Abstract
Background:
Nosocomial infections have increasingly resulted in death and the patients should bear high treatment costs. Members of the medical team could play an important role in prevention and control of nosocomial infections.Objectives:
The purpose of this research was the evaluation of nosocomial infections in patients admitted to Naft grand hospital in Ahvaz, Iran, during 2013.Patients and Methods:
This was a descriptive study, conducted prospectively during 12 months from March 2013 to March 2014 in Naft grand hospital in Ahvaz, Iran. All the patients who were hospitalized with no signs and symptoms of infection before the first 48 hours of hospitalization and presenting signs and symptoms of infection after 48 hours of hospitalization were included in this study. The patients’ age, gender, site of infection, ward of hospitalization and type of nosocomial infection were collected. The results were analyzed by Excel and SPSS 16.0.Results:
The results of the present study showed that the incidence of nosocomial infections was low (i.e., < 2%). The incidence rates of nosocomial infections were 36.78% in the intensive care unit (ICU), 46.55% in the internal medicine ward, 14.94% in the surgical medicine ward and 1.72% in the coronary care unit (CCU). Regarding the etiology of infection, Escherichia coli was found in 43.10%, coagulase-positive Staphylococci in 17.24%, coagulase-negative Staphylococci in 14.95% and Klebsiella in 10.34% of the cases. In our hospital, E. coli was the most frequent pathogen.Conclusions:
In this study, nosocomial infections had a lower frequency in comparison with the national rates. According to researches, hospitals have been able to reduce nosocomial infections by establishing strategies and getting the risks under control.Keywords
1. Background
Nosocomial infections occur 48 to 72 hours after hospital admission, due to a person’s stay in the hospital (1, 2). Nosocomial infections increase mortality, disability, hospitalization time, hospital costs and the incidence of health problems. Therefore, the prevention of hospital infection through identification and removal of cases can be very effective (3). The most common endemic infections are respiratory, urinary, skin and soft tissue, and gastrointestinal infections (4). Escherichia coli, Salmonella, Clostridium difficile and small round enteric viruses are common causes of outbreaks of gastrointestinal infections (4, 5). Although the efforts made in nosocomial infection control has been associated with some success, recent advances in medical sciences and medical interventions have carried out repeated massive consumption of drugs to inhibit the immune system as well as antibiotics prescription in vulnerable people, which has led to resistance to antibiotics (6). In many cases, nosocomial infection cause death of patients which is increasing among hospital admissions and its treatment is very difficult (4, 6). The treatment of nosocomial infections due to resistance to a variety of pharmaceutical antibiotics can be very difficult, especially for infections caused by strains that are hard to eliminate, which are sometimes caused due to being hospitalized and impose waste of time and extra costs to patients and the hospital (7, 8).
Nosocomial infections result in up to 4.5 billion dollar in additional healthcare expenses annually and affect approximately two million persons each year and nearly 90000 individuals among hospitalized patients die due to this incidence (9-13). Surgical site infections (SSIs) are defined as infections occurring at least two days after an operative procedure. Urinary tract infection (UTI) is defined as a patient with the following symptoms with no other recognizable cause: fever, dysuria and positive dipstick for leukocyte esterase and/or nitrate, physician diagnosis of a UTI, or both. A case of pneumonia is defined as a patient who has dullness to percussion on physical examination of the chest, abnormal chest radiography, or new onset of purulent sputum. A case of Bloodstream Infection (BSI) is defined as a patient with at least one of the following signs or symptoms with no other recognized cause: fever, hypotension and no apparent infection at another site, and physician instituted treatment for sepsis (14). The results of different studies have shown that by spending much costs related to diagnosis and education can be decrease the rate of nosocomial infections (15-18). The status of the patient and the type of hospital can be associated with the nosocomial infection (6, 8, 19, 20). In a study by Maa et al. (21) in Taiwan on 2688 patients with nosocomial infections, the rate of infection was about 40%. In another study in Italy, pulmonary infection was the most common nosocomial infection and the duration of hospitalization in hospital infections was an important effective factor (22). Based on the report by Bergmans et al. (23) pulmonary infection with a rate of 30% was the most common nosocomial infection. In another study in the hospital of Arak, Iran, the rates of surgical infections were high and in the ICU ward, due to invasive procedures, the maximum of infection cases occurred (24). According to the national nosocomial infections surveillance report in 2006, 8833 device-related infections in adults were reported from participating healthcare facilities (25, 26). The results of our study showed that an increase in the health worker care knowledge can be reduced the rate of nosocomial infections (27).
