Abstract
Keywords
Tendinitis Flexor Carpi Ulnaris Wrist Magnetic Resonance Imaging
1. Introduction
Calcific tendinitis also known as peritendinitis calcarea is a type of tendinopathy characterized by hydroxyapatite crystal deposition within or near the tendons, causing pain and swelling. Although this condition could happen anywhere in the body, it mostly occurs in the shoulder and greater trochanters of the hip and elbows. Gondos disclosed that the shoulder, hip, and elbow constitute about 90 percent of this type of calcification (1). Ankles, knees, and feet also could be affected and calcification is very rare at the wrist and the hand accounts for approximately 2.4 percent of all cases of calcific tendinitis (2).
Calcifications in the hand and wrist could present in metacarpophalangeal and interphalangeal joints as calcific periarthritis, at tendons as calcific tendinitis, in the articular cartilage as chondrocalcinosis and those at joint cavities as intraarticular calcification (3).
Calcific tendinitis of the hand occurs at the flexor and extensor tendons, but so far, the insertion of the flexor carpi ulnaris (FCU) tendon on the pisiform is the most common region (2, 4).
Few cases of calcific tendinitis of the wrist and hand have been described in some literature, and patients had the same acute symptoms including sudden-onset pain, swelling, edema and/or erythema often localized in the vicinity of the joint. However, unusual and rare presentations, such as carpal tunnel syndrome due to flexor digitorum tendon involvement within the carpal tunnel, acute compressive neuropathy of the ulnar nerve and trigger finger symptoms due to calcific tendinitis of the flexor digitorum tendons more distally at the level of the metacarpophalangeal joint, occasionally have been published in articles (5-7).
Owing to limited knowledge about this disorder and also non-specific symptoms overlapping with other entities, and the rare occurrence of this disease, under-recognition, and misdiagnosis is extremely common. This situation is actually misdiagnosed as acute fracture, septic arthritis, tendinopathy, gout, rheumatoid arthritis (RA) or crystalline arthropathy. For this reason, unnecessary medications and invasive procedures including surgery are not uncommon and this emphasizes the increasing role of imaging to reach the correct diagnosis (8).
2. Case Presentation
A 28-year-old male with no significant past medical history presented to the orthopedic clinic complaining of acute severe pain in the left wrist that had increased gradually over the course of one week. There was no history of trauma or significant medication and the patient was afebrile. Clinically, he had a tenderness and swelling over the volar aspect on the ulnar side of the wrist, and the hand and wrist motions were restricted. The pain was aggravated by ulnar deviation or flexion against resistance.
Initially, based on the suspicious radiographic changes at lunate, Kienbock disease was diagnosed by the orthopedist, a splint was ordered and the patient was referred to the imaging center for MRI. Upon further questioning, specifically about repetitive activities, he authorized changing his dominant hand and excessive usage recently and having sports activities over the weekend after the onset of his symptoms.
Radiography of the left wrist was normal without evidence in favor of Kienbock disease and obvious abnormal calcification distal to the ulnar head. Therefore, MRI was suggested for an accurate diagnosis. Proton density (PD) fat-saturated images of MRI revealed thickening and tendinosis of FCU tendon near insertion on pisiform without bone marrow signal changes over the carpal bones. The small signal void focus was better visualized on non- fat-saturated T1 weighted/PD images (Figure 1).
A 28-year-old man with acute severe pain in the left wrist aggravating over one week. Axial (A) and sagittal (B) proton density fat sutured magnetic resonance imaging (MRI) show soft tissue edema and thickened flexor carpi ulnaris (FCU) tendon near insertion on pisiform suggestive of tendinitis (arrows). Small signal void focus (arrows) visible within the tendon in keeping with calcification is noted which is better seen on sagittal T1 non fat-saturated (C), coronal three dimensional multiple echo recombined gradient echo (3D MERGE) (D) and coronal T1 non fat-saturated (E) images. Plain radiography (F) is normal.
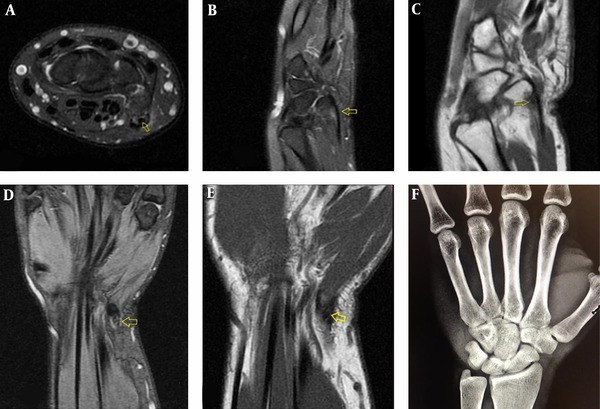
Retrospectively, minimal soft tissue swelling over the pisiform was observed only as a positive finding on radiography. Further evaluation by ultrasonography was performed to better demonstrate the calcified focus seen on MRI.
