Abstract
Background:
Neonatal jaundice is one of the most common neonatal problems. About 60% of term and 80% of preterm neonates have jaundice.Objectives:
Due to the high prevalence of early neonatal jaundice, which can lead to mothers’ concerns and even hospitalization of neonates, we decided to study the frequency and risk factors of breast feeding jaundice to determine the role of gynecologists and nurses in the development of this type of jaundice.Methods:
This study was a cross-sectional descriptive study. The sampling method was by convenience. Study populations included one hundred terms, exclusively breastfed neonates aged equal or less than seven days with jaundice who were admitted in Golestan and Khanevadeh hospitals Tehran, Iran from July 2019 to January 2020.Results:
The percentage of causes of jaundice in the study population was 65% non-breastfeeding jaundice (29 male, 36 female), including 36% blood group incompatibility, 19% Rh incompatibility and 10% G6PD deficiency. The amount of breast feeding jaundice was 35% (18 male, 17 female). The most significant factors in breastfeeding jaundice were: use of water or sugar water, depressed nipple, mother’s unwillingness to breastfeed; inappropriate breastfeeding technique, and birth weight < 2500 g.Conclusions:
The high prevalence of breastfeeding jaundice indicates that policies of breastfeeding education need to be revised. Breastfeeding education before delivery, attention of gynecologists to breast problems of mothers during pregnancy, professional coordination of nurses and physicians for effective breastfeeding training, and early mothers’ revisit after the initial discharge of neonates can reduce the frequency of breastfeeding jaundice and readmission of neonates.Keywords
Breastfeeding Breast Problem Gynecologist Neonatal Jaundice Risk Factors
1. Background
Neonatal jaundice is one of the most common neonatal problems. About 60% of term and 80% preterm neonates have jaundice (1). Neonatal jaundice is more common in breastfed infants than formula-fed infants (2). Early and adequate breastfeeding is effective in preventing neonatal jaundice. Inadequate breastfeeding is one of the major causes of neonatal jaundice (3, 4).
Usually, hyperbilirubinemia is physiologic and a natural phenomenon in the neonatal period. In most cases, inadequate breastfeeding causes jaundice rather than the direct effect of breast milk itself (5). There are two types of jaundice caused by breastfeeding. The first type (breast feeding jaundice) is due to inadequate calorie intake or breastfeeding. This type of jaundice occurs early and usually within the first week of birth. Neonates with the uridine diphosphate glucuronosyl transferase 1A1 (UGT1A1) gene polymorphism are more susceptible to this jaundice (6). The second type (breast milk jaundice) has a later onset and is due to abnormalities in breast milk (7).
Jaundice caused by inadequate breastfeeding usually occurs 2 - 4 days after birth and dehydration and calorie deficiency are the major causes of this jaundice. Early mother-child counteraction is effective for the prevention of this type of jaundice and interruption of feeding is no longer recommended as a diagnostic procedure (8). The most important causes of inadequate breastfeeding are breast congestion, fissure, mastitis, depressed nipple, maternal fatigue, and inadequate nutrition of the mother. Also, the mother’s unwillingness to breastfeed, receiving serotonin substance reuptake inhibitors (SSRIs) (9), and lack of awareness of mothers about the importance of proper breastfeeding in prevention of neonatal jaundice are important causes of this type of neonatal jaundice that can be remedied by education during pregnancy and after childbirth. These factors decrease the volume of breastfeeding and lead to inadequate intake of calories and fluids, leading to delayed meconium excretion and increased bilirubin reuptake in the enterohepatic cycle (10).
2. Objectives
Due to the high prevalence of early neonatal jaundice, which can lead to mothers’ concerns and even hospitalization of neonates, we decided to study the frequency and risk factors of breast feeding jaundice to determine the role of gynecologists and nurses in the development of this type of jaundice. Despite the extensive training provided during pregnancy and postpartum for proper breastfeeding, this study can show that educational training for mothers is still insufficient and more practical training is needed to increase mothers’ knowledge and awareness in order to prevent this type of jaundice and reduce hospitalization of neonates.
3. Methods
3.1. Design
This study was a cross-sectional descriptive study. The sampling method was by convenience.
3.2. Setting
Study populations included one hundred neonates with jaundice who were admitted in Golestan and Khanevadeh hospitals Tehran, Iran, from July 2019 to January 2020.
