Abstract
Keywords
Pain Procedures Sacral Plexus Pain Syndromes Sacral Nerves Entrapment Neuropathy Neuroanatomy Chronic Pain
1. Context
The sacral plexus or sacral nerve roots may be damaged by diseases, such as disc herniation, spinal canal stenosis, and cancer (1) or iatrogenic injuries during surgery or interventional pain procedures (open spinal surgeries, hip surgeries, percutaneous endoscopic disc decompression, trans-sacral epiduroscopic laser decompression, …) (2, 3). Patients with sacral nerve damage may experience a variety of symptoms, including low back pain radiating to the legs, sensory disturbance in the buttocks or legs, motor weakness in the legs, bladder or bowel dysfunction (urinary retention/incontinence, defecation’s problems), or sexual dysfunction (4).
Each sacral spinal nerve root is formed by the combination of the dorsal and ventral sacral root of the spinal cord. The sacral nerve roots (S1, S2, S3, S4, and S5) pass through the sacral canal and are divided into the anterior and posterior rami. The anterior rami of the upper four sacral nerve roots (S1 to S4) emerge from the anterior sacral foramina and join the lumbosacral trunk (which carries fibers from L4 and L5 lumbar nerve roots) to form the sacral plexus (Figure 1). The posterior rami pass through the posterior sacral foramina and innervate the erector spinal muscles and the overlying skin (5).
Sacral plexus, corresponding nerve roots, and terminal branches.
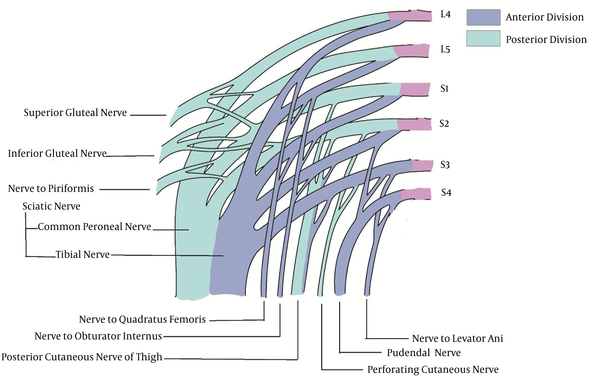
The sacral plexus is located on the posterior pelvic wall, anterior to the piriformis muscle. The branches of the sacral plexus (Figure 1 and Table 1) are distributed as follows: (1) To the lower limb: (a) Superior gluteal nerve; (b) Inferior gluteal nerve; (c) Sciatic nerve (and its branches: tibial and common peroneal nerves); (d) Posterior cutaneous nerve of thigh; (e) Nerve to quadratus femoris. (2) To pelvic wall and floor: (a) Nerve to levator ani; (b) Nerve to piriformis; (c) Nerve to obturator internus. (3) To perineum: (a) Pudendal nerve.
Sacral Plexus
| Nerve | Origin | Motor | Sensory |
|---|---|---|---|
| Superior gluteal | L4, L5, and S1 | Gluteus medius, gluteus minimus, tensor fasciae latae | _ |
| Inferior gluteal | L5, S1, and S2 | Gluteus maximus | _ |
| Sciatic | L4, L5, S1, S2, and S3 | hamstring, adductor magnus; Tibial: plantaris, soleus, gastrocnemius, popliteus, tibialis posterior, flexor digitorum longus and flexor hallucis longus; Common peroneal: fibularis longus and Brevis muscle tibialis anterior, extensor hallucis longus, fibularis tertius, and extensor digitorum longus | Tibial: posterolateral leg, lateral surface of the foot, and sole of the foot.; Common peroneal: anterolateral leg and dorsal aspect of the foot. |
| Posterior cutaneous nerve of thigh | S1, S2, and S3 | _ | perineum, the posterior surface of the thigh, and various areas of the back of the leg. |
| Nerve to quadratus femoris | L4, L5, and S1 | Quadratus femoris, inferior gemellus | _ |
| Nerve to levator ani | S3 and S4 | Levator ani, coccygeus | _ |
| Nerve to piriformis | L5, S1, and S2 | Piriformis | _ |
| Nerve to obturator internus | L4, L5, and S1 | Obturator internus, superior gemellus | _ |
| Pudendal | S2, S3, and S4 | external urethral sphincter, external anal sphincter, levator ani, and skeletal muscles of the perineum | external genitalia and skin of the perineum |
2. Superior Gluteal Nerve (SGN)
2.1. Anatomy
The SGN is made up of the posterior division of the ventral rami of L4, L5, and S1 nerve roots. This nerve (SGN) is the only nerve that leaves the pelvis through the greater sciatic foramen, above the piriformis muscle (6). Other nerves that exit through the greater sciatic foramen (pudendal, inferior gluteal, and sciatic nerve, etc.) pass under the piriformis muscle.
