expected to rise to 10.7% by 2040 (1). Until a decade ago, diabetes was not considered a major public-health problem in developing countries, including Bangladesh. The situation has now changed dramatically. Treatment of type 2 diabetes with modern drugs may improve diabetes care, however, this therapy is far from preventing micro- or macro-vascular complications effectively. This suggests that there is a strong need to intensify lifestyle interventions and motivate patients to better manage diabetes by themselves.
People with type 2 diabetes do not need to initiate a complex regimen of self-care behaviors, yet, more importantly, they need to sustain these efforts over one’s lifetime because of its chronic nature. Diabetes self-management education (DSME) programs help improve diabetes-related health outcomes in the short-term, yet without continued follow-up and proper support, these achievements cannot be maintained in the long run (2, 3).
Perhaps, a successful therapeutic goal depends on sustainable effective self-management behaviors and ‘emotional coping’ with diabetes. This sustainable goal has many barriers, such as deficiency of satisfactory understanding of diabetes and modification of management, lack of self-assurance or skills to succeed against the disease, lack of effective support from families and friends for management, increasing burden of diabetes, lack of enough time allotted to clinics, rising cost of healthcare, and inability to access appropriate healthcare, particularly in the underserved and low-resource community (4).
For professional health workers, it is often impossible or too costly to provide this support on a one-on-one basis. Thus, to empower patients, development and evaluation of low-cost strategies within available resources is essential (5). Healthcare scientists have been trying to adopt different modalities of social support programs, such as peer support, community health workers or advisors, peer coach or mentors, face-to-face discussions or telephone or web, and email-based care to maintain sustainable improvement in health gains for persons with diabetes. The World Health Organization defined “peer support” as an economic, flexible intervention for improving diabetes care, and outcomes (6).
In simple words, people with diabetes could be chosen to educate other patients regarding diabetes, known as peer support. One research claimed that the role of a peer educator includes assistance of day-to-day disease management, providing emotional and social support, linkages to clinical care, and a hands-on, and flexible attitude towards fellow patients (7).
Peer-led diabetes self-management program was used in this pilot study for determining the feasibility of this program among Bangladeshi people with type 2 diabetes. This program may be one of the steps to improve and reduce the burden of diabetes and would be a promising addition to public health systems.
2. Objectives
The aim of the study was to evaluate the effectiveness of a diabetes education program guided by health professionals versus peers in improving diabetes care among people with type 2 diabetes.
3. Methods
3.1. Study Design
A quasi-experimental design (intervention without randomization) was used.
3.2. Patients
In total, 133 type 2 diabetes patients (HbA1c > 8% and residing in Dhaka city) were screened conveniently from the Outpatient Department (OPD) of BIRDEM (the Tertiary Hospital of Diabetic Association of Bangladesh). The enrollment and interviews were carried out during October to November 2010. The intervention was implemented from December 2010 to February 2011. Patients with other medical complications or those, who were unable to answer a short list of simple questions (sociodemographic information, such as name, address, disease complications, etc.) were excluded from the study.
3.3. Selection of Trainers
The diabetes education trainer program team of BIRDEM was invited to send four trainers for conducting a three-day training program for professionals and peers. They were requested to evaluate the performance of health professionals and peer educators. The trainers conducted pre- and post-training assessments of the professionals and peers. The trainers were briefed about the background and objectives of the workshop. They reviewed the existing curriculum of the health educator training program, keeping in mind the Funnell’s education scheme (8).
3.4. Selection of Health Professional
Four of ten female medical graduates, practicing in the city of Dhaka, with more than four years of experience in diabetes-management education, were selected as professionals and they were provided diabetes education in the local language.
3.5. Selection of Peer Educators
Peer educators were also trained following the same curriculum and the same delivery method was followed in case of health professionals. Twenty-six diabetes patients attended the program and eight peer educators (four males and four females), who had diabetes at least for five years were selected (age > 40 years, HbA1c < 7%, graduation in education, committed to training and willing to spend sufficient time, enthusiastic to be peer educators, and residing in Dhaka city).
