Abstract
Background:
Mental distress is a group of mental problems manifested by symptoms of insomnia, fatigue, irritability, forgetfulness, difficulty in concentrating, and somatic complaints. University students have more severe mental health problems than the general population.Objectives:
Therefore, this study attempted to assess the magnitude of mental distress and its determinants among medical and health science regular undergraduate students at Jimma University.Methods:
A descriptive institutional-based with cross-sectional study design was conducted at Jimma University from March to April 2017 on regular undergraduate medical and health science students of the Faculty of Health Science. Study participants were selected from each batch using simple random sampling techniques and from the department by lottery method. Mental distress was assessed by using Self-Reporting questionnaire-20. Participants with score of eight and above on the Self-Reporting questionnaire-20 were considered as having mental distress. Chi-square and descriptive statistics were done using SPSS-20.Results:
From a total of 369 study participants, about 354 gave the response rate of (95.9%). The magnitude of mental distress among medical and health science students was 35.03 %. Most of the respondents were males by sex and the mean age of the respondents was 23 years with SD ± 6. Age, sex, year of study, the practice of religion, presence of family history of mental illness, department choice, and ever use of substance (chat chewing and alcohol) were predictor variables and significantly associated with mental distress at P < 0.05.Conclusions:
The magnitude of mental distress in our study was 35.03% and it needs intervention and addressing the mentioned factors significantly associated with mental distress.Keywords
1. Background
Mental distress (or psychological distress) is a term used to describe symptoms and experiences of a person’s internal life that are commonly held to be troubling, confusing or out of the ordinary activity (1, 2).
Although mental distress affect any one numerous studies reported that high burden of mental distress found in university students compared to the other general population (3, 4), despite that its burden varies considerably from nation to nation or country to country according to previous studies finding, the magnitude of mental distress at French was 25.7% in first-year university students (5), in Australian 67.4% (6), in America 82% (7), in Canada 30% (8), in Malaysia 41.9% (9), University of Hargeisa, Somaliland 19.8% (10), and in Ethiopia(low income country), it ranges of 21.6% - 49.1% in different universities (11-16).
The reason behind the high burden of mental distress is because of university students have multiple stressors including academic load, constant pressure to succeed, academic competition with peers, financial burden, peer, teacher or parental pressure as well as concerns and worry about their future (17-19). Stress throughout education can lead to mental distress and harm cognitive functioning and learning (20-22), especially, it is more common among medical and health science students due to specific reasons like the nature of their education and separation from preexisting social support (19, 22-25).
So in university students, it is an important health challenge (26, 27), but it is under-recognized and possible factors were not well addressed especially among medical and health science students.
2. Objectives
This study attempted to assess the magnitude of mental distress and factors associated with mental distress at Jimma University medical and health science which will be helpful for different stakeholders and mental health professionals to intervene the factors accordingly.
3. Methods
3.1. Study Area and Samples
The study conducted in Jimma University on the Faculty of medical and Health Science undergraduate students from April 1, 2017, to May 31, 2017. Jimma University is located in Jimma Town, and 346 km far away from the capital city of Ethiopia, Addis Ababa. Faculty of Health Science is found in Jimma University-Main Campus, it was established in 1983, and currently, it has 10 departments with 3472 students.
All undergraduate faculties of medical and health science students of Jimma University were source populations where as all selected medical and health science students of Jimma University in 2017 were study populations.
Institutional based cross-sectional study design was used.
The sample size was determined by using single population proportion formula by taking prevalence from the previous study (40.9%) from University of Gondar (21), 95% confidence interval with 5% margin error.
Where Zα/2 = 1.96, d = 0.05 = 5%, p = 0.409
n = 371, since the source population is smaller than 10,000, population correction formula was used to determine adjusted minimum sample size as follows:
Where; n = a minimum sample size, N = total number of health science students, NF = minimum final sample size, Thus:
Considering non-response rate, 10% the total sample size became 369.
Inclusion and exclusion criteria were as follows; Health Science students who attained their education at Jimma University in the 2017 year of study were part of study whereas students asked withdrawal before data collection and who can’t able to fill to the questioners at the time of data collection excluded from the study.