2.2. Function
The SGN innervates the gluteus minimus muscle (responsible for hip abduction and medial rotation of the thigh), gluteus medius (hip abductor), and tensor fascia latae muscles (hip extensor) (7, 8).
2.3. Clinical Pearls
Damage to the SGN can occur for a variety of reasons, including: (1) Trauma (falling on the buttocks, hip extension in a motor vehicle accident, hip fracture, spondylolisthesis, and intramuscular injection in the buttocks, ...). (2) Surgery (hip surgeries, hip arthroplasty, ...). (3) Entrapment (piriformis muscle hypertrophy, vascular aneurysm, ...) (9).
Patients with SGN injury complain of pain in the lower back and buttock, which continues down the leg and foot. These symptoms can lead to misdiagnosis as a lumbar disc herniation and are sometimes referred to as pseudo-sciatica (9, 10).
On physical examination, unilateral damage to the SGN leads to weakness of the abductor muscles and a positive Trendelenburg sign. In the case of bilateral nerve damage, the patient shows a Waddling gait (8).
In post-surgical injuries or trauma, spontaneous healing may occur. Patients with nerve entrapment sometimes require the injection of the local anesthetic and steroid at the point of entrapment (under fluoroscopy or ultrasound guidance). In some cases, surgery is needed to repair the damage (8, 10).
3. Inferior Gluteal Nerve (IGN)
3.1. Anatomy
The IGN is formed from the posterior division of L5, S1, and S2 nerve roots of the sacral plexus. The nerve exits in the pelvis through the greater sciatic foramen, below the piriformis muscle (11).
3.2. Function
The IGN is responsible for innervating the gluteus maximus muscle (hip extensor and hip joint external rotator) (12, 13).
3.3. Clinical Pearls
Injury to the IGN can be caused by nerve compression due to pelvic or colorectal masses, piriformis syndrome, trauma due to intramuscular injection, and hip surgery (14).
Patients with IGN involvement complain of buttock pain and gluteus maximus muscle atrophy or weakness in hip extension may be seen (11).
Treatment varies depending on the cause. In cases of secondary nerve entrapment to piriformis syndrome, injection with a local anesthetic and steroid under fluoroscopic or ultrasound guidance, and if unresponsive, injection of botulinum toxin may be helpful (14).
4. Sciatic Nerve (SN)
4.1. Anatomy
The SN is the largest nerve in humans. It originates from both posterior and anterior divisions of the ventral rami of L4, L5, S1, S2, and S3 nerve roots. The SN leaves the pelvis through the sciatic foramen, below the piriformis muscle (15, 16).
4.2. Function
The SN travels along the posterior thigh and innervates the hamstring muscles (hip extensors and knee flexors) and the adductor Magnus muscle (hip adductor and knee flexor) (17).
4.3. Clinical Pearls
Sciatica is defined as irritation or compression of the SN. The most common causes of sciatica include disc herniation and compression of the L5 and S1 nerve roots, spinal canal stenosis, degenerative disk disease, and spondylolisthesis. Less common causes include intra-pelvic pathologies (pregnancy, infection, and vascular causes), hip fracture or surgery, piriformis syndrome, sacroiliitis, and trauma (17, 18).
Patients with SN involvement complain of lower back and buttock pain radiating to the lower limb. There may be weakness or numbness in the SN distribution. The straight leg raising (SLR) is positive in 90% of patients with SN entrapment (18).
