Abstract
Objectives:
The main objective of this study was to understand the nurses' attitudes in implementation and adoption of CPOE system through Rogers’ innovation diffusion theory.Methods:
This study was cross-sectional and performed in four months (from March to June, 2017). In order to understand the acceptance of the CPOE investigated level of nursing staff’s computer literacy. The major factors influencing the nursing staff’s acceptance and use of the CPOE system were examined through Rogers’ innovation diffusion theory. Data were collected using a researcher.Results:
Majority of the nursing staff adopt this innovation. The level of nursing staff’s computer literacy was high (71.32%). Highly educated nursing staff were more likely to accept computer work. The acceptance or rejection of the use of a computer is related to experiencing the HIS system in nursing. Our finding showed that the received relative advantages, compatibility, the complexity of the system were 66.29%, 71.94% and 40.36% for the nursing staff.Conclusions:
Majority of the nursing staff had a good degree of computer literacy. The analysis of the finding shows that CPOE systems improve the quality and safety of healthcare. CPOE increases the security and quality of health care and reduces errors.Keywords
Electronic Medical Record Computerized Provider Order Entry Health Personnel Attitude Patient Safety Innovation Diffusion Feasibility Study Nursing Staff
1. Background
Computerized provider order entry (CPOE) systems are electronic versions that end-users can registration orders into a computer application rather than use paper records (1) also ensure standardized, legible, and complete orders (2-4). Technologically, CPOE is discussed nearly half a century (5). Until 2009, CPOE was available in less than 20% of US hospitals (6-8). In 2012, majority of hospitals use CPOE for variety tests (9). While the results of searching show that the only one public hospital in Iran uses CPOE just for prescribing (10).
One of the main aspects that can determine the success of implementation of CPOE is providers’ satisfaction. We know that providers have a crucial role in CPOE development. They could affect the success of the implementation of CPOE (11). Several studies examined the impact of CPOE implementation on providers’ performance (12-14). In 2003, almost all of the providers were dissatisfied with newly installed CPOE (15). Most studies show that providers’ resistance is a great obstacle to implement CPOE (16, 17) while other studies reported that providers have a willingness to use CPOE and believed with CPOE usability, efficiency, workflow, and patient safety (18, 19).
One of the most popular adoption models for understanding how CPOE innovation between providers is the diffusion of innovations theory and understanding how CPOE innovation accepts between providers (20-22). To increase the scientific value and generalizability this research, Rogers’ innovation diffusion theory was used to analyze the impact of factors on the nursing staff attitudes toward the acceptance or rejection of the CPOE. A CPOE technology’s relative advantage, compatibility, trialability, and observability generally lead to a faster rate of adoption, while increased complexity leads to a lower rate of adoption.
2. Objectives
The views and attitudes of nursing staff are essential on the usefulness and ease of use of a CPOE. Since nursing staff are one of the main users of CPOE, in this study, we set out to examine factors that may influence CPOE adoption among nurses in a large healthcare organization. The diffusion of innovation theory was used to understand nurses’ attitudes and thoughts about implementation and use of the CPOE system.
3. Methods
This cross-sectional study was conducted in Urmia City, North West of Iran, in 2017. Four teaching hospitals were in this region: 450-bed Emam Khomeini, 205-bed Motahari, 153-bed Seyedoshohada and 218-bed Taleghani. All nurses working in hospitals were included in data collection. The major factors influencing nursing staff’s acceptance and use of the CPOE system were examined through Rogers’ innovation diffusion theory.