2. Objectives
The aim of this study was to evaluate the nosocomial infections in patients admitted to a hospital as well as the frequency and prevalence of microorganisms isolated in Naft grand hospital in Ahvaz, Iran, during 2013.
3. Patients and Methods
This descriptive study was conducted from March 2013 to March 2014 in Naft grand hospital with approximately 300 beds, in the southwest of Iran. The criteria for the diagnosis of nosocomial infections were based on the United States centers for disease control and prevention (CDC) definitions (17, 28, 29). Patients staying more than 48 hours in different parts of the hospital who acquired the infection were studied. We obtained the patients’ information from the hospital information system with the help of the members in the infection control committee. Nosocomial Infections were categorized according to the national nosocomial infections surveillance (NNIS) system (30-33). Data collection was designed based on a questionnaire according to the operating system and the original NNIS infection (UTI, pneumonia, BSI, and SSIs), which was conducted based on the national surveillance system guidelines (30-33). In this study, based on the infection type, the control supervisors reported cases of infection, wards in which the infections occurred and the sampling methods and after consultation with the infectious diseases specialist of the hospital. Sampling was performed randomly from patients with infections including CBC, urine, chest x-ray and blood culture. In this study, the patients who died in less than 48 hours of the study were under the police discretion. The patients’ age, gender, site of infection, ward of hospitalization and type of microbial infection were analyzed by SPSS 16.0.
4. Results
This study was conducted on more than 16936 admitted patients to Naft grand hospital in Ahvaz during 2013; 174 patients were identified with symptoms of nosocomial infections, in which the prevalence of E. coli and coagulase-positive Staphylococci were more than other species, respectively. The mean age of patients with symptoms of nosocomial infections was 51.7 ± 24.6 years, ranging 5 - 90 years. Most of these infections were observed in patients older than 50 years. The number of admitted patients and the incidence rates of nosocomial infection in the hospital wards are presented in Table 1.
| Hospital Ward | Patients in a Year, No. | New Cases of Infection Per Year, No. | Cases of Infection in Hospital Per Year, % |
|---|---|---|---|
| ICU | 249 | 64 | 25.7 |
| Internal wards | 4030 | 81 | 2.11 |
| General surgery | 4111 | 26 | 0.632 |
| CCU | 150 | 3 | 2.05 |
| Total | 8540 | 174 | 2.0374 |
Totally, the incidence of nosocomial infections was 2.0374% in Naft grand hospital in Ahvaz. UTI was the most frequent category of infections (56.32%), followed by pneumonia (37. 35%), SSI (5.74%) and BSI (0.57%) (Table 2). Based on Table 2, UTI compared to other types was the most frequent category of infection.
| Hospital Ward | Pneumonia | UTI | SSI | BSI | Infection in Wards Per Total Infections |
|---|---|---|---|---|---|
| ICU | 45 (25.86) | 18 (10.34) | - | 1 (0.57) | 64 (36.78) |
| Internal wards | 16 (9.2) | 61 (35.05) | 4 (2.3) | - | 81 (46.55) |
| General surgery | 3 (1.72) | 17 (9.77) | 6 (3.44) | - | 26 (14.94) |
| CCU | 1 (0.57) | 2 (1.14) | - | - | 3 (1.72) |
| Total | 65 (37.35) | 98 (56.32) | 10 (5.74) | 1 (0.57) | 174 (100) |
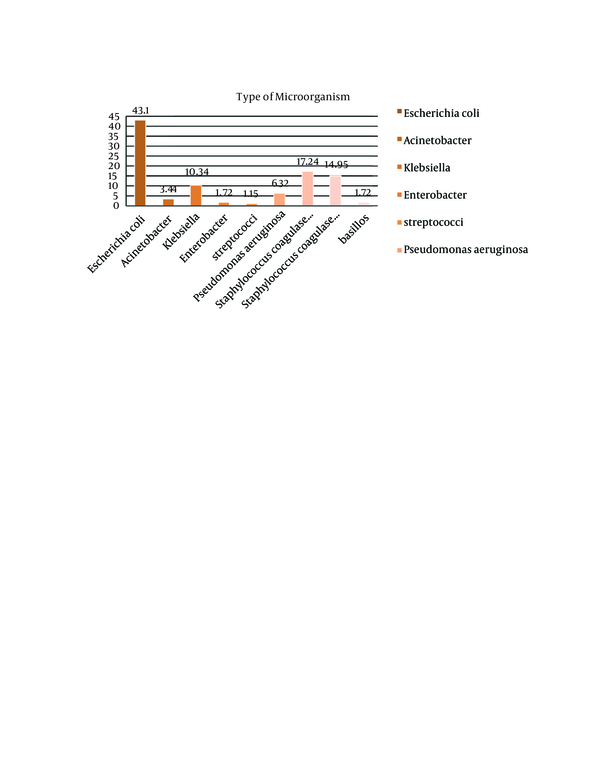
The predominant bacteria in internal wards, ICU, general surgery ward and CCU were coagulase-positive Staphylococci, E. coli, coagulase-negative Staphylococci and Klebsiella. In the ICU ward, E. coli was the most frequent pathogen (n = 26, 14.94%). Totally, the most isolated bacteria in Naft grand hospital was E. coli (n = 75, 43.10%), followed by coagulase-positive Staphylococci (n = 30, 17.24%), coagulase-negative Staphylococci (n = 26, 14.95%), Klebsiella (n = 18, 10.34%), Pseudomonas aeruginosa (n = 11, 6.32%) and Acinetobacter (n = 6, 3.44%) (Table 3).