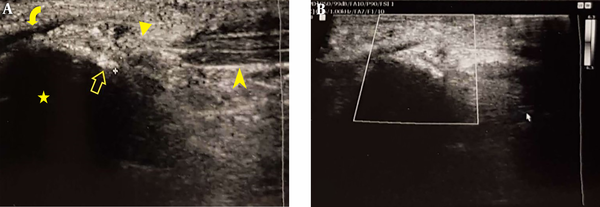
On ultrasonography, the distal of FCU tendon was thickened with echo-poor appearance, and fibrillar architecture was less-visible. The corresponding region of signal void on MRI images was echo-bright focus located within distal FCU tendon with posterior shadowing in keeping with calcific tendinitis of the FCU tendon (Figure 2).
Longitudinal grayscale (A) and color Doppler sonography (B) from the distal insertion of flexor carpi ulnaris (FCU) tendon revealed normal FCU fibers (arrowhead) continue distally (triangle) to produce distorted fibrillar pattern and tendon thickening due to tendinitis. Small echogenic focus (open arrows) located within the depth of distal FCU tendon is a calcific focus. Minimal increased flow within and around the tendon is evident (B). (Curved arrow, pisohamate ligament; stars, pisiforms).
Diagnosis of acute calcific tendinitis of FCU was made and subsequently. A palmar wrist splint was applied, nonsteroidal anti-inflammatory drugs (NSAIDs) were prescribed, and the patient was asked to rest. Two weeks after treatment, all symptoms and signs had resolved.
3. Discussion
FCU is a forearm muscle that proximally fastens at the medial epicondyle and distally attaches to the palmar surface of the pisiform, and then inserts into the hamate and fifth metacarpal bones as the pisohamate and pisometacarpal ligaments, respectively. FCU acts as the wrist flexor and adductor and such as a palmaris longus tendon, has no sheath, and therefore, does not cause tenovaginitis and stenosing tendon disorders. Calcific tendinitis also known as calcific periarthritis, peritendinitis calcarea, periarthritis calcarea, calcific bursitis, calcareous tendinitis and bursitis and hydroxyapatite rheumatism of the hand and wrist has been reported in the literature. The first description of acute calcific tendinitis of the wrist goes back to 1924 by Cohen and since then, several reports have been published.
Two large series including 209 patients with calcific tendinitis of the hand and wrist have been assessed by Carroll et al. (9) and Yelton and Dickey (10). They revealed that this entity is much more common than previously thought and the wrist is more affected than fingers. The most common site of calcification at the wrist is the distal insertion of FCU tendon on the pisiform.
Most cases of calcific tendinitis commonly occur between the ages of 30 and 60; however, no age is spared (11). Men and women are equally involved (10). Although calcific tendinitis is frequently asymptomatic in the shoulder, it is almost always symptomatic in the hand and wrist (2, 9, 10). The exact cascade of events that results in calcific deposition is not fully understood and still under question. Several authors have attributed this condition to tendon degeneration, hypoxia caused by poor blood supply, and trauma, while others have proposed that the calcifications are a cell-mediated reactive process. Uhthoff et al. explained local hypoxia induced by mechanical, metabolic, or other factors that lead to degeneration and metaplasia of the tendon to the fibrocartilage that results in calcification by chondrocytes (12).
Repetitive strain injuries and trauma cause stress necrosis and chronic inflammation, which have been postulated by Carroll et al. (9) as an etiology of such calcifications. Certain types of activity, such as sudden repeated motions and certain occupations such as typing, golfing or violin playing are more associated with this entity (13). Moyer et al. (14) presented cases of calcific tendonitis of the hand and wrist without a history of repetitive trauma or strain which considered to be idiopathic.
Calcific tendinitis is much more common at few conditions such as gout and rheumatoid arthritis (RA). Metabolic abnormalities could be associated with soft tissue calcification in hypervitaminosis D, hyperparathyroidism, and chronic renal failure. Hormonal disorders such as estrogen and thyroid hormones by Harvie et al. (15) and adult-onset diabetes mellitus by Mavrikakis et al. (16) are postulated as other possibilities that lead to calcific tendinitis. Gartner (17) and Sengar et al. (18) described an HLA-A1 gene predisposition with calcific tendinitis and Gohr et al. (19) suggested matrix vesicles could be the origin of the pathologic calcification.