3.1. Research Instrument
We used the multi-section questionnaire of Rahimi et al. that has been tested for reliability and validity in a previous study (23). The language of the questionnaire was Persian. The responses were in Likert scale format (strongly agree, agree, neutral, disagree, strongly disagree). The questionnaire was included: nursing staff' demographic information (12 questions), survey the level of computer literacy of the nursing staff (7 questions), survey the level of CPOE literacy of the nursing staff (4 questions), survey the attitude of nursing staff about the effectiveness of CPOE (21 questions (relative advantages (12 questions) and compatibility (9 questions))), survey the attitude of nursing staff of the complexity arising from the implementation of CPOE (8 questions), and survey the attitude of nursing staff regarding the technology necessary for the implementation of CPOE (8 questions). Statistical analysis was performed with SPSS Version 16.0
4. Results
4.1. Demographic Variables
Table 1 describes the research population. A total of 273 questionnaires were distributed among the nursing staff. The results showed that 177 nursing staff (64.84%) completed the questionnaire. Approximately, the number of female participants (n = 94, 53.1%) was higher than the number of male participants (n = 83, 46.9%), and most of them were young with an average age of 34.97 ± 5.85 years.
Characteristics of the Nursing Staff in the Final Study Population
| Characteristics | No. (%) |
|---|---|
| Sex | |
| Men | 83 (46.9) |
| Women | 94 (53.1) |
| Age groups (y) | |
| 20 - 29 | 63 (35.6) |
| 30 - 39 | 54 (30.5) |
| 40 - 49 | 46 (26) |
| 50 - 59 | 14 (7.9) |
4.2. The Level of Computer Literacy
The questions and responses are listed in Table 2. Generally, the level of nursing staff’s computer literacy was high (71.32%). Respondents indicated that a large number of nursing staff download scientific contents from the internet (n = 171, use email (n = 89), also to work on the PC while at the workplace (n = 140).
Distribution of the Nursing Staff Responses About the Level of Computer Literacy
| Questions | Strongly Disagree | Disagree | No Comment | Agree | Strongly Agree |
|---|---|---|---|---|---|
| Office skills | 5.6 | 9.7 | 60.7 | 20.2 | 3.7 |
| Work on the PC at workplace | 8.6 | 13.9 | 31.5 | 37.5 | 8.6 |
| Ability to install the software | 8.6 | 18 | 46.8 | 21.7 | 4.9 |
| Use Email | 38.6 | 38 | 0 | 102 | 24 |
| Download book and scientific contents from the internet | 4.1 | 0.4 | 47.9 | 34.8 | 12.7 |
| Advantages of using computers in the healthcare | 4.1 | 18 | 55.8 | 18 | 4.1 |
| Computer ability to facilitate daily tasks | 3.7 | 17.2 | 39 | 27 | 13.1 |
4.3. Nursing Staff Satisfaction
The collected data showed that just 26% of the nursing staff was aware of the CPOE system. Also we found that the compatibility, relative advantages, and complexity of the CPOE were 71.94%, 66.29% and 40.36%.
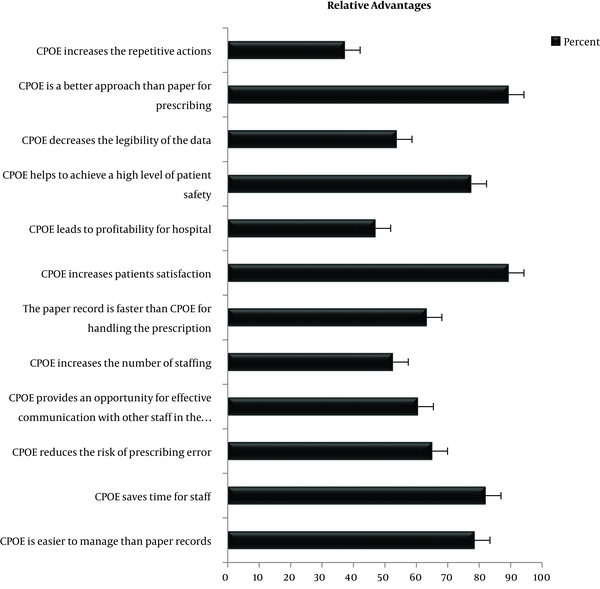
4.3.1. Level of the View of Nursing Staff About the Relative Advantages of CPOE
In the present study, the received relative advantages of the CPOE was high (66.29%). In advantages section from Figure 1, it can be seen that a lower percentage of the nursing staff agreed that the CPOE is faster to handle than the paper-based system (36.8%) whereas the vast majority respondents (78.5%) agreed that system is easier to manage than paper records and an up percentage of the nursing staff (82%) agreed that the system will save time for staff.
