Abstract
Background:
The stigma associated with mental health disorders has an enormous impact on decisions concerning receiving mental health services.Objectives:
The current qualitative study aimed to describe the stigma toward mental disorders in Tehran, Iran.Methods:
The current grounded theory study conducted from 2013 to 2016 in Tehran (Iran). Fourteen participants were sampled using purposive and theoretical sampling techniques. Data were collected through face-to-face interviews, focused groups, and written narratives. The Corbin and Strauss coding paradigm (2008) was used to analyze data.Results:
Three main categories of stigmatization toward patients with mental health diagnoses were extracted: (1) barriers to stigma reduction; (2) strategies to reduce stigma; and (3) outcomes of stigma reduction such as negative consequences of stigma toward mental disorders and positive impacts of stigma reduction toward mental disorders.Conclusions:
To improve mental health services for patients in Tehran (Iran), it is imperative to reduce the stigma toward mental disorders, educate the community, including the general population and healthcare professionals, and remove existing barriers to receive mental health services.Keywords
Grounded Theory Mental Disorder Mental Health Psychiatry Qualitative Research Stigmatization
1. Background
Nearly 1 in 5 individuals (17.6%) worldwide are at risk of mental disorders (1); one in six US adults (44.7 million in 2016) (2) and 23% of the Iranian adults in 2015 (3) had a mental health diagnosis. The prevalence of common mental disorders is increasing, particularly in lower-income countries (4). In low-and-middle-income countries, 76% - 85% of individuals with mental health disorders do not receive treatment, compared to 35% - 50% in high-income countries (5). There are many reasons why an individual might not receive therapy. According to the National Comorbidity Survey Replication conducted in the United States, 73% of individuals with mental health problems reported a desire to self-heal, 45% of patients refused treatment, and 42% dropped out of treatment because of low perceived need for support (6).
The stigma associated with mental health disorders has an enormous impact on decisions concerning receiving mental health services (7). Mental health-related stigma is defined as a negative stereotype, prejudice, discrimination, and harmful beliefs, which can lead to emotional distress for patients and their families, difficulty in access to and benefiting from treatment, and an overall negative impact on daily living, such as losing the job (8, 9). A recent systematic review reported that stigma leads to inaccessibility of treatment for individuals with mental health conditions, and thus worsening of their psychological symptoms (10).
Individuals with anxiety and/or depression diagnosis are at increased risk of discrimination (11, 12). Internalized stigma may damage self-confidence. A public stigma can lead to discrimination and isolation of those with a mental health challenge (13). Previous studies reported that stigma can cause (or exacerbate) social inequalities in housing, education, employment, income, social relations, and health services (10, 14, 15).
Besides, stigma toward psychiatric patients differs depending on the culture (16, 17). In Islam, there are contextual differences among practices and beliefs about health and illness across Muslim groups. Some Muslims believe the God influences everything, including illnesses; in fact, mental illness may be perceived as a test or punishment (18). Ciftci et al. (18) reported that many Muslims prefer to share psychiatric problems with religious leaders rather than medical professionals. In Malaysia, with a large Muslim population, stigma toward mental health has created a culture of discrimination for patients, their families, and the community (19). Similarly, in Iran, which most of the population is Muslim, there is a high rate of stigma toward those who receive mental health services (20). However, according to the studies, the level of stigma in Iran is similar to Europe (20). Also, the common belief that the rate of stigma toward psychiatric patients is lower in Muslim societies, such as Iran, than western societies, is not correct (21). For example, individuals with mental health problems in Tehran were thought to be dangerous, violent, a nuisance, bring shame to the family, and not to be spoken to (20-22). Up to 40% of patients who were living in Tehran report moderate to severe stigma, such as alienation, discrimination, and social withdrawal (20).
In Iran healthcare providers and academics believe that mental disorders have a genetic biological cause; however, some of them discriminate against individuals with mental health disorders. Ebrahimi et al. (23) found that 70% of nurses in psychiatry wards had a medium level of stigma toward psychiatric patients, which included stereotypes, prejudice, and discrimination, and 48.8% believed that individuals with mental health concerns should be socially isolated. Amini et al. (24) found that contrary to the results of other studies conducted in other Islamic countries, beliefs in supernatural causes of mental illness was rare among Iranian medical students and most believed that genetic or biological factors are the main cause. Awareness about impacts of multi-factorial etiologies, consisting of genetic, biological, psychological, and social determinants (25), is expanding and will likely increase the tolerance of societies by reducing the stigma and rejection toward individuals with mental health disorders (24).