Some researchers suggest that calcifications occur due to tendon degeneration, but most others believe that these are two distinct entities and have several differences. The age of inception of calcific tendinitis is earlier than that of degenerative tendinopathy (20). Calcific tendinitis may resolve, unlike degenerative tendinopathy. Calcific tendinitis occurs in viable tissue, but degenerative tendinopathy occurs in necrotic tissue (21). Deposits at calcific tendinitis are hydroxyapatite and have a different chemical composition compared to degenerative tendinopathy (22).
Seldom, calcific tendinitis may be seen before the onset of symptoms. Symptoms of calcific tendinitis are not due to the calcification itself and appear to happen when the calcific deposit rupture to adjacent soft tissue and result in acute inflammatory response consequently (23, 24).
On clinical examination, the disease is presented by tenderness over the distal tendon at the wrist which could be worsened by wrist flexion or ulnar deviation against resistance. Typically, the symptoms begin abruptly and initially are localized at the volar aspect of the ulnar side of the distal forearm and wrist but eventually are limited directly over the pisiform and distal of FCU within few days. Other symptoms such as swelling and erythema may be present as well.
Due to the rarity of calcific tendinitis at the distal insertion of FCU, and nonspecific symptoms, imaging has a fundamental role in the diagnosis of tendinopathy and calcific tendinitis.
Radiography is the primary and most used modality for evaluating calcific tendinitis (25). It is cost-effective and calcium deposits and their extension and density could be easily detected. Characteristically, degenerative joint evidence is usually absent (26).
Calcifications have been classified into two groups based on the shape and border on radiography (21, 26). In most cases, heterogeneous deposits with the fluffy appearance and ill-defined contour correlate with the acute symptomatic phase of calcific tendinitis, while the discrete homogeneous calcifications with well-defined edges are mostly seen in asymptomatic patients. Calcifications are usually amorphous and have varying shapes and sizes with irregular borders. Localized obliteration of fascial planes over the pisiform secondary to edema could be seen in the acute phase of calcific tendinitis (4). Over time, calcifications become less well-defined or hazy and may fragment and eventually disappear or markedly decrease in size (9). Rarely, calcifications are not visible on plain radiographs as in this case and may need other modalities for confirmation (21).
Computerized tomography (CT) is not routinely used for the diagnosis of calcific tendinitis. On CT, the appearance of calcification mirrors the radiographs (27). CT is the best modality for evaluating osseous involvement and cortical erosion and intramedullary extension of calcifications which is most often seen inside the femur and humerus and is very rare in the wrist and hand (28). CT is also helpful for localizing the disease to a tendon and confirming calcific tendinitis (27).
MRI is the second most commonly used modality after radiographs, performed for evaluation of calcific tendinitis, as it shows the presence of calcification and helps to characterize the extent of the inflammation and exclude other causes of joint pain. Sagittal plane provides a better diagnostic view for evaluating the full length of FCU tendon attachment on the pisiform. On MRI, the degree of soft tissue inflammation depends on the stage of the calcification.
Fluid sensitive MR images show soft tissue edema typically surrounding the region of calcification in the symptomatic phase. Calcifications present as focal areas of low signal on all pulse sequences located within or near the tendon insertion, although small deposits may be difficult to see by MRI and need radiography or ultrasonography for confirmation (29).
Ultrasonography is less expensive, easily accessible and the most-useful modality for the evaluation of hand and wrist tendons. Ultrasound is not routinely used for the diagnosis of calcific tendinitis, but it is useful particularly when calcification happens at shoulder tendons and is commonly used in image-guided therapeutic procedures. Longitudinal views of FCU tendon are obtained at the parasagittal plane while the wrist is mildly dorsiflexed. Within normal tendon, smooth tangential fibers are visible as echo-bright parallel thin lines that taper distally to attach on the pisiform. Tendinopathy causes loss of normal fibrillar pattern, hypoechogenicity, hypervascularity, and tendon thickening. Farin et al. (27) believe that although sonography is reliable in the recognition and localization of calcifications but it is unable to classify the pathophysiologic stage of calcifications in hand and wrist tendons. Because of this restriction and for evaluating bony abnormalities, they postulated that radiographs should be obtained in combination with ultrasound examination in calcific tendinitis for further confirmation. Increased flow on color Doppler is seen in symptomatic phases but is present in only about one-third of cases and is not necessary for diagnosis (30).