Distribution of the respondents’ agreement with statements about relative advantages of the CPOE system
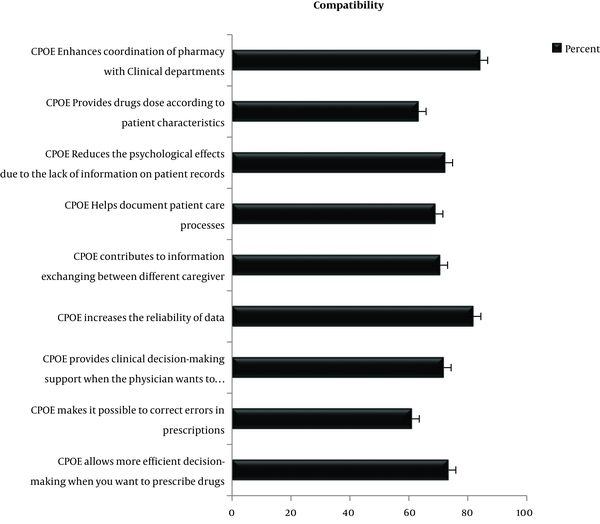
4.3.2. Level of the View of the Nursing Staff About the Compatibility of CPOE
In this study, we found that the compatibility of the CPOE was 71.94%. In the compatibility section from Figure 2, it can be seen that the CPOE will be more effective than the paper-based system. For example, when physicians prescribe drugs, the system can be more effective (73.4%). Findings show that 72.3% of the nursing staff agreed that the CPOE Reduces the missing of information on patient records.
Distribution of respondents’ agreement with statements about the compatibility of the CPOE system
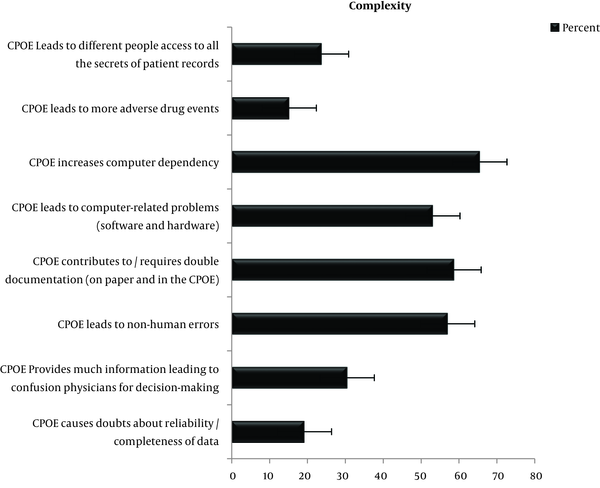
4.3.3. The Level of the View of the Nursing Staff About the Complexity of CPOE
In this study, we found that the complexity of the CPOE was 40.36%. In complexity section from Figure 3, it can be seen that a minority of the nursing staff (19.2%) stated that the CPOE system will increase doubts about completeness and reliability of data. In addition, 53.1% of the nursing staff stated that the CPOE system can lead to computer problems (software and hardware).
Distribution of respondents’ agreement with statements about the complexity of the CPOE system
4.4. Comparison of the View of the Nursing Staff About the Innovation of CPOE with Gender, Age, Educational Level, Experience of Using the HIS System and Computer Literacy
CPOE implementation in male nursing staff was acceptable. The findings showed that the relative advantages, compatibility and complexity among male and females nursing staff were almost equal (gender section from Table 3). Their viewpoint about the relative advantages, compatibility was high and complexity was low (P > 0.05).