Stigma is common for individuals with psychiatric disorders in Iran and requires research, attention, system-wide changes, and a change in individual beliefs to reduce it. Educational interventions have been successful to decrease stigma, including face-to-face training, public media education, and online education (26). Considering the importance of the phenomenon of stigma, the cultural and socioeconomic differences of Iran, and the lack of comprehensive qualitative research on the consequences of stigma toward mental disorders, there is a need to address this phenomenon. Healthcare providers have a key role to reduce stigma toward patients with mental disorders. If they recognize the importance of addressing the interventions in this regard, the quality of life (Qol) of patients may be expected to increase.
2. Objectives
The current study attempted to describe the stigma toward mental disorders in Tehran, Iran. Since, the grounded theory intends to gain in-depth knowledge about the socially-shared meaning that forms the participants’ behaviors, which are not tied to any preexisting theory, its results have the potential for innovative discoveries. So, grounded theory was used to explore the stigma and the positive consequences of reducing it.
3. Methods
3.1. Design
The current qualitative study was conducted from 2013 to 2016 using the Corbin and Strauss (27) grounded theory methodology in Tehran, Iran.
3.2. Participants and Sampling
Inclusion criteria were working in the mental health field and willingness to participate. Next, these criteria were expanded to former patients with mental health disorders and their families. Experts of the Mental Health and Social Health and Addiction (MEHSHAD) Office in the Ministry of Health and Medical Education (MoHME) proposed seven key informants. Besides, seven participants were selected by the researchers through theoretical sampling method to reach theoretical saturation and to develop the emerging theory. Various participants from different fields who were in continuous contact with psychiatric patients (n = 12), a recovered patient, and a family member of two schizophrenia patients were recruited in the study. It should be noted that two individuals refused to participate in the study due to a lack of time. A total of 14 participants participated in the study (Table 1). Written informed consent was obtained and all interviews were recorded by a digital voice recorder.
Characteristics of the Participants and Data Collection Method(s)
| Code | Sex | Degree | Organization | Collection Method |
|---|---|---|---|---|
| P1 | Male | MD | Tehran University of Medical Sciences | FGD1, FGD2 |
| P2 | Male | MD | Support Forum of Schizophrenia Patients | FGD1, FGD2, WN |
| P3 | Male | BS | Recovered patient | FGD1, FGD2, WN |
| P4 | Male | MA | Islamic Development Organization | FGD1, FGD2, SSI |
| P5 | Male | MA | Tehran Municipality Health Office | FGD1, FGD2, SSI |
| P6 | Male | MD | Office of Social Pathology Prevention of Welfare Organization | FGD1, FGD2, SSI |
| P7 | Male | PhD | Association of Clinical Psychology | FGD1, FGD2, SSI |
| P8 | Female | MA | Family member of psychiatric patient | FGD1, FGD2, WN |
| P9 | Male | MD | University of Social Welfare and Rehabilitation Sciences | FGD1, FGD2, WN |
| P10 | Male | MD | Islamic Republic of Iran Broadcasting | FGD1, FGD2 |
| P11 | Male | PhD | Iranian Health Education and Promotion Association | SSI |
| P12 | Female | MD | Office of Social Pathology Prevention of Welfare Organization | SSI, WN |
| P13 | Male | MD | Armed Forces Medical Services Insurance Organization | SSI |
| P14 | Female | MD | Health Insurance of the Ministry of Welfare, Cooperation, Labor and Social Affairs | SSI, WN |
3.3. Data Collection
Data about all measures of stigma in mental health services were collected over a total of nine months by using semi-structured face-to-face interviews (SSI), focused group discussions (FGDs), and written narratives. Interviews were conducted in Persian, the participant’s native language. Participants varied in their contribution to the study, some participants completed all three SSI, FGD, and written narrative and others only one. See Table 1.
The research team comprised of a psychiatrist and a psychologist experienced in treating patients with mental disorders, and a PhD in nursing with experience in qualitative studies. A general practitioner and two researchers with MSc in psychology who were experienced in caring for patients with mental health disorders also supported the research team.