The acute calcific tendinitis has a very good prognosis. Carroll et al. (9) and Strandell (24) reported resolution of symptoms in untreated patients takes a long time, approximately three weeks. Immobilization by splinting and treatment with NSAIDs shortens the symptomatic period to 7 - 9 days (9). The success rate of nonsurgical interventions is high. Invasive treatment including local injection of anesthetic or steroid agents, aspiration of calcium deposits, surgical excision of calcific deposition and lysis of peritendinous adhesions are also available but are usually kept for severe cases that have not responded to conventional treatments and when symptoms last for more than several weeks (8).
In conclusion, due to the rapid clinical course, it is important to make the diagnosis early to prevent unnecessary interventions. The initial diagnosis is almost always incorrect. Infection and fractures must be included in the initial differential diagnosis to avoid terrible misdiagnosis. If a patient has erythema, localized pain, restricted motion and ectopic calcification on radiographs over the tender point, without a history of trauma or findings in favor of infection, acute calcific tendinitis must be considered in the differential diagnosis. Sonography and MRI could be employed for an accurate diagnosis. Increasing knowledge and awareness about this condition lead to an earlier diagnosis without exposing the patient to unnecessary interventions.
References
-
1.
Gondos B. Observations on periarthritis calcarea. Am J Roentgenol Radium Ther Nucl Med. 1957;77(1):93-108. [PubMed ID: 13381863].
-
2.
Selby CL. Acute calcific tendinitis of the hand: an infrequently recognized and frequently misdiagnosed form of periarthritis. Arthritis Rheum. 1984;27(3):337-40. [PubMed ID: 6704195]. https://doi.org/10.1002/art.1780270314.
-
3.
Beckmann NM. Calcium Apatite Deposition Disease: Diagnosis and Treatment. Radiol Res Pract. 2016;2016:4801474. [PubMed ID: 28042481]. [PubMed Central ID: PMC5155096]. https://doi.org/10.1155/2016/4801474.
-
4.
Gandee RW, Harrison RB, Dee PM. Peritendinitis calcarea of flexor carpi ulnaris. AJR Am J Roentgenol. 1979;133(6):1139-41. [PubMed ID: 116507]. https://doi.org/10.2214/ajr.133.6.1139.
-
5.
Harris AR, McNamara TR, Brault JS, Rizzo M. An unusual presentation of acute calcific tendinitis in the hand. Hand (N Y). 2009;4(1):81-3. [PubMed ID: 18780008]. [PubMed Central ID: PMC2654957]. https://doi.org/10.1007/s11552-008-9121-3.
-
6.
Yasen S. Acute calcific tendinitis of the flexor carpi ulnaris causing acute compressive neuropathy of the ulnar nerve: a case report. J Orthop Surg (Hong Kong). 2012;20(3):414-6. [PubMed ID: 23255660]. https://doi.org/10.1177/230949901202000333.
-
7.
Hansen U, Battista V. Pediatric trigger finger from calcific tendonitis. J Hand Surg Am. 2007;32(10):1558-9. [PubMed ID: 18070644]. https://doi.org/10.1016/j.jhsa.2007.08.005.
-
8.
Shim MR. Unusual Etiology of Acute Wrist Pain: Acute Calcific Tendonitis of the Flexor Carpi Ulnaris Mimicking an Infection. Case Rep Orthop. 2018;2018:2520548. [PubMed ID: 30538878]. [PubMed Central ID: PMC6261391]. https://doi.org/10.1155/2018/2520548.
-
9.
Carroll RE, Sinton W, Garcia A. Acute calcium deposits in the hand. J Am Med Assoc. 1955;157(5):422-6. [PubMed ID: 13221441]. https://doi.org/10.1001/jama.1955.02950220016005.
-
10.
Yelton CL, Dickey LE, Jr. Calcification about the hand and wrist. South Med J. 1958;51(4):489-95. [PubMed ID: 13529268]. https://doi.org/10.1097/00007611-195804000-00014.
-
11.
Louwerens JK, Sierevelt IN, van Hove RP, van den Bekerom MP, van Noort A. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg. 2015;24(10):1588-93. [PubMed ID: 25870115]. https://doi.org/10.1016/j.jse.2015.02.024.
-
12.
Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat Res. 1976;(118):164-8. [PubMed ID: 954272].
-
13.
Edmondson M, Skyrme A. Occupationally related bilateral calcific tendonitis of Flexor carpi ulnaris: case report. J Orthop Surg Res. 2009;4:33. [PubMed ID: 19698164]. [PubMed Central ID: PMC2738660]. https://doi.org/10.1186/1749-799X-4-33.