3.2. Data Collection
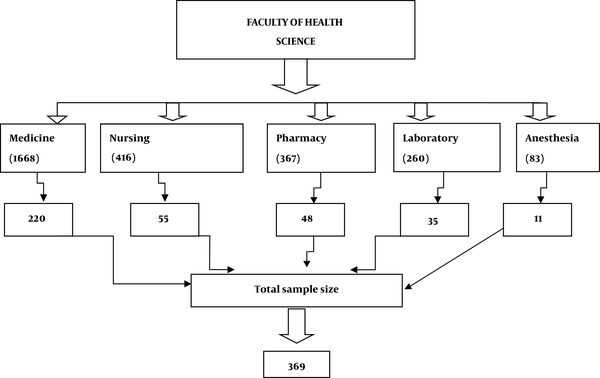
Stratified random sampling technique applied to select the participants’. The variable of stratification were years of study of students, and assuming that their mental status may be different as their year of study increased because it influences their behavior. Out of 10 departments, a lottery method was used to pick the department and then the departments were categorized into their batches to pick the proportion of students per the number of students in their batch. Thus, Medicine, Pharmacy, Nursing, Medical laboratory, and Anesthesia were selected. Then for each department, samples were proportionally allocated (Figure 1). After that again it was reallocated to their year of study and by using the name list of students’ then participants selected randomly by using lottery method and approached individually by the principal investigator at the time when they finished their class and they informed to fill the prepared questioners individually.
Sampling technique used to get study participants
First questionnaires were prepared in English language containing socio-demographic characteristics and associated factors of mental distress after exhaustive reviewing of different and relevant literature and translated into local languages (Afan Oromo and Amharic). Data collected by using Self-Reporting questionnaire-20, self-administered structured questionnaires to assess mental distress with a cut-off point eight and above (28).
3.3. Data Analysis
The collected data were cleaned, checked for completeness, coded and entered into Epi-data version 3.1software and exported to SPSS version 20 statistical software for analysis. Descriptive statistics used to summarize the results. Chi-square tests were done to see the relation between dependent and independent variables at P value < 0.05 and predictor variables were declared at P value < 0.05. Finally, the obtained results presented using narration and tables.
3.4. Ethical Considerations
Before data collection, ethical clearance and approval obtained from Jimma University, College of Health Science and Medicine, Department of Nursing. Approval ethical code was IHRB/300/2017.
Written informed consent was obtained from the involved participants for their participation after the nature of the study was fully explained to them. The right to withdraw was respected, confidentiality kept and data collection was done respectfully.
Study participants who were positive for mental distress at the time of screening by adding the positive response after they filled the questioners were referred and linked to Jimma university Medical Center Psychiatric Clinic for further assessment and treatment.
4. Results
Among 369 of the total study participants, 354 filled the questioners properly with the response rate was 95.9%. Mean age of the respondents was 23 year with SD ± 6. The Majority of respondents were orthodox 143 (40.4%) followed by Muslim 117 (33.1%) by religion, and the majority of respondents were Oromo 228 (64.4%) followed by Amhara 71 (20%) by ethnicity (Table 1).
Sociodemographic Distribution of Respondents, at Jimma University, South West, Ethiopia, 2017a
| Variables | Values |
|---|---|
| Sex | |
| Male | 231 (65.3) |
| Female | 123 (34.7) |
| Religion | |
| Orthodox | 143 (40.4) |
| Muslim | 117 (33.1) |
| Protestant | 81 (22.9) |
| Othersb | 13 (3.6) |
| Ethnicity | |
| Oromo | 228 (64.4) |
| Amhara | 71 (20) |
| Tigre | 17 (4.8) |
| Othersc | 38 (10.7) |
| Current relationship status | |
| Single | 205 (58) |
| Have a boy or girlfriend | 92 (26) |
| Married | 39 (11) |
| Divorced | 18 (5) |
| Study year | |
| First year | 126 (35.6) |
| Second year | 149 (42.1) |
| Third year and above | 79 (22.3) |
| Department | |
| Medicine | 210 (59.3) |
| Nursing | 52 (14.7) |
| Pharmacy | 47 (13.3) |
| Medical Laboratory | 34 (9.6) |
| Anesthesia | 11 (3.1) |
| Income in birr per month | |
| 200 - 500 | 217 (61.3) |
| 600 - 900 | 107 (30.2) |
| > 900 | 30 (8.5) |
| Parental residence | |
| Rural | 215 (60.7) |
| Urban | 139 (39.3) |
| Current parental marital status | |
| Together | 279 (78.8) |
| Divorced | 62 (17.5) |
| Widowed | 13 (3.7) |
| Family history of mental illness | |
| Present | 79 (22.3) |
| Absent | 275 (77.7) |
4.1. Substance Use Status of Study Respondents
Regarding substance-using among 354 respondents 243 (68.6%) were chewing khat from this 103 (83.1%) were mentally distressed, 149 (42.1%) using alcohol from this 99 (79.8%) were mentally distressed, 63 (17.8%) were use tobacco from this 28 (22.6%) were mentally distressed, and 12 (3.4%) used none medicinal recreational drug from this 3 (2.4%) was mentally distressed. The highest prevalence of 121 (97.6%) of mental distress was found among students who were using non prescribed recreational drugs during our data collection period (Table 2).