Over the first six months of the study, eight semi-structured SSIs were conducted. SSIs were conducted following an interview guide composed by the authors (Table 2). Interviews were conducted in the participants’ workplace. If necessary, probing questions were used. On average, the interviews lasted between 60 to 90 minutes. Also, ten participants engaged in FGDs, which were held by the psychiatrist and three researchers over three months. The FGDs were divided into two sessions, which were analyzed separately. Each session lasted 120 minutes, on average. Example questions from the FGD sessions are presented in Table 2. Data obtained from FGDs were considered as heterogeneous units and responses of each participant were analyzed separately.
Main Questions of Interviews to Describe Outcomes of Stigma Toward Mental Disorders in the SSIs and FGDs
| Session Type | Main Questions |
|---|---|
| SSIs | What is your experience regarding the presence of stigma toward patients with mental disorders? |
| What are the negative outcomes of the stigma toward mental disorders? | |
| What are the positive consequences of stigma reduction programs toward mental disorders? | |
| FGD1 | What experience do you have in the field of stigma toward mental disorders? |
| What causes the occurrence of stigma toward mental disorders? | |
| What are the outcomes of stigma toward patients with mental disorders? | |
| FGD2 | What are the solutions for reducing stigma toward mental disorders? |
| What can be done about eliminating or reducing stigma? | |
| What are the barriers to removing stigma toward mental disorders? |
A narrative approach was used with the participation of six patients. Narration is a powerful tool to transfer or to share opinions and experiences. As some participants might not have liked to share all of their experiences and opinions in the SSIs and FGDs, and often opinions would come to mind after the sessions. Participants were asked to write their experiences and views on the stigma toward mental disorders. Narratives were written wherever the participants were more comfortable and they could call the researchers whenever needed.
Interviewers recorded field notes during the interviews, and all interviews were transcribed word-by-word. In addition to the verbal responses of the participants, behavioral responses, such as notation of emotional and physical reactions during the interview, were also recorded.
3.4. Data Analysis
Data analysis was performed using the Corbin and Strauss (27) coding paradigm to extract perspectives and experiences of participants on outcomes of stigma towards mental disorders. This coding system created codes (derived and developed concepts from data) for further analyses. Two trained researchers performed data coding. Researchers extracted the main concepts, including actions/reactions/interactions, outcomes, and the process of reducing stigma toward mental disorders. Constant comparison method was used at all stages of analysis where each incident of an opinion regarding stigma toward mental disorders found in the data was compared with other incidents to consider differences and similarities. If incidents founded to be theoretically similar, they were categorized together to create a higher-level concept. In addition, theoretical comparisons were used to simulate thinking about properties (characteristics or components of an event or action) and dimensions (variations of a property along with a range) of categories.
Microanalysis and general analysis were used to compare interviews within and between participants. Most situations were a combination of micro conditions that referred to information directly related to the individual, such as personal beliefs, and macro conditions which referred to opinions, such as political, historical, social, and cultural conditions. The researchers identified the properties and dimensions of all categories. The relationships between the main categories (strategies to reduce the stigma, barriers to reduce stigma, and outcomes of reducing stigma toward mental disorders) and the central category (promoting psychological awareness) were also identified in the process of coding. The central category was the abstract concept that all other categories were related to and frequently appeared in the data.
Data comparison, asking questions, writing storylines, drawing diagrams, memoing, and reviewing memos (specialized written records that contain the products of analysis (27)) were among the techniques used in the coding process. Besides, the transcripts, categories, and sub-categories were returned to some participants to receive their comments or for correction. The MAXQDA software (Ver.10.0 R250412) was used to categorize and analyze the data. Codes, categories, and subcategories were translated into English.
3.5. Trustworthiness
Trustworthiness was assured through establishing proper communication with participants, conducting frequent interviews, prolonged engagement in study (the 24-month presence of researchers in the field improved the trust of the participants and provided a greater understanding of participants’ culture and context), full immersion in data (the researchers immersed themselves in the participants’ world, attending meetings with or about participants, reading documents on the subjects, and observing interactions in the setting helped researchers to immerse in data), member check (participants’ feedback or validation of findings), peer review, using triangulation (multiple methods) for data collection, a limited review of the literature, precise recording, systematic data collection, and reporting of all stages of the study. Also, one of the trained researchers with a PhD degree was well-experienced in performing qualitative studies, that some of her research are published in international journals. She conducted the methodology.