3.6. Intervention Program
Sixty-seven patients led by the health professionals were divided to four groups, and each group was directed by a professional. Sixty-six patients guided by peer educators were also divided to four groups, and each group was led by two peer educators.
All the patients (both professionals and peer educator groups) attended a two-hour diabetes education program once at the time of their enrollment, following a predesigned curriculum (8). The first interview of the patients was taken before attending the education session.
The education program was followed by face-to-face and group discussions (using leaflets, a flip-chart, and posters) for any problems they faced, thereby allowing them to freely discuss general management of diabetes.
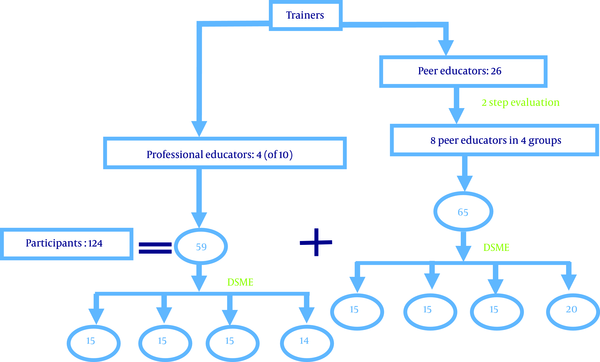
After 12 weeks, changes in knowledge, self-care activities, glycemic status, weight, and blood pressure among 124 (93%) patients (59 patients for professionals and 65 for peers) were observed following the information derived from the same questionnaire (Figure 1). The remaining nine (7%) participants were dropped out of the program due to their unwillingness and had non-availability of sufficient time to follow the program.
Design of the training program and diabetes self-management education
3.7. Development of Questionnaire and Statistical Analysis
The knowledge and self-care activities of the patients were assessed using an interviewer-administered questionnaire, and the interview was administered in the OPD setting. A medium-size three-part questionnaire was designed by the researcher. Sociodemographic information, family history of diabetes, duration of diabetes, reported data on blood pressure, weight, and glycemic status, treatment regimen, and complications were covered in the first part of the questionnaire. The second part covered 12 knowledge questions, and the third part focused on steps taken to monitor glucose, following the advice of the professionals and peers, performing regular exercise, and taking other actions indicative of patient lifestyle.
Knowledge questions were developed following the local guidelines of the Diabetic Association of Bangladesh (9). The knowledge-assessment questionnaire included questions related to diabetes, blood testing, hyperglycemia, and general principles of disease care. The questionnaire was finalized based on the results of a pretest.
During analysis, each correct response was assigned a score of 1, and each incorrect response was assigned a score of 0. Thus, for 12 items for basic knowledge, the maximum attainable score was 12, and the minimum score was 0. Similarly, for seven self-care activities, items, such as glucose monitoring, exercise, cutting of nails, smoking, and consumption of betel nuts, the maximum attainable score was 7 and the minimum was 0. The level of knowledge and self-care activities was classified according to each respondent’s score. Poor knowledge and self-care activities corresponded to a score of < mean - 1 SD; average knowledge and self-care activities corresponded to a score between mean ± 1 SD; good knowledge and self-care activities corresponded to a score of > mean + 1 SD (10). Statistical tests were considered significant at P value of ≤ 5% (≤ 0.05). Frequencies were calculated for descriptive analysis. Differences between the baseline and the follow-up data were calculated using Paired t-test and Unpaired t-test for group differences.