-
14.
Moyer RA, Bush DC, Harrington TM. Acute calcific tendinitis of the hand and wrist: a report of 12 cases and a review of the literature. J Rheumatol. 1989;16(2):198-202. [PubMed ID: 2664164].
-
15.
Harvie P, Pollard TC, Carr AJ. Calcific tendinitis: natural history and association with endocrine disorders. J Shoulder Elbow Surg. 2007;16(2):169-73. [PubMed ID: 17188907]. https://doi.org/10.1016/j.jse.2006.06.007.
-
16.
Mavrikakis ME, Drimis S, Kontoyannis DA, Rasidakis A, Moulopoulou ES, Kontoyannis S. Calcific shoulder periarthritis (tendinitis) in adult onset diabetes mellitus: a controlled study. Ann Rheum Dis. 1989;48(3):211-4. [PubMed ID: 2930276]. [PubMed Central ID: PMC1003723]. https://doi.org/10.1136/ard.48.3.211.
-
17.
Gartner J. [Is tendinosis calcarea associated with HLA-A1?]. Z Orthop Ihre Grenzgeb. 1993;131(5):469. [PubMed ID: 8256496].
-
18.
Sengar DP, McKendry RJ, Uhthoff HK. Increased frequency of HLA-A1 in calcifying tendinitis. Tissue Antigens. 1987;29(3):173-4. [PubMed ID: 3496685].
-
19.
Gohr CM, Fahey M, Rosenthal AK. Calcific tendonitis : a model. Connect Tissue Res. 2007;48(6):286-91. [PubMed ID: 18075814]. https://doi.org/10.1080/03008200701692362.
-
20.
Ark JW, Flock TJ, Flatow EL, Bigliani LU. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy. 1992;8(2):183-8. [PubMed ID: 1637430].
-
21.
Uhthoff HK, Loehr JW. Calcific Tendinopathy of the Rotator Cuff: Pathogenesis, Diagnosis, and Management. J Am Acad Orthop Surg. 1997;5(4):183-91. [PubMed ID: 10797220].
-
22.
Riley GP, Harrall RL, Constant CR, Cawston TE, Hazleman BL. Prevalence and possible pathological significance of calcium phosphate salt accumulation in tendon matrix degeneration. Ann Rheum Dis. 1996;55(2):109-15. [PubMed ID: 8712860]. [PubMed Central ID: PMC1010104]. https://doi.org/10.1136/ard.55.2.109.
-
23.
McCarty DJ, Gatter RA. Recurrent acute inflammation associated with focal apatite crystal deposition. Arthritis Rheum. 1966;9(6):804-19. [PubMed ID: 5927932]. https://doi.org/10.1002/art.1780090608.
-
24.
Strandell G. Peritendinitis calcarea in the hand. Acta Chir Scand. 1963;125:42-51. [PubMed ID: 13984533].
-
25.
Colavita N, Solivetti FM, Vecchioli A, Bock E. Peritendinitis calcarea of flexor carpi ulnaris. Diagn Imaging. 1983;52(5):284-6. [PubMed ID: 6617429].
-
26.
Depalma AF, Kruper JS. Long-term study of shoulder joints afflicted with and treated for calcific tendinitis. Clin Orthop. 1961;20:61-72. [PubMed ID: 13721957].
-
27.
Farin PU. Consistency of rotator-cuff calcifications. Observations on plain radiography, sonography, computed tomography, and at needle treatment. Invest Radiol. 1996;31(5):300-4. [PubMed ID: 8724130].
-
28.
Mascarenhas VV, Morais F, Marques H, Guerra A, Carpinteiro E, Gaspar A. [Calcifying tendinitis of the rotator cuff with focal umeral osteolysis. Imaging features]. Acta Reumatol Port. 2015;40(4):378-83. Portuguese. [PubMed ID: 26922202].
-
29.
Chung CB, Gentili A, Chew FS. Calcific tendinosis and periarthritis: classic magnetic resonance imaging appearance and associated findings. J Comput Assist Tomogr. 2004;28(3):390-6. [PubMed ID: 15100546]. https://doi.org/10.1097/00004728-200405000-00015.
-
30.
Le Goff B, Berthelot JM, Guillot P, Glemarec J, Maugars Y. Assessment of calcific tendonitis of rotator cuff by ultrasonography: comparison between symptomatic and asymptomatic shoulders. Joint Bone Spine. 2010;77(3):258-63. [PubMed ID: 20434387]. https://doi.org/10.1016/j.jbspin.2010.01.012.