Abstract
Background:
Multiple sclerosis (MS) is a chronic, common, and progressive disease of the nervous system, and the affected individuals suffer from its complications throughout their lives and experience different physical and emotional disorders.Objectives:
The present study aimed to compare the effectiveness of acceptance and commitment therapy (ACT) and cognitive-behavioral therapy (CBT) in enhancing resiliency and quality of life among MS patients.Methods:
This randomized clinical trial was carried out on 30 MS patients referred to the Department of Neurology in Baqiyatallah Hospital (Tehran, Iran) during February 19 to September 1, 2017. The patients were randomly assigned to three groups: (1) ACT (n = 10, 8 sessions, 90-minute weekly sessions), (2) CBT (n = 10, 10 sessions, 90-minute weekly sessions), and (3) control group (n = 10, no sessions). The resilience and quality of life were measured in pre-test and post-test phases and 1.5 months after treatment using the Connor-Davidson Resilience and Multiple Sclerosis Impact Scales, respectively. Repeated measurement ANOVA and SPSS Software (version 24) were used in this study to analyze the collected data.Results:
The study sample consisted of 30 MS patients (mean age = 31.7 ± 5.7, 60% female and 57% married). The three groups were homogeneous in terms of demographic and baseline variables. The results demonstrated that both ACT and CBT had the same effectiveness in increasing resiliency (mean difference in CBT = 0.9 vs ACT = 0.8 (P = 0.882); CBT = 0.9 vs. Control = -1.4 (P = 0.004); ACT = 0.8 vs. Control = -1.4 (P = 0.0041)) and quality of life (mean difference in CBT = 2.9 vs ACT = 3.1 (P = 0.051); CBT = 2.9 vs. Control = 0.6 (P = 0.002); ACT = 3.1 vs. Control = 0.6 (P = 0.014)) among the MS patients so that the participants’ post-test and follow-up scores increased significantly compared to the pretest scores.Conclusions:
The present study results indicate that ACT and CBT can equally enhance resiliency and quality of life among MS patients.Keywords
Acceptance and Commitment Therapy Cognitive-Behavioral Therapy Multiple Sclerosis Psychological Resilience Quality of Life
1. Background
Multiple sclerosis (MS) is a demyelinating disease of the central nervous system and is one of the humans' most common neurological diseases. The most common period of onset is in youth (age between 20 and 40 years) (1, 2), and it is more common among men (3). The U.S. National MS Society announced that about 2.5 million persons worldwide have multiple sclerosis and that 200 persons are being added to this statistics weekly (4). According to previous studies, approximately half of MS patients had mental health issues (5). MS, with its debilitating, chronic, and unpredictable characteristics, poses many challenges in patients' lives. Concerning the age of disease onset, patients are obliged to reconsider their plans for life, family, and work and face recurrence of the disease and lack of autonomy, thereby arousing high anxiety and worry (6). In this disease, fatigue is one of the most common and debilitating symptoms causing dysfunction in work, social activity, and the daily performance of these patients (3, 7). The research findings suggest that tiredness is associated with a physical disability, and fatigue is associated with depression in these patients. Fatigue has a significant effect on the daily life of these patients, hinders physical activity, and interferes with their responsibility, work, and social roles as such it can decrease resiliency and satisfaction with the quality of life among these patients (7). About 50 - 60% of these patients suffer from depression (2, 8), which may result from poor sleep quality and poor nutrition or may be associated with a general sense of depression. This disorder must be diagnosed, and medication and psychological treatment should be used (9). Previous research indicates that in individuals with MS, psychological problems are a major source of disabilities, social harm, and poor quality of life (10). In general, MS, even in the early stages of the disease, has a significant effect on the quality of life among the affected. Further, several studies have revealed that the quality of life in MS patients is lower compared to the healthy population (11, 12). Because these patients have to deal with both stresses imposed by everyday life and the fluctuating and unpredictable symptoms of the disease, disease progression may interfere with work, family life, relationships, and social activities. Psychological interventions help these individuals cope with the above-mentioned challenges (13). Accordingly, the studies on new interventions should consider the psychological factors associated with the health of these patients and their physical injuries and disabilities (10). Since in chronic diseases, definitive and complete treatment of the disease symptoms is out of reach, an attempt is made to identify the modifiable factors affecting a person's disabilities to improve the quality of life by preventing, treating, and rehabilitating them at an appropriate time (14). The research results suggest an interrelationship between methods such as energy conservation, exercise, behavioral interactions, and psychological interventions with the symptoms of multiple sclerosis (15, 16). In recent decades, clinical psychology and positive psychology have focused on increasing happiness and the health and scientific investigations on the role of personal strengths and positive social systems to promote optimal health (17). Clinical manifestations of MS play a vital role in each individual’s adjustment to the disease. For this reason, psychotherapeutic interventions targeting these manifestations can help each person better adjust to the disease (18). Therapeutic protocols with an acceptable performance in solving behavioral problems in MS patients can be addressed in acceptance and commitment therapy (ACT) and cognitive-behavioral therapy (CBT) (9, 19, 20).