Study Participants Pattern of Substance Use Among Jimma University Students, South West, Ethiopia, 2017a
| Substance | Ever Users | Having Mental Distress |
|---|---|---|
| Khat use | ||
| Users | 243 (68.6) | 103 (83.1) |
| Nonusers | 111 (31.4) | 21 (16.9) |
| Alcohol use | ||
| Users | 149 (42.1) | 99 (79.8) |
| Nonusers | 205 (57.9) | 25 (20.1) |
| Tobacco use | ||
| Users | 63 (17.8) | 28 (22.6) |
| Non-users | 291 (82.2) | 96 (77.4) |
| Current use of non-prescribed recreational drugs | ||
| No | 12 (3.4) | 3 (2.4) |
| Yes | 342 (96.6) | 121 (97.6) |
4.2. Magnitude of Mental Distress at Jimma University Medical and Health Science Students
Magnitude of mental distress among medical and health science students in this study using SRQ-20, with a cut-off point 8 and above was 124 (35.03 %) (Table 3).
4.3. Determinants of Mental Distress
According to chi-square age, sex, year of study, the practice of religion, history of mental illness in the family, department choice, and ever use of a substance (khat chewing and alcohol) has a significant association with mental distress at P < 0.05, whereas ever use of tobacco and current use of non-prescribed recreational drugs has no significant association with mental distress at P < 0.05.
Variables Associated with Mental Distress at Jimma University Students, South West, Ethiopia, 2017a
| Variables | Mental Distress | χ2 | P Value | ||
|---|---|---|---|---|---|
| Yes | No | Total | |||
| Age, y | 32.6008 | < 0.00001 | |||
| 18 - 24 | 74 (27.7) | 193 (72.3) | 267 (75.4) | ||
| 25 - 30 | 42 (65.6) | 22 (34.4) | 64 (18.1) | ||
| ≥ 31 | 8 (34.8) | 15 (65.2) | 23 (6.5) | ||
| Total | 124 (35.1) | 230 (64.9) | 354 (100) | ||
| Sex | 48.9924 | < 0.00001 | |||
| Female | 73 (59.4) | 50 (40.6) | 123 (34.7) | ||
| Male | 51 (22.1) | 180 (77.9) | 231 (65.3) | ||
| Study year | 16.6439 | 0.000243 | |||
| 1st year | 41 (32.5) | 85 (67.5) | 126 (35.6) | ||
| 2nd year | 68 (45.6) | 81 (54.4) | 149 (42.1) | ||
| 3rd year and above | 15 (18.9) | 64 (81.1) | 79 (22.3) | ||
| Frequency of attending religious practice | 155.6125 | < 0.00001 | |||
| Always (every day) | 11 (8) | 126 (92) | 137 (38.7) | ||
| Often (weekly) | 18 (18.8) | 78 (81.2) | 96 (27.1) | ||
| Some times (occasionally) | 42 (79.2) | 11 (20.8) | 53 (15) | ||
| Rarely (only in holidays) | 53 (77.9) | 15 (22.1) | 68 (19.2) | ||
| Family history of mental illness | 122.2877 | < 0.00001 | |||
| Yes | 69 (87.3) | 10 (12.7) | 79 (22.3) | ||
| No | 55 (20) | 220 (80) | 275 (77.7) | ||
| Department choice | 71.2837 | < 0.00001 | |||
| Preferred | 7 (5.7) | 116 (94.3) | 123 (34.7) | ||
| Not preferred | 117 (50.6) | 114 (49.4) | 231 (65.3) | ||
| Ever chewed Khat | 18.4588 | 0.000018 | |||
| Yes | 103 (42.4) | 140 (57.6) | 243 (68.6) | ||
| No | 21 (18.9) | 90 (81.1) | 111 (31.4) | ||
| Ever use alcohol | 111.5729 | < 0.00001 | |||
| Yes | 99 (66.4) | 50 (33.6) | 149 (42.1) | ||
| No | 25 (12.2) | 180 (87.8) | 205 (57.9) | ||
| Ever use tobacco | 2.9858 | 0.083998 | |||
| Yes | 28 (44.4) | 35 (55.6) | 63 (17.8) | ||
| No | 96 (33) | 195 (67) | 291 (82.2) | ||
| Current use of non-prescribed recreational drugs | 0.5489 | 0.458782 | |||
| No | 3 (25) | 9 (75) | 12 (3.4) | ||
| Yes | 121 (35.4) | 221 (64.6) | 342 (96.6) | ||
5. Discussion