3.3. Study Population
Patients were evaluated by a pediatrician and, if they had jaundice, they would be enrolled in the study. Inclusion criteria were early-onset (first week) hyperbilirubinemia, healthy term neonates, exclusively breastfed and age equal or less than seven days, as well as the absence of metabolic disorders in neonates and mothers. Exclusion criteria were delayed onset (second week and later) hyperbilirubinemia, illness, preterm neonate, age more than seven days and neonates with intestinal disorder. Breast feeding jaundice was hyperbilirubinemia in an exclusively breastfed newborn with a weight loss greater than 7%, serum Na ≥ 150 mEq/L, urine specific gravity > 1012, and serum urea ≥ 40 mg/dL without any causes of jaundice (10).
3.4. Main Outcome Measure
Frequency of causes of jaundice, mean of bilirubin on admission and discharge of neonate and risk factors of jaundice in breastfeeding and non-breastfeeding jaundice were defined as the study outcomes.
3.5. Statistical Analyses
Data analyses were performed by SPSS statistical software version 23 (IBM Company, Chicago, USA). For quantitative variables, mean and standard deviation and for qualitative variables, frequency and percentage were used. Chi-square, independent t-test and Fisher’s test were done and P value < 0.05 was considered significant.
3.6. Ethical Consideration
Informed consent was obtained from mothers and name and information of subjects were kept confidential. The ethics committee of AJA University of Medical Sciences approved the research project of this study.
4. Results
In this study, 47% of the neonates were male and 53% female. The proportion of the causes of jaundice in the study population was 65% non-breastfeeding jaundice (NBFJ) (29 male, 36 female) including 36% blood group incompatibility (23% of neonates blood group A, 13% B, and blood group of mothers O), 19% Rh incompatibility (neonate Rh+ and mothers Rh-) and G6PD deficiency 10%. The frequency of breast feeding jaundice (BFJ) was 35% (18 male, 17 female). In the BFJ group, the duration of hospitalization was 1.93± 0.537, and the mean of bilirubin on admission was 14.19 ± 3.053 and at discharge 8.74 ± 1.013 (Table 1).
| Causes of Jaundice | Number | Bilirubin in Admission, mg/dL | Bilirubin at Discharge, mg/dL | Hospitalization, d |
|---|---|---|---|---|
| Breast feeding jaundice | 35 | 14.62 ± 3.053 | 8.74 ± 1.013 | 1.9 ± 0.537 |
| Blood group incompatibly | 36 | 13.62 ± 2.668 | 8.83 ± 1.201 | 2.6 ± 0.54 |
| Rh incompatibly | 19 | 14.70 ± 3.782 | 8.52 ± 1.442 | 3.5 ± 0.73 |
| G6PD | 10 | 13.90 ± 3.273 | 9.22 ± 0.745 | 3.1 ± 0.23 |
In the BFJ group, bilirubin > 20 mg/dL was seen in 3 neonates (8.6%) and in 32 neonates it was < 20 mg/dL (91.4%). In the NBFJ group 14 neonates (21.5%) had bilirubin > 20 mg/dL and 51 neonates (78.5%) had bilirubin < 20 mg/dL. There was a significant difference between high-level bilirubin in BFJ and NBFJ (P < 0.05) (Table 2).
| Bilirubin, mg/dL | Breastfeeding Jaundice | Non-Breastfeeding Jaundice | P Value |
|---|---|---|---|
| > 20 | 3 (8.6) | 14 (21.5) | < 0.05 |
| < 20 | 32 (91.4) | 51 (78.5) | |
| Total | 35 (100) | 65 (100) |
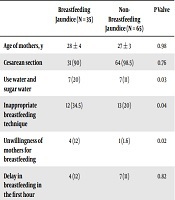
Risk factors affecting the prevalence of jaundice in both groups were shown in Table 3. The most significant factors in breastfeeding jaundice were: use of water or sugar water; depressed nipple; mother’s unwillingness to breastfeed; inappropriate breastfeeding technique and birth weight < 2500 g (P < 0.05) (Table 3).