2. Objectives
According to previous research, of the treatments performed individually to decrease fatigue in MS patients, ACT and CBT have been most effective. Accordingly, these two treatments were selected to be compared in the present study. In other words, this study aimed to compare the effectiveness of ACT and CBT in enhancing resiliency and quality of life among MS Patients.
3. Methods
3.1. Study Design, Participants, and Sample Size, and Allocation
This randomized clinical trial was carried out on 30 MS patients referred to the Department of Neurology in Baqiyatallah Hospital (Tehran, Iran) during February 19 to September 1, 2017. The required sample size was estimated by the ANOVA formula (n1 = n2 = n3) with an effect size of 0.9 and a dropout rate of 10% (α = 5%, β = 10%), according to which 30 MS patients with scores a standard deviation above or below the mean score in CD-RISC and MSIS-29 were selected using the convenience sampling. They were then randomly assigned to three groups of 10 using randomized block methods.
3.2. Inclusion and Exclusion Criteria
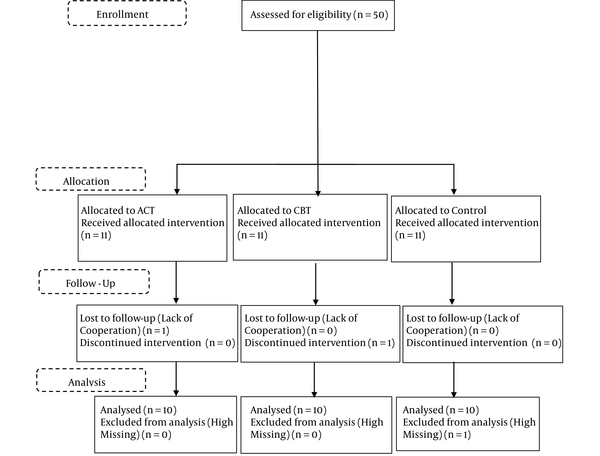
Inclusion criteria were MS disease aged 20 - 40 years old, literacy level above high school diploma, lack of other diseases, the ability to participate in regular training sessions, pregnancy or lactation, and conscious consent to participate in the research project. On the other hand, patients who were absent for more than two sessions and had high missing information in medical records were excluded (Figure 1).
Study Follow-up procedures
3.3. Intervention
The patients were randomly assigned to three groups: ACT, CBT, and control groups. The ACT and CBTs groups received 8 and 10 ACT and CBT therapy sessions, respectively, in the form of 90-minute weekly sessions. However, the control group received no psychological treatments. After the end of the treatments, the three groups were post-tested. Finally, after a 1.5-month follow-up, both treatment groups were again asked to answer the concerned questionnaires. A summary of ACT and CBT therapy protocols is provided in Table 1.