This study revealed that the magnitude of mental distress was about 35.03%. This finding is lower than USA (57%) (7), Australia (53%) (6) and Malaysia (41.9%) (9) studies. This could be due to the socio-cultural and environmental factors difference between participants, and also lower than the study finding from Gondar University (40.9%) (12) and Adama University (21.6%) (15) Ethiopia. This might be due to the study time variation; the improvement of infrastructure and mental health service option provided by universities to the students in this time variation. However, the magnitude was higher than studies from French 25.7% (5), Canada (30%) (8) and Hargeisa, Somaliland (19.8%) (10), when compared within our country Universities, it is similar with the study done in the Addis Ababa University (32.6%) (16), Aksum University (39.6%) (14), and Hawassa University (30%) (13).
The magnitude of mental distress in our study was higher among female students as compared to their male students. The finding is similar with other studies at Aksum University (14), in Amritsar, Punjab, India (25), Hargeisa, Somaliland (10), and at the Kingdom of Saudi Arabia (22). This might be because of females able to express their emotions and high stress related to hormonal changes.
In this particular study history of mental illness in the family is strongly related with mental distress. This finding agrees with the study done in Gondar (12), Aksum University (14), and Adama (15). This might be due to the genetic causes of mental illness and stressful situations in the family.
This study shows that there is a significant relation between mental distress and ever use of a substance (chewing khat and drinking alcohol). A similar finding was reported from Hargeisa, Somaliland (10). This might be because of the high availability of khat in the area and the substance itself makes them vulnerable for mental distress.
Being the second year of study is significantly related with mental distress and consistent with the finding from Amritsar, Punjab, India (25) however it is not consistent with the findings of studies conducted in Adama (24) and Aksum (14). This might because of the environment they face and academic load (22).
Moreover, this study also identifies age and department choice has a significant association with mental distress at P < 0.05, which might result from thinking about their future career and payment and consistent with the finding from India (25), Saudi Arabia (22) and Aksum University (14).
This study also found that mental distress associated with religious practice, even though most literature didn’t consider religion as a variable. Students who were involved in the religious program, irrespective of what religion they follow, were less likely to develop mental distress, and consistent with studies done in Ethiopia (15, 29). This might be because of religious teachings and doctrines helps students with stress management. Furthermore, it facilitates the development different coping mechanisms.
In this study, parent marital condition, ethnicity, and substance use like tobacco smoking and current use of non-prescribed recreational drugs of the respondents were not associated with mental distress and similar findings reported (13, 16), but it needs investigating the time and process of parental relationship.
There were some limitations in this study it is difficult to know the cause-effect relationship because from its nature of the cross-sectional study and environmental factors which might affect mental distress not included in this study and it needs further study.
5.1. Conclusions
The prevalence of mental distress in this study was significantly high and it needs intervention and addressing the mentioned factors associated with mental distress.