3.6. Ethical Considerations
The current study is approved by the Research Ethics Committee of the MoHME (No.: 2014/458883-0), and the principles of ethics in research presented in the Helsinki Declaration were followed. For example, written informed consent was obtained from all participants, anonymity, and confidentiality of the information were preserved, the right to withdraw from the study was informed to all participants, respect for the rights of authors, and necessary permissions were obtained from relevant authorities.
4. Results
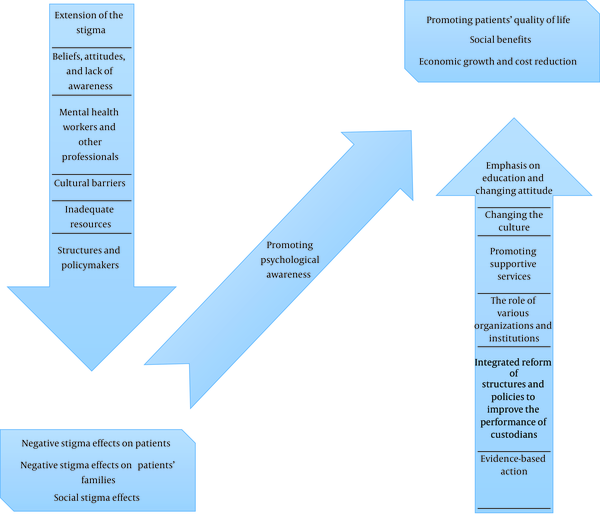
Data reduction revealed three main categories: Strategies to reduce the stigma toward mental disorder (strategies of reduction) (28), Barriers of stigma reduction toward mental disorders (barriers of reduction) (29), and Outcomes of stigma reduction toward mental disorders (Stigma outcomes). The central category that described as “the central phenomenon around which all the other categories are integrated” (27), was “the promotion of psychological awareness” (Table 3). The first two categories were reported by previous studies conducted on the same population of individuals in Iran (28, 29) and the focus of this article is on the last category.
The Main Categories and Sub-Categories Emerged From Data
| Main categories | Sub-Categories |
|---|---|
| Strategies to reduce the stigma toward mental disorders | Emphasis on education and changing attitudes |
| Changing the culture | |
| Promoting supportive services | |
| Role of various organizations and institutions | |
| Integrated reform of structures and policies to improve the performance of custodians | |
| Evidence-based actions | |
| Barriers of stigma reduction toward mental disorders | The prevalence of stigma |
| Beliefs, attitudes, and lack of awareness | |
| Mental health providers and other specialists | |
| Cultural barriers | |
| Structures and policymakers | |
| Insufficient financial resources | |
| Stigma outcome | Negative consequences of stigma toward mental disorders such as, negative effects of stigma on patients; negative effects of stigma on patients’ families; negative outcomes of stigma on the society |
| Positive impacts of stigma reduction toward mental disorders such as, promoting patients’ quality of life; social benefits; economic growth and cost reduction |
Stigma outcome included two sub-categories: Negative consequences of stigma toward mental disorders (negative consequences), and Positive impacts of reducing stigma toward mental disorders (positive impacts).
4.1. Negative Outcomes of Stigma Toward Mental Disorders
The negative consequences subcategory included three main areas of interest, negative effects of stigma on patients, negative effects of stigma on the patients’ families, and negative outcomes of stigma on the society.
Concerning the negative effects of stigma on patients, the majority of participants reported that stigma has several negative consequences, such as lack of referral for treatment, discrimination in treatment, delay to getting help and treatment, allocation of lower resources for treating these patients, marginalization and deprivation, increased crime and involvement in law enforcement due to discrimination, increased disrespectful behaviors from people, such as making jokes or unpleasant or inappropriate comments, and financial challenges including non-coverage of psychiatric services by health insurance schemes, high cost of treatment, inability to find a proper job, and livelihoods problems, such as insufficiency of income to meet necessities.
One participant reported that “psychiatric patients are less likely to be admitted to general hospitals. Also, psychiatric wards are separated from other parts of the general hospitals, to isolate and differentiate patients with mental disorders with other patients. Because of this label, they have been told are at asylum” (P1).