Most causes of sciatica improve with conservative treatment. If there is no response, interventional techniques are the next appropriate treatment option depending on the underlying cause. In cases of disc herniation, epidural steroid injection or percutaneous laser disc decompression can be regarded as the treatments in selected patients. If there is no response to interventional techniques or there are progressive signs and symptoms (motor or sensory deficit), the patient can be a candidate for surgery (open or endoscopic surgery).
5. Tibial Nerve (TN)
5.1. Anatomy
In most patients, the SN in the lower third of the thigh, near the apex of the popliteal fossa, divides into two branches (19). The anterior branch of the SN is the TN.
5.2. Function
TN continues downward to innervate posterior compartment of the leg and foot, which includes the plantaris, soleus, gastrocnemius, popliteus, tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles (plantar flexors and toes flexors) (20). The TN also provides sensory innervations of the posterolateral leg, lateral surface of the foot, and sole of the foot (21, 22).
5.3. Clinical Pearls
Causes of TN entrapment are numerous and include synovial cyst, hemodialysis, varicose veins, thrombophlebitis, osteomyelitis, fractures of the foot bones, postsurgical scars, and sports injuries (23).
Proximal injury to the TN at the knee area may occur due to baker cysts, osteoarthritis, etc., but the distal injury to the TN is more common (11). TN is often compressed in the tarsal tunnel, which is called the tarsal tunnel syndrome. Patients complain of burning pain and numbness in the plantar surface of the foot and toes. On physical examination, the Tinel sign is positive.
Conservative treatment and in case of no response, a steroid injection is recommended. In some cases, surgical treatment is used for decompression of the TN (20).
6. Common Peroneal Nerve (CPN)
6.1. Anatomy
The posterior branch of the SN is the CPN
6.2. Function
The CPN travels down to innervate lateral compartment of the leg, which includes the fibularis longus and brevis muscles (foot eversion) (24), and anterior compartment of the leg, which includes the tibialis anterior, extensor hallucis longus, fibularis tertius, and extensor digitorum longus muscles (foot dorsiflexor and toes extensor). The CPN also provides sensory innervations of the anterolateral leg and dorsal aspect of the foot (25).
6.3. Clinical Pearls
Causes of CPN injury include lateral knee trauma, knee arthroplasty, sports injuries, such as long squats or cycling, and surgery, especially lithotomy, fibula fracture, popliteal aneurysm, etc. (26). CPN neuropathy is the most common mononeuropathy in the lower extremities. CPN neuropathy often occurs due to nerve compression in the fibula head because the nerve is superficial in this area (11).
Patients with CPN involvement due to weakness of the foot dorsiflexion show partial or complete foot drop and slapping gate, which cause difficulty in walking and climbing stairs.
Depending on the cause of the neuropathy and the patient's lack of response to conservative treatment, the injection technique can be used with ultrasound or fluoroscopy guidance. In some cases, surgery is recommended (26).
7. The Posterior Cutaneous Nerve of the Thigh
7.1. Anatomy
The posterior cutaneous nerve of the thigh is also known as the posterior femoral cutaneous nerve (PFCN) formed from the posterior division of the ventral rami of the S1 and S2 and the anterior division of the ventral rami of S2 and S3 nerve roots. The PFCN emerges from the pelvis through the greater sciatic foramen, below the piriformis muscle (27).
7.2. Function
This nerve is the pure sensory nerve and has no motor innervations. The PFCN innervates the skin of the perineum, the posterior surface of the thigh, and various areas of the back of the leg (28, 29).
7.3. Clinical Pearls
The posterior cutaneous nerve can be compressed by the piriformis muscle or by prolonged use of a thigh tourniquet. The nerve can be damaged by ischial tuberosity following prolonged sitting on the edge of a chair or biking. Gluteal muscle injection may also cause PFCN injury. Pain due to the posterior cutaneous nerve entrapment is felt in the buttocks and medial side of the thigh and various parts of the leg. The patient may also experience sensory disturbances in the lower buttock or back of the thigh.
If conservative treatment does not respond, fluoroscopic-, CT-, or MRI-guided injection of the PFCN is recommended. In some cases, surgery is necessary to release the nerve entrapment (30).
