Abstract
Objectives:
Main goal in this study was to design and introduce a standard checklist that medical interns to be able to apply it to assess the medication safety status in clinical settings and learn the facts related to this issue simultaneously.Methods:
We performed the following steps to conduct the study: (1) using brainstorming and fishbone method for collecting problems in six domains including: demographic and risk factors, prescribing, transcribing, usage, storage and management; (2) collecting the medication standards and indicators; (3) designing a problem oriented checklist, including 85 questions; (4) verifying the validity and reliability of designed checklist by Delphi method and conducting a pilot study. The Cronbach's alpha co efficient were good (more than0.7); (5) to perform of pretest; (6) teaching and introducing of 10 valid evidences to answer the checklist questions in three day workshop to 41 medical interns; (7) after the workshop, students applied the mentioned checklist for assessment of drug safety status on 151 hospitalized patients with the aim of learning during assessment; (8) monitoring of patient’s medication safety status by the interns and self -learning simultaneously; and finally (9) we used Student self-assessment of medication safety education goals, before and after self-training with our checklists.Results:
A standard checklist with dual functions (self-learning during assessment) was developed. Difference between pre-test and post test scores was statistical significant (P ≤ 0.001) and 92% of participants were satisfied with this type of training.Conclusions:
We recommend our designed checklist to all clinical educators who are engaged in medication safety domain.Keywords
Medication Errors Medication Safety Adverse Drug Events Rational Drug Administration and Use
1. Background
1.1. Why Medication Safety?
Every year, nearly 98,000 people die in US hospitals from preventable medical errors, and these mistakes cost $30 billion and increased health expenditures (1). As well as, in the United States, every year, approximately 70,000 hospitalized children, experience at least one adverse event, which 60% of them may be preventable (2). Researchers have estimated that, between 9250 to 23,750 deaths related to adverse drug events (ADEs) have been prevented only in the year 2000 (3). Irrational administration and use of the drugs, increase the side effects of drugs, drug interactions, the development of antibiotic-resistant organisms (4) and increased mortality rates. Therefore, “patient safety”, specially “medication safety” is a very important topic which should be taught at the different clinical medical sciences in universities. Schools of medical sciences (medical, dental, nursing, etc.) are addressing patient safety subject through their curriculum modification. As well as, the Accreditation Council for Pharmacy Education (ACPE) strongly encourages adding the patient safety issue into the pharmacy curricula. The WHO has also recently developed a helpful patient safety curriculum for medical sciences students. In Iran, it has also been incorporated in various courses in undergraduate curriculums (2, 5, 6). The Patient safety course, are included as an elective course in medical student’s curriculum in Iran (5). But, most students do not choose it, because the attitude of medical students about health related issues more focus on remedial problems (curative issues), so, there is no much tendency to engage to community health issues by them. Therefore, due to the importance of the subject, the designed tool is not only applicable for monitoring and supervision, but also it can be used for self-directed landing in most clinical settings. It also helps to integrate basic sciences into clinical one.
Self-directed learning (SDL) is a learner centered approach (7) which it’s special features are as follows: a learning method based on learner needs; formulating learning goals by the learner; identifying human and material sources by the learner him/her- self; evaluating learning outcomes by him/her (8). It is necessary to mention that, currently, there are no any clinical pharmacologists in clinical departments of Azad university hospitals, so the use of SDL method might be a good way to train medical students. So far, a checklist has been used as an evaluation tool and it is less used as an educational tool. A checklist can have multiple applications. For example, it can be applying as a guide to doing a job (e.g. in aviation) (7), to perform a procedure (e.g. WHO surgical checklist) (8), to evaluate professional tasks, to qualification and promoting of processes like patient safety checklist (checklist is a common tool for preventing human errors) (9, 10), it is a tool for learning outcomes assessment, it use as an instrument for self- care and self – regulation (11), it is a tool for a comprehensive look of activities, standardization of activities, and it is a tool for decreasing critical task omissions (8), it is as a guide to transparent division of the tasks, to increase accountability, as well as, to increase the cognitive load (12) and also, it may apply to transfer of knowledge and experiences.