The Summary of ACT and CBT Therapy Protocols
| Session | Session Objectives | |
|---|---|---|
| ACT | CBT | |
| 1 | Introduction and basic concepts of treatment | Main concepts of cognitive-behavioral therapies |
| 2 | Discussion about values | How moods and emotions affect automatic behavior and thoughts |
| 3 | Acceptance and its definition | Cognitive techniques to challenge thoughts |
| 4 | Clarification of values | Identification of passive avoidance behaviors and disturbing behaviors and provision of assignment |
| 5 | Defusion | Identification of inefficient beliefs and cognitive errors |
| 6 | Commitment | Response to automatic thoughts |
| 7 | Satisfaction | Identification of intermediate beliefs |
| 8 | Maintenance of therapeutic benefits throughout life | Identification of fundamental beliefs |
| 9 | Relaxation training and deep breathing | |
| 10 | Review of all sessions and continuation of previous components as needed | |
3.4. Results and Questionnaires
In the present study, the following tools were used:
3.4.1. Demographic Questionnaire
A researcher-made personal profile questionnaire was prepared because of the influence of background factors and biological characteristics on the subjects' mood states. It included questions about personal information, date of birth, marital status, and disease duration.
3.4.2. Connor-Davidson Resilience Scale
Connor and Davidson developed the questionnaire by reviewing research resources on resilience (21). The psychometric characteristics of this scale have been studied in six groups, including the general population, patients admitted to the primary care department, psychiatric outpatients, individuals with generalized anxiety disorder, and two groups of patients with post-traumatic stress disorder. The scale developers believe that it can distinguish resilient people from non-resilient individuals in clinical and non-clinical groups. This 25-item questionnaire is scored on a Likert Scale, ranging from "completely incorrect" to "always correct." The maximum score is 100, and the minimum score is zero. Its cut-off point was set to be 80.4% for normal people. This scale was standardized in Iran by Keyhani et al. study (22). To determine the validity of this questionnaire, the correlation of each item with the total score of each category was first calculated, and then the factor analysis method was used. The correlation coefficients for each score with the total score, except for Item 3, ranged from 0.41 to 0.64. Afterward, the scale items were examined using factor analysis and the principal component analysis. Before extracting the factors based on the correlation matrix of the items, two indicators of KMO and Bartlett's test of sphericity were calculated. KMO was 0.87, and their value in Bartlett's test was 28.55 as such both indicators showed the adequacy of the evidence to perform the factor analysis. To determine the validity of the Connor-Davidson Resilience Scale (CD-RISC), Cronbach's alpha method was employed, and the validity coefficient was estimated to be 0.89 (22). In Samani et al.’s (23) study on a sample of university students, Cronbach’s alpha coefficient of this scale was 0.87 (23).
3.4.3. Multiple Sclerosis Impact Scale
In this study, a questionnaire wad used to assess the quality of life. Since the 1990s, several tools have been developed to measure the quality of life. One of the tools, specifically designed to evaluate the quality of life among MS patients, is the Multiple Sclerosis Impact Scale (MSIS-29) (24). It contains 29 questions, among which 20 items are related to the physical effect, and nine items are associated with the psychological effect of MS on the affected person. Five options (from 1 to 5) are considered for each question, and the sum of the individual's responses is converted to a scale of zero to 100, and a total score is then calculated. The higher these scores, the lower the patient's quality of life. The advantage of MSIS-29 is that it measures the physical and psychological impact of the disease from patient's perspectives. In two separate studies, the validity of this tool was investigated for various groups of patients, including hospitalized patients, rehabilitation patients, outpatients, and MS patients, indicating acceptable values (25). This questionnaire was translated into Persian and standardized by Ayatollahi et al. (26). The internal consistency of this scale (to show the quality of life among MS patients) with Cronbach’s alpha coefficient of > 0.70 indicates the acceptable internal consistency of the questions and the reliability of this scale.
The internal consistency of each of the physical and psychological scales ranges from 0.89 to 0.95. In the present study, to Cronbach’s alpha method was used determine the reliability of the MSIS-29. The result showed the coefficient of 0.72 for the whole questionnaire. This suggests the acceptable reliability of this questionnaire.
3.5. Ethical Considerations
All the participants in this research program were aware of the methodology used after a comprehensive explanation. The written informed consent was obtained from the participants after presenting enough explanations about the research objectives. The research's procedure was entirely consistent with the Ethics Committee of the Baqiyatallah University of Medical Sciences (code: IR.BMSU.REC.1395.308).