| Microorganism | ICU | Internal Wards | General Surgery | CCU | Infection in Wards Per Total Infections |
|---|---|---|---|---|---|
| Escherichia coli | 26 (14.94) | 37 (21.26) | 10 (5.75) | 2 (1.15) | 75 (43.10) |
| Acinetobacter | 2 (1.15) | 4 (2.3) | - | - | 6 (3.44) |
| Klebsiella | 8 (4.6) | 7 (4.02) | 3 (1.72) | - | 18 (10.34) |
| Enterobacter | - | 2 (1.15) | 1 (0.57) | - | 3 (1.72) |
| Streptococci | - | 2 (1.15) | - | - | 2 (1.15) |
| Pseudomonas aeruginosa | 4 (2.3) | 5 (2.87) | 2 (1.15) | - | 11 (6.32) |
| coagulase-positive Staphylococci | 14 (8.05) | 11 (6.32) | 5 (2.87) | - | 30 (17.24) |
| coagulase-negative Staphylococci | 10 (5.75) | 10 (5.75) | 5 (2.87) | 1 (0.57) | 26 (14.95) |
| Bacillus | - | 3 (1.72) | - | - | 3 (1.72) |
| Total | 64 (36.78) | 81 (46.55) | 26 (14.94) | 3 (1.72) | 174 (100) |
The prevalence of pathogens causing nosocomial infections based on the type of Microorganism are shown in Figure 1. As Figure 1 indicates, E. coli was the most frequent pathogen.
Nosocomial Infections Based on Type of Microorganism in Naft Grand Hospital in 2013
5. Discussion
Based on the results of this research, the incidence of nosocomial infections was 2.04%, which was lower compared to rates of referenced nosocomial infections in the guideline book. According to Table 1, the rates of ICU, internal wards, general surgery and CCU patients’ nosocomial infections were very sensitive to the type of ward. Gender was not a risk factor for nosocomial infections in our study; however, females (54.6%) were more susceptible to nosocomial infections than males. In a study by Oncul et al. (34) gender was a risk factor for nosocomial infections, but in a study by Javanbakht et al. (14) it was not a risk factor.
Based on result this study, the prevalence rate of nosocomial infections was 1.03% in Naft grand hospital in Ahvaz. In a study by Amini et al. (24) the prevalence rate of nosocomial infection was about 36%. Luzzati et al. (22) reported the incidence of nosocomial infection about 30%. The reason for this conflict can be due to the lack of reported cases of infection and the use of less invasive methods of treatment on patients.
In the present study, there was a significant relationship between the age of the patients and the rate of infection. In studies by Luzzati et al. (22) and Su et al. (33), a significant relationship between the age of patients and the rate of infection was also reported. Based on the results of this study, E. coli was the most frequent pathogen, but in Javanbakht et al. (14) survey on the incidence of cross infections in Imam Reza Hospital of Mashhad, Klebsiella was the most frequent pathogen.