4. Results
The mean age of the people with type 2 diabetes in peer educators and professionals was 54.1 ± 9.4 and 52.9 ± 11.4 years, respectively. The duration of diabetes was above three years in both groups. Thirty-four percent of the people with type 2 diabetes were homemakers in the peer group and 25% in professionals (Table 1).
| Variable | Peer Educators (N = 65) | Professionals (N = 59) |
|---|---|---|
| Age, y | 54.1 ± 9.4 | 52.9 ± 11.4 |
| ≤ 40 | 7 (11) | 8 (14) |
| 41 - 60 | 43 (66) | 36 (61) |
| 61 - 80 | 15 (23) | 15 (25) |
| Gender ratio, M:F | 47:18 | 33:26 |
| Duration of diabetes, y | 3.45 ± 1.2 | 3.49 ± 1.1 |
| Occupation | ||
| Service | 19 (29) | 13 (22) |
| Business | 12 (19) | 22 (37) |
| Homemaker | 22 (34) | 15 (25) |
| Other | 12 (18) | 9 (15) |
Table 2 shows the comparison of the different parameters between health professionals versus peer educators at baseline and follow-up among people with type 2 diabetes. Fasting blood glucose (FBG) [mmol/L, 3.9 ± 3.1 versus 6.7 ± 0.7, P = 0.0001] and their HbA1c (%, 8.04 ± 1.1 versus 9.1 ± 1.5, P = 0.0001) level significantly improved after receiving education by the peer educators compared with the health professionals. At baseline, no significant change was observed between the two groups. Weight, body mass index, systolic blood pressure (SBP), and diastolic blood pressure (DBP) did not show any significant difference between professionals and peer educators at baseline. Only the level of DBP was significantly reduced in the professionals group (mmHg 81.86 ± 13.1 versus 87.29 ± 8.2, P = 0.008) compared to that of peer educators at the follow-up visit.
Comparison of the Glycemic Status, Body Mass Index and Blood Pressure Among Patients Between Health Professionals Versus Peer Educators at Baseline and Follow-Upa,b
| Baseline | Follow-Up | |||||
|---|---|---|---|---|---|---|
| Processionals (N = 67) | Peer Educators (N = 66) | P Value | Processionals (N = 59) | Peer Educators (N = 65) | P Value | |
| FBG, mmol/L | 7.9 ± 3.2 | 7.07 ± 1.9 | 0.2 | 6.7 ± 0.7 | 3.9 ± 3.1 | 0.0001 |
| HbA1c, % | 9.5 ± 1.7 | 9.5 ± 2.1 | 0.9 | 9.1 ± 1.5 | 8.04 ± 1.1 | 0.0001 |
| Weight, kg | 69.24 ± 10.3 | 68.71 ± 11.1 | 0.8 | 67.75 ± 16.8 | 67.55 ± 10.2 | 0.9 |
| BMI, kg/m2 | 24.76 ± 5.9 | 25.29 ± 3.05 | 0.6 | 22.80 ± 9.3 | 25.09 ± 2.8 | 0.3 |
| SBP, mmHg | 134.69 ± 16.7 | 140.77 ± 17.5 | 0.07 | 129.12 ± 12.6 | 132.63 ± 11.7 | 0.11 |
| DBP, mmHg | 82.65 ± 10.6 | 85.19 ± 9.2 | 0.2 | 87.29 ± 8.2 | 81.86 ± 13.1 | 0.008 |
Results of the Paired t-test are presented in Table 3. After the intervention, the levels of HbA1c (%, 8.04 ± 1.1 versus 9.5 ± 2.1, P = 0.0001), FBG (mmol/L, 3.9 ± 3.1 versus 7.07 ± 1.9, P = 0.0001), and SBP (mmgH, 132.6 ± 11.1 versus 140.7 ± 17.5, P = 0.002) significantly changed in people with type 2 diabetes educated by peers compared to the baseline. However, no significant changes were observed in DBP and BMI. After the intervention, the levels of HbA1c (%, 9.1 ± 1.5 versus 9.51 ± 1.7, P = 0.001), FBG (mmol/L, 6.7 ± 0.7 versus 7.9 ± 3.2, P = 0.04), and SBP (mmHg, 129.4 ± 12.6 versus 134.6 ± 16.7, P = 0.05) also significantly changed in people with type 2 diabetes educated by professionals compared to the baseline.