3.6. Statistical Analysis
To analyze the data, descriptive statistical methods (namely frequency, percentage, mean, standard deviation), Levene's test, Kolmogorov-Smirnov test, and repeated measurement ANOVA were used to calculate variability within and between the groups. Data analysis was performed using SPSS Software version 24. The significance level was set to be 0.05.
4. Results
The participants’ mean ages were 28.90 ± 5.06 years in the CBT group, 34.60 ± 4.47 years in the ACT group, and 31.80 ± 6.44 years in the control group (P = 0.07). In this study, 20, 30, and 40% of the participants in the ACT, CBT, and control groups were male, respectively (P = 0.621). The percentages of single and married subjects in each group were as follows: 50% and 50% in the CBT group, 40% and 60% in the ACT group, and 80% and 20% in the control group (P = 0.171). In the CBT group, the patients with the disease duration of 2 - 3 years had the highest frequency (50%), and the patients with the disease duration of > 8 years had the lowest frequency (10%). In the ACT group, the patients with the disease duration of 2 - 3 years had the highest frequency (50%), and the patients with the disease duration of > 8 years had the lowest frequency (10%). In the control group, the patients with the disease duration of 2 - 3 years had the highest frequency (50%), and the patients with a disease duration of > 8 years had the lowest frequency (10%) of the sample (P > 0.991). Table 2 displays the descriptive findings of the fatigue scores in the experimental and control groups in the pretest, post-test, and follow-up phases. The results demonstrate that both ACT and CBT are equally effective in increasing resiliency (mean difference in CBT = 0.9 vs ACT = 0.8, P = 0.882, CBT = 0.9 vs. Control = -1.4, P = 0.004, ACT = 0.8 vs. Control = -1.4, P = 0.0041) and quality of life (mean difference in CBT = 2.9 vs. ACT = 3.1, P = 0.051, CBT = 2.9 vs. Control = 0.6, P = 0.002, ACT = 3.1 vs. Control = 0.6, P = 0.014) among MS patients so that the participants' post-test and follow-up scores increased significantly compared to the pretest scores.
Mean and Standard Deviation of Resiliency and Quality of Life Scores in Experimental and Control Groups in Pretest, Post-test, and Follow-up Phases a
| Variables | Pre-test | Post-test | Follow-up | P-Value |
|---|---|---|---|---|
| Resiliency | ||||
| CBT | 5.30 ± 1.63 | 6.20 ± 1.22 | 6.10 ± 1.44 | 0.246 |
| ACT | 5.30 ± 1.56 | 6.10 ± 1.72 | 6.40 ± 1.35 | 0.005 |
| Control | 4.70 ± 1.33 | 3.30 ± 1.70 | 3.80 ± 1.40 | 0.051 |
| P-value | 0.60 | < 0.001 | < 0.001 | |
| Quality of life | ||||
| CBT | 6.70 ± 1.82 | 3.80 ± 2.25 | 3.70 ± 2.35 | 0.009 |
| ACT | 8.50 ± 1.26 | 5.40 ± 0.699 | 5.20 ± 0.789 | < 0.001 |
| Control | 8.00 ± 2.35 | 7.40 ± 2.22 | 7.00 ± 2.62 | 0.172 |
| P-value | 0.104 | 0.001 | 0.006 |
5. Discussion
The present study aimed to compare the effectiveness of ACT and CBT in enhancing resiliency and quality of life among MS patients. The research results revealed that ACT and CBT enhanced resiliency and quality of life among the concerned patients. At the end of the treatment and follow-up, the effects of ACT and CBT remained stable, and the scores of resiliency and quality of life were higher than those in the pretest phase. Various studies have revealed that resiliency increases mental health (27, 28). The findings demonstrate that resilient individuals can further tolerate adverse conditions, resulting in their psychological well-being. This is consistent with the results of other researchers, including Scandurra et al. (18), Fritz et al. (29), Halkitis et al. (30), Ribeiro et al. (31), Foster et al. (32)., Perreira et al. (33), Marselle et al. (34). Concerning the effectiveness of CBT, Golshani and Pirnia (35), in a study on chronic pain, concluded that CBT increased the resiliency of patients with chronic pain by changing their cognitions (36). This finding is consistent with those of the present study. By enhancing resiliency in patients with chronic pain, CBT allows them to deal with their disabilities and problems resulting from their disease more flexibly. On the other hand, treatments that can increase patients' control over their lives, emotions, behaviors, and thoughts and promote their ability to cope with their problems. The findings of this study are in line with those of other studies, including Wynne et al. (37), Feinstein et al. (38), Udell et al. (39), Ghorbani Amir et al. (40), regarding the role of acceptance in increasing the quality of life of patients with chronic pain (41, 42). Similarly, Joyce et al. (43) concluded that psychological flexibility and acceptance in this treatment could reduce the effects of chronic pain in individuals, improve their health in various aspects, promote the meaningful aspects of their lives, and increase their valuable activities to enhance the quality of life (44, 45).