2. Objectives
The main goal in this study was to design and introduce a standard checklist that medical interns to be able to apply it to assess the medication safety status in clinical settings and learn the facts related to this issue simultaneously
3. Methods
The research steps were as follow: Provide a list of possible problems by Ishikawa diagram for collecting problems in six domains including: demographic facilitators and risk factors, prescribing, transcribing, usage, storage and management. (Ishikawa diagram or fishbone technique is a method for listing problems with brain storming and rout cause analysis of problems) (13). Then collecting of drug safety standards, with emphasis on WHO indicators.
Designing a dual function checklist (for assessment of medication safety and self-directed learning simultaneously) including 85 questions. The main format of the questionnaire was a “checklist” (an objective closed questionnaire) with dual educational and supervisory functions which designed as a tool for monitoring of drug events in hospitals and learn the facts simultaneously. The questions of checklist were classified in six categories including: demographic information of the patients, risk factors and facilitators (32 items), prescribing related questions (18 items), transcribing related questions (status of medical orders implementation by nurses) (3 items), rational medication use (RMU) (9 items), drugs reserving and storing indicators (17 items) and drug management indices (6 items) (14, 15).
Verifying the validity and reliability of designed checklist by Delphi method and conducting a pilot study. To confirm the content and face validity of the questionnaire, we inquired the opinions of 15 different experts included: seven clinical specialists, three social & preventive medicine specialists, three pharmacists, one Ph.D. of social determinants of health (SDH) and one nursing MSc (as patient safety executive director in hospital). As well as, to confirm of reliability of the checklist, the questioner was piloted by 41 medical interns who first had a three days designed theoretical and workout training course, then, after the necessary coordination and division of labor, they referred to the different clinical wards of the hospitals and completed the questionnaire for 151 hospitalized patients. Cronbach's alpha and Guttman split half and Spearman-Brown methods were used to measure reliability. The Cronbach's alpha coefficients for main studied domain (medication administration, usage, storage and management) were good (0.788, 0.712, 0.714 and 0.742, respectively). Split- half reliability coefficients for total scale was r = 606. Next step is to perform of pretest.
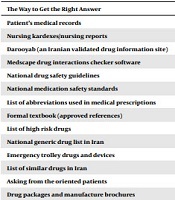
Teaching and introducing of 10 valid evidences to answer the checklist questions in three-day workshop to 41 medical interns (Table 1)
Documents which Introduced and Taught in Workshop
| The Way to Get the Right Answer | References |
|---|---|
| Patient’s medical records | - |
| Nursing kardexes/nursing reports | - |
| Darooyab (an Iranian validated drug information site) | (15) |
| Medscape drug interactions checker software | (16) |
| National drug safety guidelines | (17) |
| National medication safety standards | (17) |
| List of abbreviations used in medical prescriptions | (18) |
| Formal textbook (approved references) | (19, 20) |
| List of high risk drugs | (16) |
| National generic drug list in Iran | (21, 22) |
| Emergency trolley drugs and devices | (23) |
| List of similar drugs in Iran | (16) |
| Asking from the oriented patients | - |
| Drug packages and manufacture brochures | - |
Use of designed tool for 151 hospitalized patients by the interns (assess and learn simultaneously) under supervision of faculties.
Monitoring of patient’s medication safety status by the interns and self -learning simultaneously; and finally, we used, student self-assessment of medication safety education goals, before and after self-training with our checklists
Medical interns were chosen as the learners because they have relatively good information about the drugs and they are allowed to enter various medical units and they have access to patient’s profiles and nursing kardexes. As well as, they are able to communicate with managers, doctors, nurses, technicians and patients.