Age, sex, year of study, the practice of religion, family history of mental illness, department choice, and ever use of substance (chat chewing and alcohol) has a significant association with mental distress.
Stress-prevention strategies for students who have any level of psychological stress are recommendable and helpful for them.
References
-
1.
Khudair F, Al-Amarei H, Khudair Z. A survey of determination the mental distress level among internally displaced person at Al-Najaf City. Am J Biomed. 2016;4(10):421-6. https://doi.org/10.18081/2333-5106/016-10/421-426.
-
2.
Doherty DT, Moran R, Kartalova-O'D. Y. Psychological distress, mental health problems and use of health services in Ireland. 2008. Available from: https://www.lenus.ie/handle/10147/336104.
-
3.
Gaspersz R, Frings-Dresen MH, Sluiter JK. Prevalence of common mental disorders among Dutch medical students and related use and need of mental health care: A cross-sectional study. Int J Adolesc Med Health. 2012;24(2):169-72. [PubMed ID: 22909932]. https://doi.org/10.1515/ijamh.2012.025.
-
4.
Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7:26. [PubMed ID: 17678553]. [PubMed Central ID: PMC1951961]. https://doi.org/10.1186/1472-6920-7-26.
-
5.
Saias T, du Roscoat E, Veron L, Guignard R, Richard JB, Legleye S, et al. Psychological distress in French college students: Demographic, economic and social stressors. Results from the 2010 National Health Barometer. BMC Public Health. 2014;14:256. [PubMed ID: 24629002]. [PubMed Central ID: PMC3995499]. https://doi.org/10.1186/1471-2458-14-256.
-
6.
Rosenthal B, Wilson WC. Mental health services: Use and disparity among diverse college students. J Am Coll Health. 2008;57(1):61-8. [PubMed ID: 18682347]. https://doi.org/10.3200/JACH.57.1.61-68.
-
7.
Dyrbye LN, Harper W, Durning SJ, Moutier C, Thomas MR, Massie FJ, et al. Patterns of distress in US medical students. Med Teach. 2011;33(10):834-9. [PubMed ID: 21942482]. https://doi.org/10.3109/0142159X.2010.531158.
-
8.
Adlaf EM, Gliksman L, Demers A, Newton-Taylor B. The prevalence of elevated psychological distress among Canadian undergraduates: Findings from the 1998 Canadian Campus Survey. J Am Coll Health. 2001;50(2):67-72. [PubMed ID: 11590985]. https://doi.org/10.1080/07448480109596009.
-
9.
Mohd Sidik S, Rampal L, Kaneson N. Prevalence of emotional disorders among medical students in a Malaysian university. Asia Pac Fam Med. 2003;2(4):213-7. https://doi.org/10.1111/j.1444-1683.2003.00089.x.
-
10.
Hersi L, Tesfay K, Gesesew H, Krahl W, Ereg D, Tesfaye M. Mental distress and associated factors among undergraduate students at the University of Hargeisa, Somaliland: A cross-sectional study. Int J Ment Health Syst. 2017;11:39. [PubMed ID: 28603551]. [PubMed Central ID: PMC5465570]. https://doi.org/10.1186/s13033-017-0146-2.
-
11.
Tesfaye A. Prevalence and correlates of mental distress among regular undergraduate students of Hawassa University: A cross sectional survey. East Afr J Public Health. 2009;6(1):85-94. [PubMed ID: 20000071]. https://doi.org/10.4314/eajph.v6i1.45755.
-
12.
Dachew BA, Azale Bisetegn T, Berhe Gebremariam R. Prevalence of mental distress and associated factors among undergraduate students of University of Gondar, Northwest Ethiopia: A cross-sectional institutional based study. PLoS One. 2015;10(3). e0119464. [PubMed ID: 25794278]. [PubMed Central ID: PMC4368633]. https://doi.org/10.1371/journal.pone.0119464.
-
13.
Melese B, Bayu B, Wondwossen F, Tilahun K, Lema S, Ayehu M, et al. Prevalence of mental distress and associated factors among Hawassa University medical students, Southern Ethiopia: A cross-sectional study. BMC Res Notes. 2016;9(1):485. [PubMed ID: 27821143]. [PubMed Central ID: PMC5100187]. https://doi.org/10.1186/s13104-016-2289-7.