Concerning the negative effects of stigma on the patient’ families, participants reported that in addition to the burden of caring for a mentally ill family member, the stigma toward their family members and their disorder reduced the support and treatment for families and thus increased family stress. A family member reported that “the torment of mental illness stigma makes the family fall into a vortex that multiplies their torture” (P8).
Concerning the negative outcomes of stigma on society, participants reported that stigma toward patients with mental disorders exacerbates the treatment-related problems, including investment of resources, quality of care, and care standards. Expanded stigma causes lower morality and humanistic behaviors among different classes of society, which results in increased anger, neglect, and humiliating behaviors toward individuals with mental health problems. Such situations negatively affect the development and implementation of basic programs along with diagnosis and treatment. Stigma leads to increased treatment expenditures, along with negative economic and social consequences. For example, one participant said that “Stigma toward mental disorders increases individualism and promotes the demoralization of society” (P11).
4.2. Positive Outcomes of Stigma Reduction Toward Mental Disorders
The second subcategory of Stigma outcomes (i.e., Positive Outcomes) comprises three areas of interest: Promoting patients’ QoL, social benefits, and Economic growth and cost reduction.
Stigma reduction programs are based on the assumption that if discrimination reduces over time, individuals with mental health disorders are more likely to receive services they need as well as the support to live a more fruitful life. In terms of promoting QoL, most participants reported that stigma reduction programs improved the QoL of mental health patients and their families, and provided an improved outlook toward mental health across society. Improved QoL for mental health patients consisted of increased rights and liberties for patients, such as rights to treatment, social care, and social inclusion. Stigma reduction programs increased the belief that individuals with mental health concerns should have the freedom to express their beliefs without fear of persecution or judgment. One participant reported, “therapeutic facilities teach that the rights and needs of patients with mental illnesses are as important as individuals without mental health problems. Increased mental health support allows others to realize the legal rights of citizens with mental illness” (P3).
In terms of social benefits, participants expressed that the representation of psychiatric patients in society allows them to become active and successful contributors to the community.
Participants felt that being in the society would prove their efficacy and decrease the severity of mental illness. One participant noted that “famous people with psychiatric diseases should be introduced to the community so that people understand that a person who suffers from mental illness can be successful, and thus other patients can also success” (P7).
Concerning the economic growth and cost reduction, participants reported that the successful reduction of stigma towards patients with mental disorders leads to alleviation of the financial burden imposed on households with a member who has mental health concerns and reduces economic loss for organizations due to the employee’s absence from work. Participants reported that with the economic growth of governmental and non-governmental organizations, the costs of mental health care in society will be moderated and patients will be more likely to receive treatment.
4.3. Core Variable: Promoting of Psychological Awareness
The relationships between the main emerged categories are shown in Figure 1. The “core variable” was “the promotion of psychological awareness”. Also, the “basic social process” was the same. The concept of “promoting psychological awareness” was evident in all categories and it was connected to other categories, like a bridge between the main categories. Reducing stigma barriers had a negative impact on the level of psychological awareness of the community and were the main cause of the slowed reduction of stigma in Iran. in Iran, negative outcomes of stigma toward psychiatric patients had negative effects on both patients and their families, and had social consequences. The strategies for reducing stigma in mental disorders, through the promotion of community psychological awareness, accelerate the process of reducing stigma in Iran. The final results of the process of reducing stigma toward patients with mental disorders included improving the QoL, social benefits, economic growth, and cost reduction.
Effective factors on stigma toward mental disorders in Iran
5. Discussion
The current qualitative study reported overall concerns regarding stigma toward mental disorders in Tehran (Iran) and suggested that promoting psychological awareness would improve the treatment process and socioeconomic status of psychiatric patients and their relatives by reducing the negative outcomes of stigma. Participants reported that the negative consequences of stigma reduce QoL, social benefits, and economic growth. Furthermore, the stigma associated with a mental health disorder leads to fear of treatment and lack of referral for higher-level care. Practices such as the separation of the psychiatric wards from the general medical settings and specialized psychiatric hospitals perpetuate the stigma. Consistent with the current study, previous investigations emphasized the negative impacts of stigma toward mental health on receiving or continuing the treatment (10), occupational and economic status (30), social relationships (31), and QoL (32). According to the previous studies, internalized stigma influences the severity of psychiatric symptoms, seeking treatment, and treatment adherence, which result in deprivation from basic needs, poverty, reduction in life satisfaction, medical complications, and even death by self-neglect or suicide (7, 11).