As the results showed, UTI was the most common site of infection in Naft grand hospital in Ahvaz. In a similar work by Pellizzer et al. (35) in Italy, urinary tract (28.4%), surgical sites (20.3%) and bloodstream (19.3%) were the most frequent sites of infections, respectively. based on the study of Javanbakht et al. (14) in Mashhad and the results reported by Appelgren et al. (36), SSI was the most common site of infection. Luzzati et al. (22) reported that pneumonia was the most common site of infection. These differences may be due to the number of patients, study location and genetic susceptibility.
The rates of nosocomial infections increased in the elderly due to their weak immune systems. According to Table 1, the incidence rates of nosocomial infections in the ICU compared to other wards were the most common, due to the use of invasive procedures, the severity of diseases and periodic hospitalization. In Zolldann et al. (8), Unal and Garcia-Rodriguez (7), Jeong et al. (37) and Kaoutar et al. (38) studies, ICU was the most common site of infection compared to other wards.
Our data demonstrated that E. coli, coagulase-positive Staphylococci, coagulase-negative Staphylococci and Klebsiella mainly played a major role in causing nosocomial infections in 2013 which is consistent with some other studies conducted in Iran. Sohrabi et al. (39) showed that E. coli, coagulase-negative Staphylococci and Klebsiella were the most common microorganisms in their hospital.
In conclusion, although the incidence rate of nosocomial infections in this hospital was low, medical and hygiene interventions such as wearing sterile gloves, hand washing, especially for the health-related personnel, education on health, continuous supervision, correct use of disposable equipment, controlled use of antibiotics, precise care of surgical wounds, using air conditioner in each patient’s room, keeping infected patients away from other patients, appropriate nutrition, and sufficient number of nurses are the most important to be considered to reduce nosocomial infections and their adverse effects.
Acknowledgements
References
-
1.
Medeiros EA, Grinberg G, Rosenthal VD, Bicudo Angelieri D, Buchner Ferreira I, Bauer Cechinel R, et al. Impact of the International Nosocomial Infection Control Consortium (INICC) multidimensional hand hygiene approach in 3 cities in Brazil. Am J Infect Control. 2015;43(1):10-5. [PubMed ID: 25564118]. https://doi.org/10.1016/j.ajic.2014.10.001.
-
2.
Mitchell BG, Russo PL. Preventing healthcare-associated infections: the role of surveillance. Nurs Stand. 2015;29(23):52-8. [PubMed ID: 25649603]. https://doi.org/10.7748/ns.29.23.52.e9609.
-
3.
Dasgupta S, Das S, Chawan NS, Hazra A. Nosocomial infections in the intensive care unit: Incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med. 2015;19(1):14-20. [PubMed ID: 25624645]. https://doi.org/10.4103/0972-5229.148633.
-
4.
Mathei C, Niclaes L, Suetens C, Jans B, Buntinx F. Infections in residents of nursing homes. Infect Dis Clin North Am. 2007;21(3):761-72. ix. [PubMed ID: 17826622]. https://doi.org/10.1016/j.idc.2007.07.005.
-
5.
Nicolle LE. Preventing infections in non-hospital settings: long-term care. Emerg Infect Dis. 2001;7(2):205-7. [PubMed ID: 11294707]. https://doi.org/10.3201/eid0702.700205.
-
6.
Eriksen HM, Iversen BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect. 2005;60(1):40-5. [PubMed ID: 15823655]. https://doi.org/10.1016/j.jhin.2004.09.038.
-
7.
Unal S, Garcia-Rodriguez JA. Activity of meropenem and comparators against Pseudomonas aeruginosa and Acinetobacter spp. isolated in the MYSTIC Program, 2002-2004. Diagn Microbiol Infect Dis. 2005;53(4):265-71. [PubMed ID: 16360550]. https://doi.org/10.1016/j.diagmicrobio.2005.10.002.
-
8.
Zolldann D, Haefner H, Poetter C, Buzello S, Sohr D, Luetticken R, et al. Assessment of a selective surveillance method for detecting nosocomial infections in patients in the intensive care department. Am J Infect Control. 2003;31(5):261-5. [PubMed ID: 12888760].
-
9.
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, et al. Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med. 2002;28(2):108-21. [PubMed ID: 11907653]. https://doi.org/10.1007/s00134-001-1143-z.
-
10.
Black SR, Weaver KN, Weinstein RA, Hayden MK, Lin MY, Lavin MA, et al. Regional infection control assessment of antibiotic resistance knowledge and practice. Infect Control Hosp Epidemiol. 2015;36(4):381-6. [PubMed ID: 25782891]. https://doi.org/10.1017/ice.2014.78.