| Breastfeeding Jaundice (N = 35) | Non-Breastfeeding Jaundice (N = 65) | P Valve | |
|---|---|---|---|
| Age of mothers, y | 28 ± 4 | 27 ± 3 | 0.98 |
| Cesarean section | 31 (90) | 64 (98.5) | 0.76 |
| Use water and sugar water | 7 (20) | 7 (11) | 0.03 |
| Inappropriate breastfeeding technique | 12 (34.5) | 13 (20) | 0.04 |
| Unwillingness of mothers for breastfeeding | 4 (12) | 1 (1.6) | 0.02 |
| Delay in breastfeeding in the first hour | 4 (12) | 7 (11) | 0.82 |
| No breastfeeding education | 4 (12) | 7 (11) | 0.82 |
| Depressed nipple | 11 (31.5) | 3 (5) | 0.001 |
| Fissure | 3 (8.5) | 7 (11) | 0.73 |
| Mastitis | 0(0) | 1 (1.6) | 0.72 |
| Weight < 2500 g | 7 (20) | 5 (7.7) | 0.001 |
| 2500 - 4000 g | 26 (74) | 56 (86) | 0.74 |
| Weight > 4000 g | 2 (6) | 4 (6.2) | 0.81 |
5. Discussion
Due to the high prevalence of early neonatal jaundice, which causes concern for mothers and family, we decided to determine the frequency of breast feeding jaundice and the risk factors contributing to its development. In this study the most important risk factors (about 13 factors, Table 3) that are effective in early jaundice were investigated. In a few studies, all of these factors were studied together. This study showed that breastfeeding jaundice accounted for 35% of neonates hospitalized for jaundice in the first week. Use of water or sugar water, depressed nipple; mother’s unwillingness to breastfeed; inappropriate breastfeeding technique, and birth weight < 2500 g were the most significant factors in developing BFJ.
There were diverse statistics on the frequency of BFJ. Tanticharoenwiwat and Techasatid et al. (11) found that BFJ consisted of 47% of neonates’ hospitalizations due to jaundice. A study in Pakistan showed that the frequency of BFJ was 60% (12). Another study in USA confirmed that the frequency of BFJ was 15.5% (13). However, in our study, it was 35%. Effective breastfeeding in Iran seems to be better than Thailand and Pakistan. But it seems that race and genetic polymorphism are the main causes of jaundice and therefore the prevalence of early jaundice in diverse races is different. Neonatal hyperbilirubinemia is more common in residents of East Asian and around the Mediterranean, especially in Greece, and in people living in the highlands (1).
In one study, 36.5% of mothers had breast problems. Another study showed that the most common breast problem was depressed nipples (33.3%) (10, 14). In the present study, this problem was seen in 31.5% of mothers, which was statistically significant in comparison with mothers of NBFJ (5%). This problem showed that the examination and education of mothers before delivery were important and necessary.
A study found that the rate of breastfeeding in mothers who had early contact with neonates was 85%. This study showed that early contact was effective at initiating breastfeeding but had no effect on breastfeeding frequency and volume (15). In our study, early breastfeeding was 88%, which is consistent with the result of the above study, showing that early close infant-mother contact after birth is well observed.
In the Huang et al. (16) study, only neonates ≥ 2500 g were studied. This study showed that although weight loss and gestational age increased the risk of jaundice, but it was not due to ineffective breastfeeding in Chinese neonates. They believed that race was a significant factor in the development of jaundice. But our study also studied neonates < 2500 g and found that weight < 2500 g and inappropriate breastfeeding technique were important risk factors in BFJ.
The use of water or sugar water during breastfeeding reduces calorie intake and causes jaundice (17). According to the findings of the present research, the use of these supplements was about 20% which was statistically significant compared to the NBFJ (11%).
A study showed that proper breastfeeding can prevent weight loss and reduce the occurrence of jaundice (18). In our study, in 65.5% of newborns, breastfeeding was effective with proper technique and in 34.5% of newborns with BFJ was not found. This was an important factor that was statistically significant compared with the NBFJ.
Due to the side effects of SSRIs such as drowsiness and restlessness, which were seen especially in fluoxetine and citalopram, mothers who received these drugs may have more problems with breastfeeding. Therefore, these mothers need more support for breastfeeding, although this may be related to their underlying disease (19). In the present study, the mother’s unwillingness to breastfeed was 12% in BFJ and 1.6% in NBFJ groups that was a significant difference between the two groups; however, we did not study the effect of such drugs on breastfeeding.