4. Results
We have developed a checklist with dual function of "evaluation" and "training" of medication safety in clinical wards. Details of the questionnaire are discussed below. This checklist has been used for more than one year with the approval of the department as a component of social medical education in community & preventive medicine department of Islamic Azad University, Tehran, Iran. This questionnaire of drug safety in the hospital consists of five separate parts, that each of which can be used separately. Assessors can be physicians, nurses responsible for patient safety plans in the hospital (with the purpose of evaluation) or the medical interns and pharmacotherapy residents (with the purpose of evaluation and self-education) as well as researchers. Part 1, demographic information and factors affecting patient safety issues (refer to the patient’s file); Part 2, evaluation of prescribing errors (refer to the patient’s file); Part 3, evaluation of transcribing errors (refer to nursing Kardexes and nursing reports); Part 4, questions related to medication preserving and storage (16) (refer to shelf or drug and treatment room); Part 5, questions related to medication management in the hospital. The change in attitude, knowledge and experiences of students was evaluated with a rating scale on 41 participants (medical interns) which the results were shown in Table 2.
| Question | Yes | No | If Yes, How Much? | |||
|---|---|---|---|---|---|---|
| Very Much | Somewhat | Trace | Missing | |||
| My scattered information on drug safety was aggregated and categorized in my mind. | 37 (94.9) | 2 (5.1) | 27 (69.2) | 10 (25.6) | - | - |
| My attention was drawn to the points that, so far I had not thought much about them. | 35 (89.8) | 4 (10.2) | 30 (77) | 5 (12.8) | - | - |
| My attitude to necessity of identifying and managing the medication errors changed. | 33 (84.6) | 5 (12.8) | 27 (69.2) | 6 (15.4) | - | 1 (2.6) |
| I got some capabilities to identify medication errors and how to manage them. | 34 (87.2) | 5 (12.8) | 23 (59) | 7 (18) | 3 (7.6) | 1 (2.6) |
| Systemically I got acquainted with the potential hazards threatens patients in the hospital in drug safety domain. | 37 (94.9) | 2 (5.1) | 29 (74.3) | 6 (15.4) | 1 (2.6) | 1 (2.6) |
| I got acquainted with RCA (root cause analysis) techniques. | 35 (89.8) | 4 (10.2) | 20 (51.3) | 14 (35.9) | - | 1 (2.6) |
| I got acquainted with the features of a “checklist” and how to design it. | 39 (100) | - | 28 (71.8) | 9 (23) | 1 (2.6) | 1 (2.6) |
| I got acquainted with the ways to prevent the medication errors. | 38 (97.4) | 1 (2.6) | 23 (59) | 10 (25.6) | 1 (2.6) | 4 (10.2) |
| I applied the theoretical contents that I had learned at the workshop, in confronting with the current facts in the hospitals. | 34 (87.2) | 5 (12.8) | 22 (56.5) | 9 (23) | 1 (2.6) | 2 (5.1) |
| In my mind, I accepted the issue of patient safety especially medication safety as an important professional duty. | 36 (92.3) | 3 (7.7) | 30 (76.9) | 4 (10.2) | 1 (2.6) | 1 (2.6) |
| Overly, I was satisfied with this type of training. | 37 (94.9) | 2 (5.1) | 32 (82) | 4 (10.3) | - | 1 (2.6) |
Pre-test and post test scores were compared and the results of the scores obtained are presented in Table 3.
Comparison of Pretest and Posttest Scores
| Question | Pretest Scores (n = 19) | Posttest Scores (n = 22) | P Value |
|---|---|---|---|
| Some drug name with sound similarity | 6.8 | 12.2 | ≤ 0.001 |
| List of high risk drugs | 6.8 | 15.4 | ≤ 0.001 |
| Pharmaceutical prescription abbreviations | 10 | 9.5 | 1.00 |
| Essential drugs of emergency trolley | 12.1 | 13.1 | 0.549 |
| Contents of the second floor of emergency trolley | 5.2 | 20 | ≤ 0.001 |
| Contents of the third floor of emergency trolley | 4.2 | 14.5 | ≤ 0.001 |
| Ability to use a proven software for drug interactions assessment | 8.4 | 18.2 | ≤ 0.001 |
| Ability to use fish bone technic for medication errors root cause analysis | 0 | 15.4 | ≤ 0.001 |
Table 4 shows the results of interns' self-assessment before and after self-training with our checklist.