According to Ryan et al. (46), the acceptance of thoughts as thoughts, feelings as feelings, and emotions as emotions, as they are- neither more nor less- weakens cognitive fusion and, at the same time, the acceptance of internal events when the person is not in conflict with his distress and turmoil, allows him to develop his behavioral repertoire. He can use the time obtained in this way to do his worthwhile activities and commit himself to a valuable and purposeful life (44, 45). In this regard, one of the most critical aspects of quality of life, ie, the spiritual aspect, which refers to the purpose and meaning that a person considers for life and the values pursued by him in his life, is improved. According to Feinstein et al. (38), individuals with greater experiential avoidance experience fewer positive emotions and life satisfaction and feel that their life is meaningless. However, since ACT aims to reduce experiential avoidance and increase psychological flexibility by accepting unpleasant, unavoidable, and distressing feelings such as anxiety, cultivating mindfulness to neutralize excessive conflict with cognitions, and identifying personal values associated with behavioral goals as such patients are encouraged to communicate with their experiences fully and with no resistance while moving toward their valuable goals and accepting them when they emerge with no judgment of whether they are right or wrong. This would increase the incentive to change despite the unavoidable obstacles and encourages individuals to strive to achieve valuable life goals. Finally, this would improve quality of life, especially in the psychological field (47).
The findings of studies by Jones and Hurrell (48) and Olason et al. (49) indicating the effectiveness of CBT and ACT in increasing the quality of life among patients with chronic pain and reducing pain is consistent with those of the present study (47). Moreover, the present findings are in line with those reported by Fisher et al. (50) and Urits et al. (51) regarding the effectiveness of ACT in promoting quality of life (47).
The findings on the effectiveness of CBT in enhancing quality of life among MS patients are consistent with the findings reported by Espie et al. (52), Riyahi et al. (53), Abdollahi et al. (54), Stapersma et al. (55), Kunzler et al. (56), and Qiu et al. (57). CBT effectively improves mental health by altering attitudes and reinforcing the logic and power to assess facts and increase assertiveness. CBT enhances a person's ability to adapt to stressful situations by improving his/her coping styles and thus reduces learning effective and efficient coping strategies for anxiety. Sun et al. (58) state that CBT decreases depression by focusing on self-efficacy and modifying thoughts as such it makes the depressed person more active and cohesive (47). With a positive effect on depression, CBT has also been the focus of numerous studies. Kalmbach et al. (59) also assume that self-esteem and self-concept increase when this treatment is adopted. Moreover, research on patients has revealed that CBT enhances social relationships and improves social support, thereby reducing depression, anxiety, and stress in patients. This would lead to improved quality of life among the affected patients (60). Finally, the small sample size and the selection of patients just from one center are the limitation of the present study.
5.1. Conclusions
The findings indicated that ACT and CBT can be equally effective in enhancing resiliency and quality of life among MS patients.
Acknowledgements
References
-
1.