8. Nerve to Quadratus Femoris (NQF)
8.1. Anatomy
The nerve to quadrates femoris originates from the anterior division of the ventral rami of L4, L5, and S1 nerve roots of the sacral plexus. The NQF exists in the pelvis through the lower part of the greater sciatic foramen, below the piriformis muscle, and deep to the SN (31).
8.2. Function
This nerve, in addition to innervating the quadrates femoris muscle (adductor and external rotator of the thigh) (32), is responsible for innervating the inferior gemellus muscle (thigh external rotator) and providing the articular branch for the posterior hip joint capsule (31, 33).
8.3. Clinical pearls
Few studies have been performed on quadratic nerve pathologies and research is ongoing (34).
Ischiofemoral impingement syndrome refers to narrowing the space between the ischium and the femur with entrapment of soft tissues. Causes of this syndrome include congenital, such as hip dysplasia, acquired deformity, such as a fracture or femoral osteoarthritis, or iatrogenic causes, such as hip surgery.
Patients complain of hip pain that is exacerbated by hip extensions and long strides.
Research on treatments is limited. However, in the absence of response to protective treatment, CT-guided quadratic muscle injection is recommended. In some cases, surgery is necessary (35).
9. Levator ani Nerve (LAN)
9.1. Anatomy
The nerve to levator ani is formed from the anterior division of the ventral rami of S3 and S4 spinal nerve roots.
9.2. Function
The LAN is responsible for innervating the levator ani muscle (pelvic and abdomen stabilizer and control the opening and closing of the levator hiatus) and the coccygeus muscle (pelvis supporter and pulling the coccyx forward after defecation) (36, 37).
9.3. Clinical pearls
levator ani syndrome is the result of a levator muscle spasm that is felt with pain and pressure in the rectal, sacral, and coccygeal areas. The pain is aggravated by sitting. The diagnosis is clinical and ruling out other causes. Treatment includes muscle relaxant, biofeedback, massage, sitz bath, and electro-galvanic stimulation (38).
10. Nerve to Piriformis
10.1. Anatomy
The nerve to piriformis originates from the posterior division of the ventral rami of the S1 and S2 spinal nerve root of the sacral plexus. The nerve to piriformis leaves the pelvis through a greater sciatic foramen, below the piriformis.
10.2. Function
The nerve to piriformis innervates the piriformis muscle (hip external rotator) (39, 40).
10.3. Clinical Pearls
Piriformis syndrome is usually caused by proximal compression of the SN. In 50% of cases, the cause of piriformis syndrome is trauma to the buttock or lower limb, which leads to the formation of hematomas and scars between the piriformis muscle and the SN (41). Other causes include anatomical abnormalities, piriformis muscle hypertrophy, spasm, and Myositis ossificans of the piriformis muscle, secondary to laminectomy, etc. (42).
Patients have pain in the lower back, buttock with radiation to ipsilateral leg. On physical examination, the pace test is positive that reproduces pain and weakness to resisted abduction and external rotation.
Depending on the cause, treatment includes conservative treatment (medication, applying heat, massage, stretching exercise, etc.), piriformis muscle injection (guided by fluoroscopy, ultrasound, or CT scan), or surgery (in refractory cases) (41).
11. Nerve to Obturator Internus
11.1. Anatomy
The nerve to obturator internus is formed from the anterior division of the ventral rami of L5, S1, and S2 spinal nerve roots. The nerve to obturator internus emerges from the pelvis through a greater sciatic foramen, below the piriformis muscle, and after providing a branch to the superior gemellus muscle, crosses the ischial spine and reenters the pelvis through the lesser sciatic foramen (31).
11.2. Function
The nerve provides innervations for internal obturator muscle (thigh abductor and external rotator of extent thigh) and superior gemellus muscle (thigh external rotator) (32, 33).
11.3. Clinical Pearls
Obturator internus-gemelli syndrome is often caused by SN entrapment at the junction of the superior gemelli and obturator internus muscles and the scissor-like effect created by the two muscles. Due to the similarity of structure and function, most treatments used in piriformis syndrome also affect obturator internus-gemelli syndrome (43).