-
14.
Tesfahunegn TB, Gebremariam EH. Mental distress and associated factors among Aksum University students, Ethiopia: A cross-sectional study. BMC Psychiatry. 2019;19(1):71. [PubMed ID: 30760233]. [PubMed Central ID: PMC6375136]. https://doi.org/10.1186/s12888-019-2051-5.
-
15.
Dessie Y, Ebrahim J, Awoke T. Mental distress among university students in Ethiopia: A cross sectional survey. Pan Afr Med J. 2013;15:95. [PubMed ID: 24198889]. [PubMed Central ID: PMC3810159]. https://doi.org/10.11604/pamj.2013.15.95.2173.
-
16.
Alem A, Araya M, Melaku Z, Wendimagegn D, Abdulahi A. Mental distress in medical students of Addis Ababa University. Ethiop Med J. 2005;43(3):159-66. [PubMed ID: 16370547].
-
17.
Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: A cross-sectional study. Med Educ. 2005;39(6):594-604. [PubMed ID: 15910436]. https://doi.org/10.1111/j.1365-2929.2005.02176.x.
-
18.
Cvetkovski S, Reavley NJ, Jorm AF. The prevalence and correlates of psychological distress in Australian tertiary students compared to their community peers. Aust N Z J Psychiatry. 2012;46(5):457-67. [PubMed ID: 22535294]. https://doi.org/10.1177/0004867411435290.
-
19.
Rahman NIA, Ismail S, Binti TNA, Seman T, Binti NFA, Mat SAB, et al. Stress among preclinical medical students of University Sultan Zainal Abidin. J Appli Pharm Sci. 2013;3(11):76.
-
20.
Saipanish R. Stress among medical students in a Thai medical school. Med Teach. 2003;25(5):502-6. [PubMed ID: 14522672]. https://doi.org/10.1080/0142159031000136716.
-
21.
Alzahem AM, van der Molen HT, Alaujan AH, Schmidt HG, Zamakhshary MH. Stress amongst dental students: A systematic review. Eur J Dent Educ. 2011;15(1):8-18. [PubMed ID: 21226800]. https://doi.org/10.1111/j.1600-0579.2010.00640.x.
-
22.
Alalwani B, Juhani A, Fallatah S, Abdulhaleem S. The prevalence of stress among medical students and its effects on academic performance in the kingdom of Saudi Arabia. Egypt J Hosp Med. 2018;71(5):3200-5. https://doi.org/10.12816/0046625.
-
23.
Firth-Cozens J. Medical student stress. Med Educ. 2008;35(1):6-7. https://doi.org/10.1111/j.1365-2923.2001.00832.x.
-
24.
Mitchell CU, LaGory M. Social capital and mental distress in an impoverished community. City Commun. 2008;1(2):199-222. https://doi.org/10.1111/1540-6040.00017.
-
25.
Mehta K, Kaur S, Girgla K, Kaur P, Kaur H. A study of mental distress in medical students. Natl J Physiol Pharm Pharmacol. 2015;5(3). https://doi.org/10.5455/njppp.2015.5.2810201415.
-
26.
Stallman HM. Prevalence of psychological distress in university students--implications for service delivery. Aust Fam Physician. 2008;37(8):673-7. [PubMed ID: 18704221].
-
27.
Middleton H, Shaw I. Distinguishing mental illness in primary care. We need to separate proper syndromes from generalised distress. BMJ. 2000;320(7247):1420-1. [PubMed ID: 10827025]. [PubMed Central ID: PMC1127622]. https://doi.org/10.1136/bmj.320.7247.1420.
-
28.
Beusenberg M, Orley J; World Health Organization. A user's guide to the Self-Reporting questionnaire (SRQ). World Health Organization; 1994. Available from: https://apps.who.int/iris/handle/10665/61113.
-
29.
Reta Y, Samuel T, Mekonnen M. Mental distress and associated factors among undergraduate engineering students of Hawassa University, Ethiopia. J Multidiscip Healthc. 2020;13:99-107. [PubMed ID: 32099377]. [PubMed Central ID: PMC6999758]. https://doi.org/10.2147/JMDH.S238113.