Changes of the Variable Among Patients at Follow-Up Educated by Peer Educators and Health Professionalsa,b
| Variable | Peer Educators (N = 65) | Health Professionals (N = 59) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | P Value | Baseline | Follow-Up | P Value | |
| HbA1c, % | 9.5 ± 2.1 | 8.04 ± 1.1 | 0.0001 | 9.51 ± 1.7 | 9.1 ± 1.5 | 0.001 |
| FBG, mmol/L | 7.07 ± 1.9 | 3.9 ± 3.1 | 0.0001 | 7.9 ± 3.2 | 6.7 ± 0.7 | 0.04 |
| SBP, mmHg | 140.7 ± 17.5 | 132.6 ± 11.1 | 0.002 | 134.6 ± 16.7 | 129.4 ± 12.6 | 0.05 |
| DBP, mmHg | 85.1 ± 9.2 | 88.0 ± 8.2 | 0.07 | 82.6 ± 10.6 | 81.8 ± 13.1 | 0.65 |
| BMI, kg/m2 | 25.2 ± 3.05 | 25.1 ± 2.8 | 0.43 | 24.7 ± 5.9 | 23.8 ± 8.04 | 0.53 |
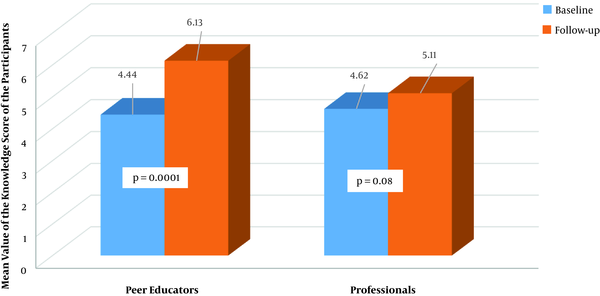
The knowledge on DM improved in the people with type 2 diabetes educated by the peer (4.44 versus 6.13) and professionals (4.62 versus 5.11) though more significant improvement was found in the peer group (P = 0.0001) (Figure 2).
Changes in level of knowledge in study subjects educated by peer educators and health professionals
The knowledge distribution of the people with type 2 diabetes regarding diabetes and the improvement of their lifestyle are shown in Table 4. Their mean knowledge scores were 5 ± 2 at baseline and 6 ± 2 after the intervention. Approximately 65% of the people with type 2 diabetes had an average (3 - 7) knowledge score at baseline whereas 63% had an average (4 - 8) knowledge score at follow-up. About 25% had poor (< 3) knowledge at baseline, and 20% had poor (< 4) knowledge after the intervention. About 6% had good (> 7) knowledge at baseline whereas 15% had good (> 8) knowledge after receiving education. The mean lifestyle score of the people with type 2 diabetes was 3 ± 2 at baseline and 4 ± 1 after the intervention. At baseline, 54% had an average (1 - 5) lifestyle score. The slightly increase in the percentage (58%) found an average (3 - 5) lifestyle score after the intervention. About 30% had a poor (< 1) lifestyle score at baseline, and 29% had a poor (< 3) lifestyle score at the follow-up visit. About 14% had a good (> 5) lifestyle score at baseline, and after receiving education, 10% had a good (> 5) lifestyle score.
| Variables | Baseline | Follow-up | ||||
|---|---|---|---|---|---|---|
| Good | Average | Poor | Good | Average | Poor | |
| Levels of knowledge | 7 (6) | 81 (65) | 31 (25) | 18 (15) | 78 (63) | 25 (20) |
| Changes in lifestyle | 17 (14) | 67 (54) | 37 (30) | 12 (10) | 72 (58) | 36 (29) |
5. Discussion
To the best of the author’s knowledge, no study has been conducted to understand the feasibility, acceptance, and benefits of peer-led diabetes self-management program in low-middle income countries (LMIC), such as Bangladesh. The patients supported by the peer educator groups experienced significantly (P = 0.0001) improved FBG and HbA1c levels compared to the patients educated by the professionals. Seventeen percent of the patients from the peer groups achieved the targeted HbA1c level (< 7%) after 12 weeks of the intervention whereas the percentage was 7% in the professional groups.