12. Pudendal Nerve
12.1. Anatomy
The pudendal nerve consists of the ventral rami of S2, S3, and S4 spinal nerve roots. The pudendal nerve leaves the pelvis through a greater sciatic foramen, below the piriformis muscle, and then turns around the posterior aspect of the sacrococcygeal ligament at the ischial spine and reenters the pelvis through the lesser sciatic foramen (44). After exciting the sciatic foramen, the nerve travels to the pudendal canal.
12.2. Function
The pudendal nerve gives the motor branches to the external urethral sphincter, external anal sphincter, levator ani, and skeletal muscles of the perineum. The nerve also provides sensory innervations of the external genitalia and skin of the perineum (45).
12.3. Clinical pearls
Causes of pudendal neuralgia include nerve compression following cycling or prolonged sitting, direct blow to the pelvis, chronic constipation, gynecological or hip surgeries, immunologic or infectious disorders, etc. Patients with pudendal nerve involvement present with symptoms, such as pain and numbness in the pudendal nerve distribution, including the genitalia, anorectal region, and the terminal urinary tract. There may also be symptoms, such as sexual dysfunction (painful intercourse, vulvodynia, etc.) or sphincter dysfunction (fecal incontinence, burning when urinating, etc.), and foreign body sensation in the anus or vagina. On physical examination, depending on the site of injury, tenderness over the greater sciatic notch or ischium can be felt (44). The symptoms may be exacerbated with passive hip external or internal rotation.
Depending on the cause of pudendal neuralgia, medication (NSAIDs, anticonvulsants, and antidepressant) or physical therapy may be helpful, and in case of no response, patients may benefit from injection techniques (under fluoroscopy or ultrasound guidance) or surgical treatments (46).
References
-
1.
Rubin DI. Brachial and lumbosacral plexopathies: A review. Clin Neurophysiol Pract. 2020;5:173-93. [PubMed ID: 32954064]. [PubMed Central ID: PMC7484503]. https://doi.org/10.1016/j.cnp.2020.07.005.
-
2.
Chang MC. Sacral root injury during trans-sacral epiduroscopic laser decompression: A case report. Medicine (Baltimore). 2017;96(42). e8326. [PubMed ID: 29049245]. [PubMed Central ID: PMC5662411]. https://doi.org/10.1097/MD.0000000000008326.
-
3.
Hasija R, Kelly JJ, Shah NV, Newman JM, Chan JJ, Robinson J, et al. Nerve injuries associated with total hip arthroplasty. J Clin Orthop Trauma. 2018;9(1):81-6. [PubMed ID: 29628688]. [PubMed Central ID: PMC5884042]. https://doi.org/10.1016/j.jcot.2017.10.011.
-
4.
Van Boxem K, Cheng J, Patijn J, van Kleef M, Lataster A, Mekhail N, et al. 11. Lumbosacral radicular pain. Pain Pract. 2010;10(4):339-58. [PubMed ID: 20492580]. https://doi.org/10.1111/j.1533-2500.2010.00370.x.
-
5.
Gosling JA. Atlas of human anatomy with integrated text. Gower Medical Pub; 1985.
-
6.
Jacobs LG, Buxton RA. The course of the superior gluteal nerve in the lateral approach to the hip. J Bone Joint Surg Am. 1989;71(8):1239-43. [PubMed ID: 2777853].
-
7.
Caviglia H, Cambiaggi G, Vattani N, Landro ME, Galatro G. Lesion of the hip abductor mechanism. SICOT J. 2016;2:29. [PubMed ID: 27382925]. [PubMed Central ID: PMC4935799]. https://doi.org/10.1051/sicotj/2016020.
-
8.
Lung K, Lui F. Anatomy, abdomen and pelvis, superior gluteal nerve. Treasure Island (FL): StatPearls; 2018. Portuguese.
-
9.
Trescot AM. Superior gluteal nerve entrapment. Peripheral nerve entrapments. Springer; 2016. p. 571-9. https://doi.org/10.1007/978-3-319-27482-9_53.
-
10.
McCrory P, Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999;27(4):261-74. [PubMed ID: 10367335]. https://doi.org/10.2165/00007256-199927040-00005.
-
11.