Student Self-assessment of Medication Safety Education Goals, Before and After Self-training with Our Checklists
| Questions a | N | Correlation | Significancy |
|---|---|---|---|
| Q1B & Q1A | 21 | 0.557 | 0.009 |
| Q2B & Q2A | 21 | 0.703 | 0.000 |
| Q3B & Q3A | 21 | -0.114 | 0.621 |
| Q4B & Q4A | 21 | 0.248 | 0.278 |
| Q5B & Q5A | 21 | 0.320 | 0.158 |
| Q6B & Q6A | 21 | 0.572 | 0.007 |
| Q7B & Q7A | 21 | 0.385 | 0.085 |
| Q8B & Q8A | 21 | 0.469 | 0.032 |
| Q9B & Q9A | 21 | 0.759 | 0.001 |
| Q10B & Q10A | 21 | 0.773 | 0.001 |
| Q11B & Q11A | 21 | 0.592 | 0.005 |
| Q12B & Q12A | 21 | 0.816 | 0.001 |
| Q13B & Q13A | 21 | 0.737 | 0.001 |
| Q14B & Q14A | 21 | 0.316 | 0.162 |
| Q15B & Q15A | 21 | 0.170 | 0.460 |
| Q16B & Q16A | 21 | 0.438 | 0.047 |
| Q17B & Q17A | 21 | 0.694 | 0.001 |
| Q18B & Q18A | 21 | 0.589 | 0.005 |
| Q19B & Q19A | 21 | 0.567 | 0.007 |
| Q20B & Q20A | 21 | 0.745 | 0.001 |
| Q21B & Q21A | 21 | 0.674 | 0.001 |
| Q22B & Q22A | 21 | 0.457 | 0.037 |
| Q23B & Q23A | 21 | 0.428 | 0.053 |
| Q24B & Q24A | 21 | 0.546 | 0.010 |
| Q25B & Q25A | 21 | 0.354 | 0.115 |
5. Discussion
Prescribing, transcribing, applying, reserve & storing and managing the drugs are important activities that medical students must be familiar with them. In this study, we have developed a standard checklist for evaluation of medication safety and we have introduced it as a tool for monitoring the medication safety and learning different situations simultaneously.
Using a checklist makes us aware of the problems that are out of our sight. A completely transparent and standard checklist can play an important role in documenting of experiences. Checklists are commonly suggested tools to reduce errors (12); and also a checklist may be given to students to use it to accomplish and complete the steps of a procedure (16).
Kok et al., with using a chest radiograph checklist have shown that, a checklist can help medical students to detect more abnormalities on the chest radiographs (11). As well as, another study showed that the checklists reduce diagnostic errors (12).
The attitude of medical students about health related issues more focus on remedial problems (curative issues), so there is no much tendency to engage to community health issues by them. Therefore, at the beginning of the course, some students did not agree with the fact that attention to patient safety concept is a part of their professional tasks, while this issue (medication safety) has been considered in their new curriculum.
Despite the initial opposition, most students gradually became aware to importance of the subject, so that, the final evaluation of the short educational course showed that 94.9% of students were satisfied with this type of training. As well as, in our study, 84.6% of the participants were agreed with changing their attitudes toward education about the necessity to pay attention to the patient safety and medication error issues. Almaramhy et al. have shown that, only 60.7% of medical students were agree with the importance of the patient safety subject (17). This is while in our study, 92.3% of students accepted the issue of patient safety as a professional duty in their mind.
The changes in relation to 6 out of 8 questions in the pretest and posttest scores, as well as, the total score were statistical significantly different. Two topics that had no statistical significant changes were drug abbreviations and list of emergency trolley drugs that we should work on them more.