Kenner M, Menon U, Elliott DG. Multiple Sclerosis as A Painful Disease. The Neurobiology of Multiple Sclerosis. International Review of Neurobiology; 2007. p. 303-21. https://doi.org/10.1016/s0074-7742(07)79013-x.
-
2.
Currie R. Spasticity: a common symptom of multiple sclerosis. Nurs Stand. 2001;15(33):47-52. quiz 54-5. [PubMed ID: 12216268]. https://doi.org/10.7748/ns2001.05.15.33.47.c3021.
-
3.
Ghaffari S, Ahmadi F, Nabavi M, Memarian R. [The effect of progressive muscle relaxation on depression, anxiety and stress in patients with multiple sclerosis]. Res Med Martyr Beheshti Univ Med Sci Health Ser. 2008;1(32):45. Persian.
-
4.
McCabe MP. Mood and self-esteem of persons with multiple sclerosis following an exacerbation. J Psychosom Res. 2005;59(3):161-6. [PubMed ID: 16198189]. https://doi.org/10.1016/j.jpsychores.2005.04.010.
-
5.
Steck B, Amsler F, Grether A, Dillier AS, Baldus C, Haagen M, et al. Mental health problems in children of somatically ill parents, e.g. multiple sclerosis. Eur Child Adolesc Psychiatry. 2007;16(3):199-207. [PubMed ID: 17136500]. https://doi.org/10.1007/s00787-006-0589-5.
-
6.
Landoni MG, Giordano MT, Guidetti GP. Group psychotherapy experiences for people with multiple sclerosis and psychological support for families. J Neurovirol. 2000;6(2). S168. [PubMed ID: 10871807].
-
7.
Schreurs KM, de Ridder DT, Bensing JM. Fatigue in multiple sclerosis: Reciprocal relationships with physical disabilities and depression. J Psychosom Res. 2002;53(3):775-81. https://doi.org/10.1016/s0022-3999(02)00326-4.
-
8.
Blake DJ, Bodine C. An overview of assistive technology for persons with multiple sclerosis. J Rehabil Res Dev. 2002;39(2):299. [PubMed ID: 12051472].
-
9.
Motl RW, Snook EM, Schapiro RT. Symptoms and physical activity behavior in individuals with multiple sclerosis. Res Nurs Health. 2008;31(5):466-75. [PubMed ID: 18286635]. https://doi.org/10.1002/nur.20274.
-
10.
Mitchell AJ, Kemp S, Benito-León J, Reuber M. The influence of cognitive impairment on health-related quality of life in neurological disease. Acta Neuropsychiatr. 2014;22(1):2-13. https://doi.org/10.1111/j.1601-5215.2009.00439.x.
-
11.
The Canadian Burden of Illness Study Group. Burden of illness of multiple sclerosis: Part I: Cost of illness. Can J Neurol Sci. 1998;25(1):23-30. [PubMed ID: 9532277]. https://doi.org/10.1017/s0317167100033448.
-
12.
Nedjat S, Montazeri A, Mohammad K, Majdzadeh R, Nabavi N, Nedjat F, et al. [Quality of life in multiple sclerosis compared to the healthy population in Tehran]. Iran J Epidemiology. 2006;2(3):19-24. Persian.
-
13.
Kalani N, Mosalanejad L, Abdolahifard S. The Effect of Group Hope Therapy Integrated with Mobile Learning on Hope and Perceived Stress Levels in MS Patients. Biosci Biotechnol Res Asia. 2015;12(3):1947-55. https://doi.org/10.13005/bbra/1861.
-
14.
Bahramian J, Zahrakar K, Rasouli M. [The effect of hope based group therapy approach on the severity of depression in multiple sclerosis patients]. Iran J Rehabil Res Nurs. 2014;1(1):12-22. Persian.
-
15.
Poser CM. The diagnosis and management of multiple sclerosis. Acta Neurol Scand. 2005;112(3):199-201. [PubMed ID: 16097966]. https://doi.org/10.1111/j.1600-0404.2005.00450.x.
-
16.