Participants of the current study also reported concerns for both the stigma projected on the families of patients and with the stigma generated from family onto the patient. Stigma not only affects the patients themselves but also their family members may disrupt the treatment process, which imposes economic, social, and psychological pressures on the patient’s family. Similar research showed that the main contributors to discriminatory behaviors toward mentally ill patients were generated from their own family, friends, and colleagues (19). In Ghana, economic problems, social isolation, depression, and lack of time for other responsibilities were reported as challenges facing families of patients with mental health concerns (33). In a study conducted in Tehran, about 25% of people mentioned that having a family member with mental health problems is an embarrassment (21).
Participants also discussed that decreasing the stigma has positive impacts on QoL of psychiatric patients. Similar to other research, participants emphasized the decline in unemployment and delinquency of individuals with mental health problems as positive results of stigma reduction (10). Most of the participants believed that augmenting public awareness about psychological illnesses increases the QoL of patients, and introducing famous persons with psychiatric diseases can be useful. They reported that by introducing successful people with psychiatric illnesses, it is possible to reduce social stigmatization. Similarly, it is realized that community education and integration of psychiatric patients into society will decrease stigma and improve the QoL of mental health patients (32, 34).
Participants believed that economic growth and reduction in costs of mental health care would reduce stigma, result in earlier treatment, less unemployment, and less negative impact on QoL for patients. A systematic review of the economic impacts of the stigma on psychiatric patients found that stigma toward patients has a negative impact on their employment and income as well as the general interest in the allocation of public resources for psychiatric care. Also, it is concluded that the reduction of stigma can have positive economic effects, and to achieve this goal, national, regional, and global planning as well as public campaigns are needed (30). Therefore, it should be noted that allocating more resources for stigma reduction programs is reasonable, given the fact that it will lead to economic growth and lower costs in the future.
Psychological awareness can reduce negative stigma toward patients, their families, and the community, which in turn improves the QoL of patients with psychiatric disorders and reduces costs. Previous studies focused on strategies to reduce stigma toward psychiatric patients and obstacles toward planned changes (28, 29). According to the findings of the current study, psychological awareness can be promoted through educational programs to change attitudes, increasing supportive services, development of appropriate policies, and evidence-based actions. Effectiveness of educational programs intended to increase awareness, such as lectures, video clips, and direct exposure to psychiatric patients, is well proved; although direct contact with psychiatric patients is reported as the most effective strategy to reduce stigma (35, 36). Participants believed that reducing barriers would increase the psychological awareness of people and thus reduce stigma towards patients. Relatively limited transferability is of limitations to the current study, particularly given its qualitative nature. However, the present study provided a rich and contextualized understanding of its participants and their experience with mental health, which provide useful information to guide future research, policy-making, and medical care.
5.1. Conclusions
Stigma about mental health disorders has a significant impact on individuals with mental disorders. Stigma can disrupt the treatment process, create disturbance in the social and occupational life of individuals, and cause various problems for their family. Promoting psychological awareness through stigma-reduction programs can lead to lower stigma and thus improving the QoL for patients, reducing costs of mental health care, and economic growth. It is recommended to conduct further studies to explore the process of changing the stigma toward mental disorders and factors that affect it in other settings.
Acknowledgements
References
-
1.
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43(2):476-93. [PubMed ID: 24648481]. [PubMed Central ID: PMC3997379]. https://doi.org/10.1093/ije/dyu038.
-
2.
National Institue of Mental Health. Mental illness: The National Institute of Mental Health Information Resource Center. 2018, [cited 2018 Jul 1]. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml.
-
3.
Noorbala AA, Faghihzadeh S, Kamali K, Bagheri Yazdi SA, Hajebi A, Mousavi MT, et al. Mental health survey of the Iranian adult population in 2015. Arch Iran Med. 2017;20(3):128-34. [PubMed ID: 28287805].
-
4.
World Health Organization. Depression and other common mental disorders - Global health estimates. 2017, [cited 2018 Jul 01]. Available from: http://apps.who.int/iris/bitstream/10665/254610/1/WHO-MSD-MER-2017.2-eng.pdf.
-
5.