Relative Advantages, Compatibility and Complexity Scores of Nurses in a CPOE System Based on Their Demographic Information a
| Attributions of the Diffusion of Innovation Theory | Relative Advantages | Compatibility | Complexity |
|---|---|---|---|
| Gender | |||
| Men | 60.84 ± 6.96 | 61.06 ± 7.01 | 36.01 ± 4.88 |
| Women | 59.96 ± 5.94 | 67.29 ± 5.88 | 34.57 ± 4.77 |
| Age groups (y) | |||
| 22 - 32 | 40.18 ± 6.28 | 40.3 ± 6.3 | 21.84 ± 4.89 |
| 33 - 42 | 34.1 ± 6.53 | 30.42 ± 6.7 | 25.83 ± 4.72 |
| > 43 | 35.72 ± 6.77 | 26.53 ± 6.46 | 20.55 ± 4.85 |
| Degree of education | |||
| Associate’s degree | 30.5 ± 5.52 | 20.42 ± 5.41 | 26.5 ± 3.6 |
| Bachelor’s degree | 30.08 ± 6.37 | 20.57 ± 6.32 | 25.27 ± 5.04 |
| Master’s degree | 31.1 ± 7.06 | 20.75 ± 7.32 | 26.32 ± 4.75 |
| Phd’s degree | 31.86 ± 9.46 | 23.14 ± 9.79 | 28.71 ± 5.09 |
| Experience with the HIS system (mo) | |||
| NO | 30.06 ± 5.93 | 20.39 ± 5.69 | 25.48 ± 4.83 |
| < 1 | 28.78 ± 3.96 | 19.13 ± 2.48 | 25 ± 3.42 |
| 2 - 6 | 31.92 ± 8.35 | 21.77 ± 8.95 | 28.03 ± 4.66 |
| 6 - 12 | 31.95 ± 8.63 | 22.45 ± 9.3 | 25.23 ± 6.32 |
| > 12 | 30.31 ± 5.74 | 20.58 ± 5.67 | 25.77 ± 4.64 |
Older nursing staff also accepted CPOE implementation hardly (age section from Table 3). Since young nursing staff use technology more often, then they also welcome CPOE. However, older nurses were also more likely to agree that relative advantages of CPOE are high (P > 0.05).
The findings showed that the degree of education has the same effect on the recognition of Relative advantages, Compatibility and Complexity of the CPOE system (degree of education section from Table 3). Although nurses with a baccalaureate degree and more had better computer literacy, the educational level did not affect CPOE acceptance (P > 0.05).
5. Discussion
All of the organizations and individuals are interested to change (24). The present study has demonstrated that understanding the nursing staff’s computer literacy and their attitude and satisfaction can be effective in accepting and the implementation of a CPOE system. Although prescribing is done by the physicians, our study examines nursing staff satisfaction with CPOE. The results of this study show that to how extent nursing staff agree with the use of computers in the workplace and the implementation of CPOE.
Generally, the level of nursing staff’s computer literacy was high. Approximately, half of the nursing staff reported that they use computers in the workplace. Our results demonstrate the associations between nursing staff’s view computers with age, educational level, and experience with the HIS system. Our study found that age was small in the nursing staff’s computer literacy. Similarly, as with other studies reported this to be very small or nonexistent (25, 26).
Since the level of nursing staff’s computer literacy was high, it is expected that they would easily accept CPOE. The findings indicated that the educational level did not affect CPOE acceptance. Likewise, Khajouei’s study revealed that there was no significant relationship between nurses’ satisfaction and educational level (27). However, evidence shows that gradual acquisition of the skills through training could effectively increase users’ satisfaction (28). Young nursing staff accepted CPOE implementation more easily.
Often, studies have shown that CPOE provision of just-in-time feedback to physicians when they want to prescribe drugs (29-31). In our study, most of the nursing staff believe that CPOE makes it possible to correct errors at the moment of prescription. Correct errors at the moment of prescription increase patient satisfaction that one finding in our study demonstrated that approximately all nursing staff thought CPOE increases patient satisfaction.
Another important finding of this study was that approximately half of the nursing staff agreed about increasing prescription legibility. Also study Foster and Antonelli on CPOE showed the same opinion (32). They believe that the advantages of CPOE include order legibility, improved response time, reduction in adverse drug reactions, and improved patient outcomes.
This study has several limitations. First, this study was limited to the perception of innovation attributes such as relative advantage, compatibility and complexity and other studies could be carried out to include other factors such as trialability and observability. Second, the number of the participating nursing staff was also low.