Craig A. Entrapment neuropathies of the lower extremity. PM & R. 2013;5(5 Suppl):S31-40. [PubMed ID: 23542774]. https://doi.org/10.1016/j.pmrj.2013.03.029.
-
12.
Ling ZX, Kumar VP. The course of the inferior gluteal nerve in the posterior approach to the hip. J Bone Joint Surg Br. 2006;88(12):1580-3. [PubMed ID: 17159167]. https://doi.org/10.1302/0301-620X.88B12.18182.
-
13.
Merryman J, Asuka E, Varacallo M. Anatomy, abdomen and pelvis, inferior gluteal nerve. Treasure Island (FL): StatPearls; 2020.
-
14.
Trescot AM. Inferior gluteal nerve entrapment. Peripheral nerve entrapments. Springer, Cham; 2016. p. 581-7.
-
15.
Ribeiro FS, Bettencourt Pires MA, Silva Junior EX, Casal D, Casanova-Martinez D, Pais D, et al. [Rethinking sciatica in view of a bilateral anatomical variation of the sciatic nerve, with low origin and high division: Historical, anatomical and clinical approach]. Acta Med Port. 2018;31(10):568-75. [PubMed ID: 30387425]. https://doi.org/10.20344/amp.10567.
-
16.
Dupont G, Unno F, Iwanaga J, Oskouian RJ, Tubbs R. A variant of the sciatic nerve and its clinical implications. Cureus. 2018. https://doi.org/10.7759/cureus.2874.
-
17.
Giuffre BA, Jeanmonod R. Anatomy, sciatic nerve. StatPearls; 2020.
-
18.
Gallagher AE, Gulati A, Dallas-Prunskis T. Proximal sciatic nerve entrapment: Low back. Peripheral nerve entrapments. Springer; 2016. p. 589-603.
-
19.
Berihu BA, Debeb YG. Anatomical variation in bifurcation and trifurcations of sciatic nerve and its clinical implications: in selected university in Ethiopia. BMC Res Notes. 2015;8:633. [PubMed ID: 26526618]. [PubMed Central ID: PMC4630888]. https://doi.org/10.1186/s13104-015-1626-6.
-
20.
Desai SS, Cohen-Levy WB. Anatomy, bony pelvis and lower limb, tibial nerve. StatPearls; 2019.
-
21.
Torres AL, Ferreira MC. Study of the anatomy of the tibial nerve and its branches in the distal medial leg. Acta Ortop Bras. 2012;20(3):157-64. [PubMed ID: 24453596]. [PubMed Central ID: PMC3718430]. https://doi.org/10.1590/S1413-78522012000300005.
-
22.
Davis TJ, Schon LC. Branches of the tibial nerve: Anatomic variations. Foot Ankle Int. 1995;16(1):21-9. [PubMed ID: 7697149]. https://doi.org/10.1177/107110079501600105.
-
23.
Brown MN, Pearce BS, Trescot AM, Karl HW. Tibial nerve entrapment. Peripheral nerve entrapments. Springer; 2016. p. 819-31.
-
24.
Khan IA, Mahabadi N, D'Abarno A, Varacallo M. Anatomy, bony pelvis and lower limb, leg lateral compartment. Treasure Island (FL): StatPearls; 2021.
-
25.
Hardin JM, Devendra S. Anatomy, bony pelvis and lower limb, calf common peroneal (fibular) nerve. Treasure Island (FL): StatPearls Publishing; 2020.
-
26.
Murinova N, Chiu SC, Krashin D, Karl HW. Common peroneal nerve entrapment. Peripheral nerve entrapments. Springer; 2016. p. 745-57.
-
27.
Dumitru D, Nelson MR. Posterior femoral cutaneous nerve conduction. Arch Phys Med Rehabil. 1990;71(12):979-82. [PubMed ID: 2241545].
-
28.
Feigl GC, Schmid M, Zahn PK, Avila Gonzalez CA, Litz RJ. The posterior femoral cutaneous nerve contributes significantly to sensory innervation of the lower leg: an anatomical investigation. Br J Anaesth. 2020;124(3):308-13. [PubMed ID: 31973825]. https://doi.org/10.1016/j.bja.2019.10.026.