Nilsson et al. (20) believed that early discharge of newborns could lead to nutritional problems and readmission, which could be due to inadequate breastfeeding and weight loss and as a result causing jaundice. In their study, mothers were hospitalized for 50 h and effective breastfeeding training was provided. They found that by effective breastfeeding, readmission rate and jaundice that required treatment were lower in their newborns (20). In Iran most of the newborns were discharged within the first 24 hours after birth. In our study, the mean length of hospitalization was 1.9 ± 0.537 days and proper breastfeeding training (close and appropriate mother-neonate contact, feeding in the first hours after delivery, and frequent breastfeeding) by physicians and nurses were done during hospitalization in 88%. But in practice, proper breastfeeding technique was seen in only about 65.5%, indicating that training of mothers should be provided more thoroughly, in simple methods and frequently by nurses to achieve proper and effective breastfeeding.
Another study showed that a bulletin about proper breastfeeding was effective. This study found that the quality of feeding increased from 48% to 63% (21). We did not use a bulletin, but with direct training the effective feeding rate was about 65.5%. It seems that using a bulletin can improve the breastfeeding technique.
This study showed that despite proper breastfeeding education in Iran, but in practice, breastfeeding technique, attention to breast problems, use of supplements (especially water and sugar water) during feeding and attention to newborns with weight < 2500 g were not sufficient, and these were the major causes of weight loss in newborns and breastfeeding jaundice. Most of the newborns were discharged within the first 24 hours after birth, which may be one of the main causes of inadequate attention to these risk factors. It is suggested that effective breastfeeding of mothers can be achieved by increasing the quality of education by midwives and nurses during pregnancy and also more attention to the above-mentioned risk factors in the first 24 hours after birth and, as a result, reducing the breastfeeding jaundice and readmission. Many of these above risk factors are related to before birth; thereby, the role of midwives, gynecologists, and nurses is crucial. One of the limitations of this study was the lack of studies on maternal education level and the number of previous deliveries in the quality of breastfeeding.
5.1. Conclusions
According to the findings of this study, the high prevalence of breastfeeding jaundice indicates that breastfeeding education policies need to be revised. Breastfeeding education before delivery, more attention of gynecologists to breast problems of mothers during pregnancy, professional coordination of nurses and physicians for effective breastfeeding training, and early mothers’ revisiting after the initial discharge of neonates can reduce the frequency of breastfeeding jaundice and readmission of neonates.
Acknowledgements
References
-
1.
Ullah S, Rahman K, Hedayati M. Hyperbilirubinemia in neonates: Types, causes, clinical examinations, preventive measures and treatments: a narrative review article. Iran J Public Health. 2016;45(5):558-68. [PubMed ID: 27398328]. [PubMed Central ID: PMC4935699].
-
2.
Preer GL, Philipp BL. Understanding and managing breast milk jaundice. Arch Dis Child Fetal Neonatal Ed. 2011;96(6):F461-6. [PubMed ID: 20688866]. https://doi.org/10.1136/adc.2010.184416.
-
3.
Ketsuwan S, Baiya N, Maelhacharoenporn K, Puapornpong P. The association of breastfeeding practices with neonatal jaundice. J Med Assoc Thai. 2017;100(3):255-61. [PubMed ID: 29911780].
-
4.
Prameela KK. Breastfeeding during breast milk jaundice - a pathophysiological perspective. Med J Malaysia. 2019;74(6):527-33. [PubMed ID: 31929480].
-
5.
Soldi A, Tonetto P, Chiale F, Varalda A, Peila C, Sabatino G, et al. Hyperbilirubinemia and management of breastfeeding. J Biol Regul Homeost Agents. 2012;26(3 Suppl):25-9. [PubMed ID: 23158510].
-
6.
Chou HC, Chen MH, Yang HI, Su YN, Hsieh WS, Chen CY, et al. 211 G to a variation of UDP-glucuronosyl transferase 1A1 gene and neonatal breastfeeding jaundice. Pediatr Res. 2011;69(2):170-4. [PubMed ID: 20975617]. https://doi.org/10.1203/PDR.0b013e31820263d2.
-
7.