Merkelbach S, Sittinger H, Koenig J. Is there a differential impact of fatigue and physical disability on quality of life in multiple sclerosis? J Nerv Ment Dis. 2002;190(6):388-93. [PubMed ID: 12080209]. https://doi.org/10.1097/00005053-200206000-00007.
-
17.
Carr A. Positive psychology. New York, USA: Brunner Routledge; 2004.
-
18.
Scandurra C, Bochicchio V, Amodeo AL, Esposito C, Valerio P, Maldonato NM, et al. Internalized Transphobia, Resilience, and Mental Health: Applying the Psychological Mediation Framework to Italian Transgender Individuals. Int J Environ Res Public Health. 2018;15(3):508. [PubMed ID: 29534023]. [PubMed Central ID: PMC5877053]. https://doi.org/10.3390/ijerph15030508.
-
19.
Jopson NM, Moss-Morris R. The role of illness severity and illness representations in adjusting to multiple sclerosis. J Psychosom Res. 2003;54(6):503-11. https://doi.org/10.1016/s0022-3999(02)00455-5.
-
20.
Besharat MA, Pourhosein R, Rostami R, Bazzazian S. Perfectionism and fatigue in multiple sclerosis. Psychol Health. 2011;26(4):419-32. [PubMed ID: 20437295]. https://doi.org/10.1080/08870440903464228.
-
21.
Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76-82. [PubMed ID: 12964174]. https://doi.org/10.1002/da.10113.
-
22.
Keyhani M, Taghvaei D, Rajabi A, Amirpour B. [Internal consistency and confirmatory factor analysis of the Connor-Davidson Resilience Scale (CD-RISC) among nursing female]. Iran J Med Sci. 2015;14(10):857-65. Persian.
-
23.
Samani S, Jokar B, Sahragard N. [Effects of resilience on mental health and life satisfaction]. Iran J Psychiatry Clin Psychol. 2007;13(3):290-5. Persian.
-
24.
Hobart J, Lamping D, Fitzpatrick R, Riazi A, Thompson A. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain. 2001;124(Pt 5):962-73. [PubMed ID: 11335698]. https://doi.org/10.1093/brain/124.5.962.
-
25.
Riazi A, Hobart JC, Lamping DL, Fitzpatrick R, Thompson AJ. Multiple Sclerosis Impact Scale (MSIS-29): reliability and validity in hospital based samples. J Neurol Neurosurg Psychiatry. 2002;73(6):701-4. [PubMed ID: 12438473]. [PubMed Central ID: PMC1757371]. https://doi.org/10.1136/jnnp.73.6.701.
-
26.
Ayatollahi P, Nafissi S, Eshraghian M, Tarazi A. [Cross-Cultural Adaptation of the Multiple Sclerosis Impact Scale (MSIS-29) for Iranian MS Patients, Evaluation of Reliability and Validity]. Tehran Univ Med J. 2006;64(1):62-8. Persian.
-
27.
Beasley M, Thompson T, Davidson J. Resilience in response to life stress: the effects of coping style and cognitive hardiness. Pers Individ Differ. 2003;34(1):77-95. https://doi.org/10.1016/s0191-8869(02)00027-2.
-
28.
Inzlicht M, Aronson J, Good C, McKay L. A particular resiliency to threatening environments. J Exp Soc Psychol. 2006;42(3):323-36. https://doi.org/10.1016/j.jesp.2005.05.005.
-
29.
Fritz J, de Graaff AM, Caisley H, van Harmelen AL, Wilkinson PO. A Systematic Review of Amenable Resilience Factors That Moderate and/or Mediate the Relationship Between Childhood Adversity and Mental Health in Young People. Front Psychiatry. 2018;9:230. [PubMed ID: 29971021]. [PubMed Central ID: PMC6018532]. https://doi.org/10.3389/fpsyt.2018.00230.
-
30.
Halkitis PN, Krause KD, Vieira DL. Mental Health, Psychosocial Challenges and Resilience in Older Adults Living with HIV. Interdiscip Top Gerontol Geriatr. 2017;42:187-203. [PubMed ID: 27875833]. https://doi.org/10.1159/000448564.
-
31.