World Health Organization. Mental disorder. 2017, [cited 2018 Jul 01]. Available from: http://www.who.int/mediacentre/factsheets/fs396/en/.
-
6.
Mojtabai R, Olfson M, Sampson NA, Jin R, Druss B, Wang PS, et al. Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med. 2011;41(8):1751-61. [PubMed ID: 21134315]. [PubMed Central ID: PMC3128692]. https://doi.org/10.1017/S0033291710002291.
-
7.
Shrivastava A, Johnston M, Bureau Y. Stigma of mental illness-1: Clinical reflections. Mens Sana Monogr. 2012;10(1):70-84. [PubMed ID: 22654383]. [PubMed Central ID: PMC3353607]. https://doi.org/10.4103/0973-1229.90181.
-
8.
Sartorius N, Gaebel W, Cleveland HR, Stuart H, Akiyama T, Arboleda-Florez J, et al. WPA guidance on how to combat stigmatization of psychiatry and psychiatrists. World Psychiatry. 2010;9(3):131-44. [PubMed ID: 20975855]. [PubMed Central ID: PMC2948719]. https://doi.org/10.1002/j.2051-5545.2010.tb00296.x.
-
9.
Corrigan PW, Bink AB. The stigma of mental illness. Encyclopedia of Mental Health. 2016. p. 230-4. https://doi.org/10.1016/b978-0-12-397045-9.00170-1.
-
10.
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11-27. [PubMed ID: 24569086]. https://doi.org/10.1017/S0033291714000129.
-
11.
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150-61. [PubMed ID: 21051128]. https://doi.org/10.1016/j.socscimed.2010.09.030.
-
12.
Griffiths KM, Batterham PJ, Barney L, Parsons A. The Generalised Anxiety Stigma scale (GASS): psychometric properties in a community sample. BMC Psychiatry. 2011;11:184. [PubMed ID: 22108099]. [PubMed Central ID: PMC3248354]. https://doi.org/10.1186/1471-244X-11-184.
-
13.
Brown C, Conner KO, Copeland VC, Grote N, Beach S, Battista D, et al. Depression stigma, race, and treatment seeking behavior and attitudes. J Community Psychol. 2010;38(3):350-68. [PubMed ID: 21274407]. [PubMed Central ID: PMC3026177]. https://doi.org/10.1002/jcop.20368.
-
14.
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813-21. [PubMed ID: 23488505]. [PubMed Central ID: PMC3682466]. https://doi.org/10.2105/AJPH.2012.301069.
-
15.
Moses T. Being treated differently: Stigma experiences with family, peers, and school staff among adolescents with mental health disorders. Soc Sci Med. 2010;70(7):985-93. [PubMed ID: 20122768]. https://doi.org/10.1016/j.socscimed.2009.12.022.
-
16.
Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: An integrative review. Clin Psychol Rev. 2011;31(6):934-48. [PubMed ID: 21683671]. https://doi.org/10.1016/j.cpr.2011.05.003.
-
17.
Mellor D, Carne L, Shen YC, McCabe M, Wang L. Stigma toward mental illness. J Cross-Cult Psychol. 2012;44(3):352-64. https://doi.org/10.1177/0022022112451052.
-
18.
Ciftci A, Jones N, Corrigan PW. Mental health stigma in the muslim community. J Muslim Mental Health. 2013;7(1). https://doi.org/10.3998/jmmh.10381607.0007.102.
-
19.
Hanafiah AN, Van Bortel T. A qualitative exploration of the perspectives of mental health professionals on stigma and discrimination of mental illness in Malaysia. Int J Ment Health Syst. 2015;9:10. [PubMed ID: 25774215]. [PubMed Central ID: PMC4359579]. https://doi.org/10.1186/s13033-015-0002-1.
-
20.
Ghanean H, Nojomi M, Jacobsson L. Internalized stigma of mental illness in Tehran, Iran. Stigma Res Action. 2011;1(1). https://doi.org/10.5463/sra.v1i1.10.
-
21.
Ghanean H, Nojomi M, Jacobsson L. A community study on attitudes to and knowledge of mental illness in Tehran. Open J Psychiatry. 2015;5(1):26-30. https://doi.org/10.4236/ojpsych.2015.51004.
-
22.
Nojomi M, Malakouti SK, Ghanean H, Joghataei MT, Jacobson L. Mental illness stigma in city of Tehran, 2009. Razi J Med Sci. 2010;17(78/79):43-52.