The medication error checklist was validated by experts and the reliability of the checklist in a pilot study was approved (Cronbach's alpha coefficient were above 0.7) (18).
In calculating reliability of “medication administration error” questionnaire in Taheri et al. study in 2013, Cronbach's alpha was equal to 0.712 for different types of non-injection medication errors and 0.841 for different types of injection medication errors (19).
As well as, in Vizeshfar et al. research in 2015, pharmacological errors questionnaire was used and the validity of each part was specified with content validity and reliability method was affirmed by Cronbach’s alpha coefficient (alpha = 80) (20).
5.1. Study Limitations
Although the questionnaire seems a bit long and time consuming, but in certain circumstances, the questionnaire can be divided into four complete distinct parts including: prescribing, transcribing and usage, storage and managing the drugs.
5.2. Conclusion
The results of student self-assessment, demonstrate the usefulness of our checklists in student self-training of medication safety. Therefore, we recommend using this dual function checklist (self- directed learning via evaluation of medication safety status) to all clinical educators who are engaged in this domain (clinicians), especially when there are no clinical pharmacologists in clinical settings.
5.3. Achievements
Design a dual functions checklist; attracting students to a critical professional task; assist in the implementation of patient safety monitoring programs in the hospital.
Acknowledgements
References
-
1.
Kiersma ME, Plake KS, Darbishire PL. Patient safety instruction in US health professions education. Am J Pharm Educ. 2011;75(8):162. [PubMed ID: 22102752]. [PubMed Central ID: PMC3220343]. https://doi.org/10.5688/ajpe758162.
-
2.
Woods D, Thomas E, Holl J, Altman S, Brennan T. Adverse events and preventable adverse events in children. Pediatrics. 2005;115(1):155-60. [PubMed ID: 15629994]. https://doi.org/10.1542/peds.2004-0410.
-
3.
Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian adverse events study: The incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678-86. [PubMed ID: 15159366]. [PubMed Central ID: PMC408508]. https://doi.org/10.1503/cmaj.1040498.
-
4.
Yewale VN, Dharmapalan D. Promoting appropriate use of drugs in children. Int J Pediatr. 2012;2012:906570. [PubMed ID: 22645620]. [PubMed Central ID: PMC3356911]. https://doi.org/10.1155/2012/906570.
-
5.
Supreme Council for Medical Science Planning. General medical doctors curriculum. Tehran, Iran: Islamic Republic of Iran, Ministry of Health and Medical Education, Deputy Ministry for Education; 2017.
-
6.
Kamran R, Bari A, Khan RA, Al-Eraky M. Patient safety awareness among undergraduate medical students in Pakistani medical school. Pak J Med Sci. 2018;34(2):305-9. [PubMed ID: 29805398]. [PubMed Central ID: PMC5954369]. https://doi.org/10.12669/pjms.342.14563.
-
7.
Petrik EW, Ho D, Elahi M, Ball TR, Hofkamp MP, Wehbe-Janek H, et al. Checklist usage decreases critical task omissions when training residents to separate from simulated cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2014;28(6):1484-9. [PubMed ID: 25277642]. https://doi.org/10.1053/j.jvca.2014.05.011.
-
8.
Mayer EK, Sevdalis N, Rout S, Caris J, Russ S, Mansell J, et al. Surgical checklist implementation project: The impact of variable WHO checklist compliance on risk-adjusted clinical outcomes after national implementation: A longitudinal study. Ann Surg. 2016;263(1):58-63. [PubMed ID: 25775063]. https://doi.org/10.1097/SLA.0000000000001185.
-
9.
Ambulkar R, Ranganathan P, Salunke K, Savarkar S. The World Health Organization surgical safety checklist: An audit of quality of implementation at a tertiary care high volume cancer institution. J Anaesthesiol Clin Pharmacol. 2018;34(3):392-8. [PubMed ID: 30386026]. [PubMed Central ID: PMC6194824]. https://doi.org/10.4103/joacp.JOACP_328_17.