-
29.
Singh K. Spine essentials handbook. New York: Thieme; 2019.
-
30.
Murinova N, Krashin D, Trescot AM. Posterior femoral cutaneous nerve entrapment: Low back. Peripheral nerve entrapments. Springer; 2016. p. 605-13.
-
31.
Miniato M, Varacallo M. Anatomy, back, lumbosacral trunk. Treasure Island (FL): StatPearls; 2020.
-
32.
Aung HH, Sakamoto H, Akita K, Sato T. Anatomical study of the obturator internus, gemelli and quadratus femoris muscles with special reference to their innervation. Anat Rec. 2001;263(1):41-52. [PubMed ID: 11331970]. https://doi.org/10.1002/ar.1075.
-
33.
Lezak B, Massel DH. Anatomy, bony pelvis and lower limb, gemelli muscles. Treasure Island (FL): StatPearls Publishing; 2021.
-
34.
Mehta K, Tubbs R. The nerve to quadratus femoris. Surgical anatomy of the sacral plexus and its branches. Elsevier; 2021. p. 35-9.
-
35.
Gollwitzer H, Banke IJ, Schauwecker J, Gerdesmeyer L, Suren C. How to address ischiofemoral impingement? Treatment algorithm and review of the literature. J Hip Preserv Surg. 2017;4(4):289-98. [PubMed ID: 29250337]. [PubMed Central ID: PMC5721376]. https://doi.org/10.1093/jhps/hnx035.
-
36.
Wallner C, van Wissen J, Maas CP, Dabhoiwala NF, DeRuiter MC, Lamers WH. The contribution of the levator ani nerve and the pudendal nerve to the innervation of the levator ani muscles; a study in human fetuses. Eur Urol. 2008;54(5):1136-42. [PubMed ID: 18036724]. https://doi.org/10.1016/j.eururo.2007.11.015.
-
37.
Nyangoh Timoh K, Bessede T, Lebacle C, Zaitouna M, Martinovic J, Diallo D, et al. Levator ani muscle innervation: Anatomical study in human fetus. Neurourol Urodyn. 2017;36(6):1464-71. [PubMed ID: 27813139]. https://doi.org/10.1002/nau.23145.
-
38.
Gowda SN, Bordoni B. Anatomy, abdomen and pelvis, levator ani muscle. StatPearls; 2021.
-
39.
Iwanaga J, Eid S, Simonds E, Schumacher M, Loukas M, Tubbs RS. The majority of piriformis muscles are innervated by the superior gluteal nerve. Clin Anat. 2019;32(2):282-6. [PubMed ID: 30408241]. https://doi.org/10.1002/ca.23311.
-
40.
Akita K, Sakamoto H, Sato T. Stratificational relationship among the main nerves from the dorsal division of the sacral plexus and the innervation of the piriformis. Anat Rec. 1992;233(4):633-42. [PubMed ID: 1626722]. https://doi.org/10.1002/ar.1092330417.
-
41.
Waldman SD. Pain management E-book. Elsevier Health Sciences; 2011.
-
42.
Jankovic D, Peng P, van Zundert A. Brief review: Piriformis syndrome: Etiology, diagnosis, and management. Can J Anaesth. 2013;60(10):1003-12. [PubMed ID: 23893704]. https://doi.org/10.1007/s12630-013-0009-5.
-
43.
Hernando MF, Cerezal L, Perez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: Anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal Radiol. 2015;44(7):919-34. [PubMed ID: 25739706]. https://doi.org/10.1007/s00256-015-2124-6.
-
44.
Kaur J, Singh P. Pudendal nerve entrapment syndrome. Treasure Island (FL): StatPearls Publishing; 2019.
-
45.
Maldonado PA, Chin K, Garcia AA, Corton MM. Anatomic variations of pudendal nerve within pelvis and pudendal canal: clinical applications. Am J Obstet Gynecol. 2015;213(5):727 e1-6. [PubMed ID: 26070708]. https://doi.org/10.1016/j.ajog.2015.06.009.
-
46.
Chowdhury SK, Trescot AM. Pudendal nerve entrapment. Switzerland: Springer International Publishing; 2016.