-
11.
Chaudhuri AK. Infection control in hospitals: has its quality-enhancing and cost-effective role been appreciated? J Hosp Infect. 1993;25(1):1-6. [PubMed ID: 7901272].
-
12.
Haley RW, Culver DH, White JW, Morgan WM, Emori TG, Munn VP, et al. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol. 1985;121(2):182-205. [PubMed ID: 4014115].
-
13.
Horstman MJ, Li YF, Almenoff PL, Freyberg RW, Trautner BW. Denominator Doesn't Matter: Standardizing Healthcare-Associated Infection Rates by Bed Days or Device Days. Infect Control Hosp Epidemiol. 2015;36(6):710-6. [PubMed ID: 25782986]. https://doi.org/10.1017/ice.2015.42.
-
14.
Javanbakht A, Askari E, Danesh L, Moghadas N, Mostafavi I, Naderinasab M. The incidence of cross infections in Imam Reza hospital, Mashhad, Iran. Iran J Microbiol. 2012;4(4):177-9. [PubMed ID: 23205248].
-
15.
Agarwal M, Thomas P. Prevalence of post-op. nosocomial infection in neurosurgical patients and associated risk factors--a prospective study of 2441 patients. Nurs J India. 2003;94(9):197-8. [PubMed ID: 15315200].
-
16.
Conterno LO, Shymanski J, Ramotar K, Toye B, Zvonar R, Roth V. Impact and cost of infection control measures to reduce nosocomial transmission of extended-spectrum beta-lactamase-producing organisms in a non-outbreak setting. J Hosp Infect. 2007;65(4):354-60. [PubMed ID: 17289215]. https://doi.org/10.1016/j.jhin.2006.12.014.
-
17.
Crivaro V, Bogdanovic L, Bagattini M, Iula VD, Catania M, Raimondi F, et al. Surveillance of healthcare-associated infections in a neonatal intensive care unit in Italy during 2006-2010. BMC Infect Dis. 2015;15:152. [PubMed ID: 25885702]. https://doi.org/10.1186/s12879-015-0909-9.
-
18.
Wilson MP, Spencer RC. Laboratory role in the management of hospital acquired infections. J Hosp Infect. 1999;42(1):1-6. [PubMed ID: 10363204].
-
19.
Askarian M, Gooran NR. National nosocomial infection surveillance system-based study in Iran: additional hospital stay attributable to nosocomial infections. Am J Infect Control. 2003;31(8):465-8. [PubMed ID: 14647108].
-
20.
Gastmeier P, Geffers C, Schwab F, Fitzner J, Obladen M, Ruden H. Development of a surveillance system for nosocomial infections: the component for neonatal intensive care units in Germany. J Hosp Infect. 2004;57(2):126-31. [PubMed ID: 15183242]. https://doi.org/10.1016/j.jhin.2003.12.038.
-
21.
Maa SH, Lee HL, Huang YC, Wu JH, Tsou TS, MacDonald K, et al. Incidence density and relative risk of nosocomial infection in Taiwan's Only Children's Hospital, 1999-2003. Infect Control Hosp Epidemiol. 2008;29(8):767-70. [PubMed ID: 18690787]. https://doi.org/10.1086/589724.
-
22.
Luzzati R, Antozzi L, Bellocco R, Del Bravo P, Mirandola M, Procaccio F, et al. [Prevalence of nosocomial infections in Intensive Care Units in Triveneto area, Italy]. Minerva Anestesiol. 2001;67(9):647-52. [PubMed ID: 11731755].
-
23.
Bergmans DC, Bonten MJ, Gaillard CA, van Tiel FH, van der Geest S, de Leeuw PW, et al. Indications for antibiotic use in ICU patients: a one-year prospective surveillance. J Antimicrob Chemother. 1997;39(4):527-35. [PubMed ID: 9145828].
-
24.
Amini M, Sanjary L, Vasei M, Alavi S. Frequency Evaluation of The Nosocomial Infections and Related Factors in Mostafa Khomeini Hospital" ICU" Based on" NNI" System. J Ardabil Univ Med Sci. 2009;7(1):9-14.
-
25.
Edwards JR, Peterson KD, Andrus ML, Tolson JS, Goulding JS, Dudeck MA, et al. National Healthcare Safety Network (NHSN) Report, data summary for 2006, issued June 2007. Am J Infect Control. 2007;35(5):290-301. [PubMed ID: 17577475]. https://doi.org/10.1016/j.ajic.2007.04.001.