-
23.
Ebrahimi H, Namdar H, Vahidi M. Mental illness stigma among nurses in psychiatric wards of teaching hospitals in the north-west of Iran. Iran J Nurs Midwifery Res. 2012;17(7):534-8. [PubMed ID: 23922602]. [PubMed Central ID: PMC3730459].
-
24.
Amini H, Majdzadeh R, Eftekhar-Ardebili H, Shabani A, Davari-Ashtiani R. How mental illness is perceived by iranian medical students: A preliminary study. Clin Pract Epidemiol Ment Health. 2013;9:62-8. [PubMed ID: 23878611]. [PubMed Central ID: PMC3715759]. https://doi.org/10.2174/1745017901309010062.
-
25.
Baradaran Eftekhari M, Setareh Forouzan A, Mirabzadeh A, Sajadi H, Dejman M, Rafiee H, et al. Mental health priorities in Iranian women: Overview of social determinants of mental health. Iran J Psychiatry. 2014;9(4):271-4. [PubMed ID: 25792993]. [PubMed Central ID: PMC4361828].
-
26.
Griffiths KM, Carron-Arthur B, Parsons A, Reid R. Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry. 2014;13(2):161-75. [PubMed ID: 24890069]. [PubMed Central ID: PMC4102289]. https://doi.org/10.1002/wps.20129.
-
27.
Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory. 3rd ed. 2008. https://doi.org/10.4135/9781452230153.
-
28.
Taghva A, Farsi Z, Javanmard Y, Atashi A, Hajebi A, Noorbala AA. Strategies to reduce the stigma toward people with mental disorders in Iran: Stakeholders' perspectives. BMC Psychiatry. 2017;17(1):17. [PubMed ID: 28088199]. [PubMed Central ID: PMC5237535]. https://doi.org/10.1186/s12888-016-1169-y.
-
29.
Taghva A, Farsi Z, Javanmard Y, Atashi A, Hajebi A, Khademi M. Stigma barriers of mental health in Iran: A qualitative study by stakeholders of mental health. Iran J Psychiatry. 2017;12(3):163-71. [PubMed ID: 29062367]. [PubMed Central ID: PMC5640577].
-
30.
Sharac J, McCrone P, Clement S, Thornicroft G. The economic impact of mental health stigma and discrimination: A systematic review. Epidemiol Psichiatr Soc. 2010;19(3):223-32. [PubMed ID: 21261218]. https://doi.org/10.1017/s1121189x00001159.
-
31.
Elena Lemonis BB. Effects of internalized stigma of mental disorder on quality of life and selfesteem in panic disorder patients. J Clin Rese Bioethics. 2014;5(5). https://doi.org/10.4172/2155-9627.1000196.
-
32.
Chronister J, Chou CC, Liao HY. The role of stigma coping and social support in mediating the effect of societal stigma on internalized stigma, mental health recovery, and quality of life among people with serious mental illness. J Commun Psychol. 2013;41(5):582-600. https://doi.org/10.1002/jcop.21558.
-
33.
Ae-Ngibise KA, Doku VC, Asante KP, Owusu-Agyei S. The experience of caregivers of people living with serious mental disorders: A study from rural Ghana. Glob Health Action. 2015;8:26957. [PubMed ID: 25967587]. [PubMed Central ID: PMC4429259]. https://doi.org/10.3402/gha.v8.26957.
-
34.
Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42(8):1741-52. [PubMed ID: 22085422]. https://doi.org/10.1017/S0033291711002558.
-
35.
Payton JW, Wardlaw DM, Graczyk PA, Bloodworth MR, Tompsett CJ, Weissberg RP. Social and emotional learning: A framework for promoting mental health and reducing risk behavior in children and youth. J Sch Health. 2000;70(5):179-85. [PubMed ID: 10900594]. https://doi.org/10.1111/j.1746-1561.2000.tb06468.x.
-
36.
Yamaguchi S, Mino Y, Uddin S. Strategies and future attempts to reduce stigmatization and increase awareness of mental health problems among young people: A narrative review of educational interventions. Psychiatry Clin Neurosci. 2011;65(5):405-15. [PubMed ID: 21851449]. https://doi.org/10.1111/j.1440-1819.2011.02239.x.