-
10.
Staender S, Smith A. Enhancing the quality and safety of the perioperative patient. Curr Opin Anaesthesiol. 2017;30(6):730-5. [PubMed ID: 28938300]. https://doi.org/10.1097/ACO.0000000000000517.
-
11.
Kok EM, Abed A, Robben SGF. Does the use of a checklist help medical students in the detection of abnormalities on a chest radiograph? J Digit Imaging. 2017;30(6):726-31. [PubMed ID: 28560508]. [PubMed Central ID: PMC5681473]. https://doi.org/10.1007/s10278-017-9979-0.
-
12.
Nabilou B, Feizi A, Seyedin H. Patient safety in medical education: Students' perceptions, knowledge and attitudes. PLoS One. 2015;10(8). e0135610. [PubMed ID: 26322897]. [PubMed Central ID: PMC4554725]. https://doi.org/10.1371/journal.pone.0135610.
-
13.
Exir Danesh Asia Pharmacoutical Co. [Darooyab]. Tehran, Iran: Exir Danesh Asia Pharmacoutical Co; 2021. Persian. Available from: https://www.darooyab.ir/.
-
14.
Mohanty M, Lawal OD, Skeer M, Lanier R, Erpelding N, Katz N. Medication errors involving intravenous patient-controlled analgesia: Results from the 2005-2015 MEDMARX database. Ther Adv Drug Saf. 2018;9(8):389-404. [PubMed ID: 30364852]. [PubMed Central ID: PMC6199682]. https://doi.org/10.1177/2042098618773013.
-
15.
Ministry of Health and Medical Education in Iran. [National Guidelines]. Tehran, Iran: Vice-Chancellor in Treatment Affairs, Shahid Beheshti of Medical Sciences; 2021. Persian. Available from: http://treatment.sbmu.ac.ir/index.jsp?pageid=49029&p=1.
-
16.
Institute for Safe Medication Practices; National Medication Errors Reporting Program (ISMP MERP). List of high risk drugs. Tehran, Iran: Tehran University of Medical Sciences, Deputy of Food and Drug Affairs; 2014. Available from: http://fdo.tums.ac.ir/uploads/HighAlert.pdf.
-
17.
Almaramhy H, Al-Shobaili H, El-Hadary K, Dandash K. Knowledge and attitude towards patient safety among a group of undergraduate medical students in Saudi Arabia. Int J Health Sci. 2011;5(1):59-67. [PubMed ID: 22489231]. [PubMed Central ID: PMC3312770].
-
18.
Gliem JA, Gliem RR. Calculating, interpreting, and reporting Cronbach’s alpha reliability coefficient for Likert-type scales. Midwest Research to Practice Conference in Adult, Continuing, and Community Education. USA. Indiana University; 2003. p. 82-8.
-
19.
Taheri E, Nourian M, Rasouli M, Kavousi A. The study of type and amount of medication errors in neonatal intensive care units and neonatal units. Iran J Crit Care Nurs. 2013;6(1):21-8.
-
20.
Vizeshfar F, Rivaz M, Montaseri Z, Montaseri H. Assessment of the rate and etiology of pharmacological errors by nurses of two major teaching hospitals in Shiraz. Trends Pharm Sci. 2015;1(2):87-96.
-
21.
Darooyab. [List of Generic drug names]. 2020. Persian. Available from: http://www.darooyab.ir/Generic.
-
22.
Hogerzeil HV, Policy A. Essential medicines and health products information portal a World Health Organization resource. WHO Drug Information. 2002;16(3).
-
23.
Urmia University of Medical Sciences. [Emergency trolley information]. 2009. Persian. Available from: https://shahindezh.umsu.ac.ir/uploads/%D8%AA%D8%B1%D8%A7%D9%84%DB%8C_12369.pdf.