The results of the assessment between baseline and follow-up visits in both groups showed a significant (P < 0.05) reduction in FBG, HbA1c, and SBP. The professional education intervention in this study achieved only marginal improvement in HbA1c and FBG, although the changes in the same parameters were good and highly significant in patients of the peer educators. Studies have indicated that peer-led education is effective in helping patients with uncontrolled blood glucose than standard care (11, 12).
A significant (P < 0.05) improvement in the knowledge level proves that peers, who share knowledge and experiences with others living with diabetes, is an important factor to improve and sustain behavior change and health condition. Similar opinion was aired in other studies by Davidson et al. (13), Eysenbach et al. (14), and Parry and Watt-Watson (15).
In particular, peer support can make a relationship people with a chronic disease or condition and can share their understanding regarding disease with others, yet many health professionals do not have that type of practical and emotional support for the managing the diseases.
In this pilot study, peer-led educational interventions led to improvements in clinical outcomes and knowledge level. Similar findings (16) were found in Africa yet in contrast, a cluster-randomized trial on a group education intervention led by health professionals in South Africa (17) reported negative results, including poor attendance at sessions and low adherence to self-care activities.
Changes in lifestyle among people with type 2 diabetes of the present study were not remarkable, yet gradually improved. The reasons behind this may be the short duration of the intervention, less devotion to self-care activities, and absence from the education session. A one-year follow-up would have indicated whether the interventions had a more lasting impact (18), though due to lack of fund, it was not possible to run a one-year intervention in the present study.
The study patients with type 2 diabetes educated by the peer educators achieved better outcomes. However, peer-led DSME interventions may respond to the needs of people living with diabetes. So far, there is no evidence in the literature proving its effectiveness in Bangladesh.
In a resource-constrain community, like Bangladesh, a peer-led program can sustain diabetes-related goals, coping with their life through reinforcement of empowerment to circumvent barriers. Peer-support interventions will be appreciated by professionals and policy-makers seeking help and may be used for supplementing treatment to patients motivated to improve their behaviors related to diabetes.
The study had some limitations. As this was a pilot study, it was not possible to select a large number of samples and to provide a one-year intervention. Besides, the study was confined only to a community with the same economic status, therefore, the study was not a randomized control trial. Due to lack of fund and for the nature of the study, the duration of intervention was short, i.e. three months. Finally, the individual mode of strategies/delivery of teaching peer participants was not analyzed separately to assess effectiveness and affectivity.
5.1. Conclusions
Peer-led education is an effective mode of DSME to improve the health status of individuals with diabetes, who failed to achieve the goals. It may be considered an adjunct and supplement to clinic-based or center-based education facilities. More studies are required to define the effect of the peer-support model in larger populations, long-term outcomes, and its sustainability. This pilot study will help make plans to perform studies in different settings to explore the feasibility of peer- support models in diabetes care.
Acknowledgements
References
-
1.
Aldworth J, Patterson C, Jacobs E, Misra A, Tamayo T, Elizabeth BS. IDF diabetes atlas. Abu Dhabi, United Arab Emirates: International Diabetes Federation (IDF); 2017.
-
2.
Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;(2). CD003417. [PubMed ID: 15846663]. https://doi.org/10.1002/14651858.CD003417.pub2.
-
3.
Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159-71. [PubMed ID: 12087014]. https://doi.org/10.2337/diacare.25.7.1159.
-
4.
Collins MM, Bradley CP, O'Sullivan T, Perry IJ. Self-care coping strategies in people with diabetes: A qualitative exploratory study. BMC Endocr Disord. 2009;9:6. [PubMed ID: 19232113]. [PubMed Central ID: PMC2664817]. https://doi.org/10.1186/1472-6823-9-6.
-
5.
World Health Organization. Innovative care for chronic conditions: building blocks for action: global report. Geneva: World Health Organization; 2002.
-
6.
World Health Organization. Peer Support program in diabetes. Report of a WHO consultation, 5‑7 November 2007. Geneva: World Health Organization; 2008.