Despite these limitations, this study has identified a factor that could have an impact on the users’ high satisfaction. Results of this study emphasize the importance of training programs that aim at improving computer literacy among nursing staff and ultimately would increase their levels of satisfaction with the system and increase productivity with ease.
Acknowledgements
References
-
1.
Metzger J, Turisco F. Computerized physician order entry: a look at the vendor marketplace and getting started. Washington, DC: Leapfrog Group; 2001.
-
2.
Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003;163(12):1409-16. [PubMed ID: 12824090]. https://doi.org/10.1001/archinte.163.12.1409.
-
3.
Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160(18):2741-7. [PubMed ID: 11025783]. https://doi.org/10.1001/archinte.160.18.2741.
-
4.
Marfo; Garcia; Khalique; Berger; Lu; Khalique. Evaluation of medication errors via a computerized physician order entry system in an inpatient renal transplant unit. Transpl Res Risk Manag. 2011;3:91-6. https://doi.org/10.2147/trrm.s17819.
-
5.
Sittig DF, Stead WW. Computer-based physician order entry: the state of the art. J Am Med Inform Assoc. 1994;1(2):108-23. [PubMed ID: 7719793]. [PubMed Central ID: PMC116190]. https://doi.org/10.1136/jamia.1994.95236142.
-
6.
Aarts J, Koppel R. Implementation of computerized physician order entry in seven countries. Health Aff (Millwood). 2009;28(2):404-14. [PubMed ID: 19275996]. https://doi.org/10.1377/hlthaff.28.2.404.
-
7.
Furukawa MF, Raghu TS, Spaulding TJ, Vinze A. Adoption of health information technology for medication safety in U.S. Hospitals, 2006. Health Aff (Millwood). 2008;27(3):865-75. [PubMed ID: 18474981]. https://doi.org/10.1377/hlthaff.27.3.865.
-
8.
Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628-38. [PubMed ID: 19321858]. https://doi.org/10.1056/NEJMsa0900592.
-
9.
DesRoches CM, Charles D, Furukawa MF, Joshi MS, Kralovec P, Mostashari F, et al. Adoption of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Aff (Millwood). 2013;32(8):1478-85. [PubMed ID: 23840052]. https://doi.org/10.1377/hlthaff.2013.0308.
-
10.
Khammarnia M, Zand F, Sharifian R, Barati O, Keshtkaran A, Sabetian G, et al. Designing and implementation of computerized provider order entry software on mobile device in Iran. Shiraz E-Med J. 2018;19(Suppl). e66305. https://doi.org/10.5812/semj.66305.
-
11.
Saathoff A. Human factors considerations relevant to CPOE implementations. J Healthc Inf Manag. 2005;19(3):71-8. [PubMed ID: 16045087].
-
12.
Callen J, Braithwaite J, Westbrook J. Differences in doctors' and nurses' assessments of hospital culture and their views about computerised order entry systems. Stud Health Technol Inform. 2008;136:15-20. [PubMed ID: 18487701].
-
13.
Weiner M, Gress T, Thiemann DR, Jenckes M, Reel SL, Mandell SF, et al. Contrasting views of physicians and nurses about an inpatient computer-based provider order-entry system. J Am Med Inform Assoc. 1999;6(3):234-44. [PubMed ID: 10332656]. [PubMed Central ID: PMC61363]. https://doi.org/10.1136/jamia.1999.0060234.
-
14.
Kazemi A, Fors UG, Tofighi S, Tessma M, Ellenius J. Physician order entry or nurse order entry? Comparison of two implementation strategies for a computerized order entry system aimed at reducing dosing medication errors. J Med Internet Res. 2010;12(1). e5. [PubMed ID: 20185400]. [PubMed Central ID: PMC2855204]. https://doi.org/10.2196/jmir.1284.
-
15.
Freudenheim M. Many hospitals resist computerized patient care. New York Times. 2004;6.
-
16.
Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R. Overcoming the barriers to the implementing computerized physician order entry systems in US hospitals: perspectives from senior management. AMIA Annu Symp Proc. 2003:975. [PubMed ID: 14728479]. [PubMed Central ID: PMC1480209].