-
26.
Reed D, Kemmerly SA. Infection control and prevention: a review of hospital-acquired infections and the economic implications. Ochsner J. 2009;9(1):27-31. [PubMed ID: 21603406].
-
27.
Askarian M, Hosseini RS, Kheirandish P, Assadian O. Incidence and outcome of nosocomial infections in female burn patients in Shiraz, Iran. Am J Infect Control. 2004;32(1):23-6. [PubMed ID: 14755231]. https://doi.org/10.1016/j.ajic.2003.03.004.
-
28.
Giamarellou H. Nosocomial cardiac infections. J Hosp Infect. 2002;50(2):91-105. [PubMed ID: 11846535]. https://doi.org/10.1053/jhin.2001.1144.
-
29.
van der Zwet WC, Kaiser AM, van Elburg RM, Berkhof J, Fetter WP, Parlevliet GA, et al. Nosocomial infections in a Dutch neonatal intensive care unit: surveillance study with definitions for infection specifically adapted for neonates. J Hosp Infect. 2005;61(4):300-11. [PubMed ID: 16221510]. https://doi.org/10.1016/j.jhin.2005.03.014.
-
30.
Assar S, Akhoundzadeh R, Aleali AM, Latifi SM, Salemzadeh M. Survey of nosocomial infections and causative bacteria: A hospital-based study. Pak J Md sci. 2012;28(3).
-
31.
Cuellar LE, Fernandez-Maldonado E, Rosenthal VD, Castaneda-Sabogal A, Rosales R, Mayorga-Espichan MJ, et al. Device-associated infection rates and mortality in intensive care units of Peruvian hospitals: findings of the International Nosocomial Infection Control Consortium. Rev Panam Salud Publica. 2008;24(1):16-24. [PubMed ID: 18764990].
-
32.
Babazono A, Kitajima H, Nishimaki S, Nakamura T, Shiga S, Hayakawa M, et al. Risk factors for nosocomial infection in the neonatal intensive care unit by the Japanese Nosocomial Infection Surveillance (JANIS). Acta Med Okayama. 2008;62(4):261-8. [PubMed ID: 18766209].
-
33.
Su BH, Hsieh HY, Chiu HY, Lin HC, Lin HC. Nosocomial infection in a neonatal intensive care unit: a prospective study in Taiwan. Am J Infect Control. 2007;35(3):190-5. [PubMed ID: 17433943]. https://doi.org/10.1016/j.ajic.2006.07.004.
-
34.
Oncul O, Ulkur E, Acar A, Turhan V, Yeniz E, Karacaer Z, et al. Prospective analysis of nosocomial infections in a burn care unit, Turkey. Indian J Med Res. 2009;130(6):758-64. [PubMed ID: 20090139].
-
35.
Pellizzer G, Mantoan P, Timillero L, Allegranzi B, Fedeli U, Schievano E, et al. Prevalence and risk factors for nosocomial infections in hospitals of the Veneto region, north-eastern Italy. Infection. 2008;36(2):112-9. [PubMed ID: 18327681]. https://doi.org/10.1007/s15010-007-7092-x.
-
36.
Appelgren P, Hellstrom I, Weitzberg E, Soderlund V, Bindslev L, Ransjo U. Risk factors for nosocomial intensive care infection: a long-term prospective analysis. Acta Anaesthesiol Scand. 2001;45(6):710-9. [PubMed ID: 11421829].
-
37.
Jeong SH, Bae IK, Kwon SB, Lee K, Yong D, Woo GJ, et al. Investigation of a nosocomial outbreak of Acinetobacter baumannii producing PER-1 extended-spectrum beta-lactamase in an intensive care unit. J Hosp Infect. 2005;59(3):242-8. [PubMed ID: 15694982]. https://doi.org/10.1016/j.jhin.2004.09.025.
-
38.
Kaoutar B, Joly C, L'Heriteau F, Barbut F, Robert J, Denis M, et al. Nosocomial infections and hospital mortality: a multicentre epidemiology study. J Hosp Infect. 2004;58(4):268-75. [PubMed ID: 15617231].
-
39.
Sohrabi MB, Khosravi A, Zolfaghari P, Sarrafha J. Evaluation of nosocomial infections in Imam Hossein (as) Hospital of Shahrood, 2005. J Birjand Univ Med Sci. 2009;16(3):33-9.