-
7.
Boothroyd RI, Fisher EB. Peers for progress: Promoting peer support for health around the world. Fam Pract. 2010;27 Suppl 1:i62-8. [PubMed ID: 20483801]. https://doi.org/10.1093/fampra/cmq017.
-
8.
Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. 2009;32 Suppl 1:S87-94. [PubMed ID: 19118294]. [PubMed Central ID: PMC2613581]. https://doi.org/10.2337/dc09-S087.
-
9.
Khan AR, Fariduddin M, Mollah SA, Ahmed T, Chowdhury WA, Ashrafuzzaman SM. Mahtab H, Latif ZA, Pathan MF, editors. Clinical management of diabetes mellitus in bangladesh: Principles and guidelines. Dhaka, Bangladesh: Clinical Research Group, Bangladesh Endocrine Society; 2013.
-
10.
Saleh F, Mumu SJ, Ara F, Begum HA, Ali L. Knowledge and self-care practices regarding diabetes among newly diagnosed type 2 diabetics in Bangladesh: A cross-sectional study. BMC Public Health. 2012;12:1112. [PubMed ID: 23267675]. [PubMed Central ID: PMC3552981]. https://doi.org/10.1186/1471-2458-12-1112.
-
11.
Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in African American veterans: A randomized trial. Ann Intern Med. 2012;156(6):416-24. [PubMed ID: 22431674]. [PubMed Central ID: PMC3475415]. https://doi.org/10.7326/0003-4819-156-6-201203200-00004.
-
12.
Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, Walker C, Gallo LC. Peer-led diabetes education programs in high-risk Mexican Americans improve glycemic control compared with standard approaches: A Project Dulce promotora randomized trial. Diabetes Care. 2011;34(9):1926-31. [PubMed ID: 21775748]. [PubMed Central ID: PMC3161298]. https://doi.org/10.2337/dc10-2081.
-
13.
Davidson L, Chinman M, Kloos B, Weingarten R, Stayner D, Tebes JK. Peer support among individuals with severe mental illness: A review of the evidence. Clin Psychol Sci Pract. 1999;6(2):165-87. https://doi.org/10.1093/clipsy.6.2.165.
-
14.
Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A. Health related virtual communities and electronic support groups: Systematic review of the effects of online peer to peer interactions. BMJ. 2004;328(7449):1166. [PubMed ID: 15142921]. [PubMed Central ID: PMC411092]. https://doi.org/10.1136/bmj.328.7449.1166.
-
15.
Parry M, Watt-Watson J. Peer support intervention trials for individuals with heart disease: A systematic review. Eur J Cardiovasc Nurs. 2010;9(1):57-67. [PubMed ID: 19926339]. https://doi.org/10.1016/j.ejcnurse.2009.10.002.
-
16.
Fisher EB, Boothroyd RI, Coufal MM, Baumann LC, Mbanya JC, Rotheram-Borus MJ, et al. Peer support for self-management of diabetes improved outcomes in international settings. Health Aff (Millwood). 2012;31(1):130-9. [PubMed ID: 22232103]. [PubMed Central ID: PMC4128379]. https://doi.org/10.1377/hlthaff.2011.0914.
-
17.
Mash RJ, Rhode H, Zwarenstein M, Rollnick S, Lombard C, Steyn K, et al. Effectiveness of a group diabetes education programme in under-served communities in South Africa: A pragmatic cluster randomized controlled trial. Diabet Med. 2014;31(8):987-93. [PubMed ID: 24766179]. [PubMed Central ID: PMC4232864]. https://doi.org/10.1111/dme.12475.
-
18.
Debussche X, Besancon S, Balcou-Debussche M, Ferdynus C, Delisle H, Huiart L, et al. Structured peer-led diabetes self-management and support in a low-income country: The ST2EP randomised controlled trial in Mali. PLoS One. 2018;13(1). e0191262. [PubMed ID: 29357380]. [PubMed Central ID: PMC5777645]. https://doi.org/10.1371/journal.pone.0191262.