-
17.
Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R. Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals. Health Aff (Millwood). 2004;23(4):184-90. [PubMed ID: 15318579]. https://doi.org/10.1377/hlthaff.23.4.184.
-
18.
Khajouei R, Wierenga PC, Hasman A, Jaspers MW. Clinicians satisfaction with CPOE ease of use and effect on clinicians' workflow, efficiency and medication safety. Int J Med Inform. 2011;80(5):297-309. [PubMed ID: 21419695]. https://doi.org/10.1016/j.ijmedinf.2011.02.009.
-
19.
Kazemi A, Ellenius J, Tofighi S, Salehi A, Eghbalian F, Fors UG. CPOE in Iran-a viable prospect? Physicians' opinions on using CPOE in an Iranian teaching hospital. Int J Med Inform. 2009;78(3):199-207. [PubMed ID: 18760960]. https://doi.org/10.1016/j.ijmedinf.2008.07.004.
-
20.
Sherry L, Gibson D. The path to teacher leadership in educational technology. Contemporary issues in technology and teacher education. 2002;2(2):178-203.
-
21.
Venkatesh; Morris; Davis; Davis. User acceptance of information technology: Toward a unified view. MIS Quarterly. 2003;27(3):425. https://doi.org/10.2307/30036540.
-
22.
Rogers EM. The diffusion of innovation. 5th ed. New York: Free Press; 2003.
-
23.
Rahimi B, Timpka T, Vimarlund V, Uppugunduri S, Svensson M. Organization-wide adoption of computerized provider order entry systems: a study based on diffusion of innovations theory. BMC Med Inform Decis Mak. 2009;9:52. [PubMed ID: 20043843]. [PubMed Central ID: PMC2809050]. https://doi.org/10.1186/1472-6947-9-52.
-
24.
Lorenzi NM, Riley RT. Managing change: an overview. J Am Med Inform Assoc. 2000;7(2):116-24. [PubMed ID: 10730594]. [PubMed Central ID: PMC61464]. https://doi.org/10.1136/jamia.2000.0070116.
-
25.
Moody LE, Slocumb E, Berg B, Jackson D. Electronic health records documentation in nursing: nurses' perceptions, attitudes, and preferences. Comput Inform Nurs. 2004;22(6):337-44. [PubMed ID: 15602303]. https://doi.org/10.1097/00024665-200411000-00009.
-
26.
Levy S, Williams B. Attitudes to information technology: toys or tools? Nurs Stand. 1999;13(52):1-9. [PubMed ID: 27036369]. https://doi.org/10.7748/ns1999.09.13.52.1.c2675.
-
27.
Khajouei R, Abbasi R. Evaluating nurses' satisfaction with two nursing information systems. Comput Inform Nurs. 2017;35(6):307-14. [PubMed ID: 28060182]. https://doi.org/10.1097/CIN.0000000000000319.
-
28.
Alanazy S. Factors associated with implementation of electronic health records in Saudi Arabia [Thesis/dissertation]. Newark, N.J: University of Medicine and Dentistry of New Jersey; 2006.
-
29.
Kaushal R, Bates DW. Computerized physician order entry (CPOE) with clinical decision support systems (CDSSs). Making health care safer: a critical analysis of patient safety practices. University of California at San Francisco (UCSF)–Stanford University; 2001. 58 p.
-
30.
Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3(6):399-409. [PubMed ID: 8930856]. [PubMed Central ID: PMC116324]. https://doi.org/10.1136/jamia.1996.97084513.
-
31.
Davenport TH, Glaser J. Just-in-time delivery comes to knowledge management. Harv Bus Rev. 2002;80(7):107-11. 126. [PubMed ID: 12140850].
-
32.
Foster RA, Antonelli PJ. Computerized physician-order entry: are we there yet? Otolaryngol Clin North Am. 2002;35(6):1237-43. vii. [PubMed ID: 12687740]. https://doi.org/10.1016/s0030-6665(02)00088-9.