Zhou S, Wang Z, He F, Qiu H, Wang Y, Wang H, et al. Association of serum bilirubin in newborns affected by jaundice with gut microbiota dysbiosis. J Nutr Biochem. 2019;63:54-61. [PubMed ID: 30342317]. https://doi.org/10.1016/j.jnutbio.2018.09.016.
-
8.
Soldi A, Tonetto P, Varalda A, Bertino E. Neonatal jaundice and human milk. J Matern Fetal Neonatal Med. 2011;24 Suppl 1:85-7. [PubMed ID: 21942599]. https://doi.org/10.3109/14767058.2011.607612.
-
9.
Rezakhaniha B, Sirosbakht S. Efficacy of selective serotonin reuptake inhibitor (SSRI) in patient with premature ejaculation. Int J Reproduct BioMed. 2010;8(2):55-9.
-
10.
Alizadeh Taheri P, Sepahran M, Shariat M. Maternal factors in newborns breast feeding jaundice: A case control study. Tehran Univ Med J. 2013;70(12).
-
11.
Tanticharoenwiwat P, Techasatid W. Outcome analysis of jaundice fast-track system implementation in Thammasat University Hospital. J Med Assoc Thai. 2014;97(5):500-5. [PubMed ID: 25065088].
-
12.
Ali R, Ahmed S, Qadir M, Ahmad K. Icterus Neonatorum in near-term and term infants: An overview. Sultan Qaboos Univ Med J. 2012;12(2):153-60. [PubMed ID: 22548133]. [PubMed Central ID: PMC3327561]. https://doi.org/10.12816/0003107.
-
13.
Maisels MJ, Gifford K. Neonatal jaundice in full-term infants. Role of breast-feeding and other causes. Am J Dis Child. 1983;137(6):561-2. [PubMed ID: 6846290]. https://doi.org/10.1001/archpedi.1983.02140320037007.
-
14.
Boskabadi H, Ramazanzadeh M, Zakerihamidi M, Rezagholizade Omran F. Risk factors of breast problems in mothers and its effects on newborns. Iran Red Crescent Med J. 2014;16(6). e8582. [PubMed ID: 25068067]. [PubMed Central ID: PMC4103000]. https://doi.org/10.5812/ircmj.8582.
-
15.
Hemachandra A, Puapornpong P, Ketsuwan S, Imchit C. Effect of early skin-to-skin contact to breast milk volume and breastfeeding jaundice at 48 hours after delivery. J Med Assoc Thai. 2016;99 Suppl 8:S63-9. [PubMed ID: 29901914].
-
16.
Huang A, Tai BC, Wong LY, Lee J, Yong EL. Differential risk for early breastfeeding jaundice in a multi-ethnic Asian cohort. Ann Acad Med Singapore. 2009;38(3):217-24. [PubMed ID: 19347075].
-
17.
Chang JH, Chan WT. Analysis of factors associated with initiation and duration of breast-feeding: A study in Taitung Taiwan. Acta Paediatr Taiwan. 2003;44(1):29-34. [PubMed ID: 12800381].
-
18.
Gartner LM. Breastfeeding and jaundice. J Perinatol. 2001;21 Suppl 1:S25-9. discussion S35-9. [PubMed ID: 11803412]. https://doi.org/10.1038/sj.jp.7210629.
-
19.
Rezakhaniha B, Siroosbakhat S. Comparative study of therapeutic effects of two medicinal procedures of citalopram in premature ejaculation. Biosci Biotechnol Res Asia. 2014;11(2):953-8. https://doi.org/10.13005/bbra/1365.
-
20.
Nilsson IMS, Strandberg-Larsen K, Knight CH, Hansen AV, Kronborg H. Focused breastfeeding counselling improves short- and long-term success in an early-discharge setting: A cluster-randomized study. Matern Child Nutr. 2017;13(4). [PubMed ID: 28194877]. https://doi.org/10.1111/mcn.12432.
-
21.
Tartaglia KM, Campbell J, Shaniuk P, McClead RE. A quality project to improve compliance with AAP guidelines for inpatient management of neonatal hyperbilirubinemia. Hosp Pediatr. 2013;3(3):251-7. [PubMed ID: 24313095]. https://doi.org/10.1542/hpeds.2012-0103.