Ribeiro WS, Bauer A, Andrade MCR, York-Smith M, Pan PM, Pingani L, et al. Income inequality and mental illness-related morbidity and resilience: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4(7):554-62. https://doi.org/10.1016/s2215-0366(17)30159-1.
-
32.
Foster K, Roche M, Delgado C, Cuzzillo C, Giandinoto JA, Furness T. Resilience and mental health nursing: An integrative review of international literature. Int J Ment Health Nurs. 2019;28(1):71-85. [PubMed ID: 30294937]. https://doi.org/10.1111/inm.12548.
-
33.
Perreira KM, Marchante AN, Schwartz SJ, Isasi CR, Carnethon MR, Corliss HL, et al. Stress and Resilience: Key Correlates of Mental Health and Substance Use in the Hispanic Community Health Study of Latino Youth. J Immigr Minor Health. 2019;21(1):4-13. [PubMed ID: 29550906]. [PubMed Central ID: PMC6141349]. https://doi.org/10.1007/s10903-018-0724-7.
-
34.
Marselle MR, Warber SL, Irvine KN. Growing Resilience through Interaction with Nature: Can Group Walks in Nature Buffer the Effects of Stressful Life Events on Mental Health? Int J Environ Res Public Health. 2019;16(6):986. [PubMed ID: 30893850]. [PubMed Central ID: PMC6466337]. https://doi.org/10.3390/ijerph16060986.
-
35.
Golshani G, Pirnia B. Comparison of Mindfulness-Based Cognitive Therapy (MBCT) with Acceptance and Commitment Therapy (ACT) On the Severity of Fatigue, Improvement of Sleep Quality and Resilience in a Patient with Prostate Cancer: A Single-Case Experimental Study. Int J Cancer Manag. 2019;12(2). https://doi.org/10.5812/ijcm.88416.
-
36.
Ghasemi M, Hatami M, Hasani J. [The effectiveness of combination of Cognitive Behavior Therapy and Cognitive Emotion Regulation Strategies on mindfulness, resiliency and quality of life in patients with chronic pain]. J Health Psychol. 2016;5(18):69-86. Persian.
-
37.
Wynne B, McHugh L, Gao W, Keegan D, Byrne K, Rowan C, et al. Acceptance and Commitment Therapy Reduces Psychological Stress in Patients With Inflammatory Bowel Diseases. Gastroenterology. 2019;156(4):935-45. [PubMed ID: 30452919]. https://doi.org/10.1053/j.gastro.2018.11.030.
-
38.
Feinstein AB, Sturgeon JA, Bhandari RP, Yoon IA, Ross AC, Huestis SE, et al. Risk and Resilience in Pediatric Pain: The Roles of Parent and Adolescent Catastrophizing and Acceptance. Clin J Pain. 2018;34(12):1096-105. [PubMed ID: 30028367]. [PubMed Central ID: PMC6219922]. https://doi.org/10.1097/AJP.0000000000000639.
-
39.
Udell CJ, Ruddy JL, Procento PM. Effectiveness of Acceptance and Commitment Therapy in Increasing Resilience and Reducing Attrition of Injured US Navy Recruits. Mil Med. 2018;183(9-10):e603-11. [PubMed ID: 29518230]. https://doi.org/10.1093/milmed/usx109.
-
40.
Ghorbani Amir HA, Moradi O, Arefi M, Ahmadian H. The Effectiveness of Acceptance and Commitment Therapy on Cognitive-Emotional Regulation, Resilience, and Self-control Strategies in Divorced Women. Avicenna J Neuro Psycho. 2019:195-202. https://doi.org/10.32598/ajnpp.6.4.5.
-
41.
McCracken LM, Zhao-O'Brien J. General psychological acceptance and chronic pain: There is more to accept than the pain itself. Eur J Pain. 2010;14(2):170-5. [PubMed ID: 19349199]. https://doi.org/10.1016/j.ejpain.2009.03.004.
-
42.
Johnston M, Foster M, Shennan J, Starkey NJ, Johnson A. The effectiveness of an Acceptance and Commitment Therapy self-help intervention for chronic pain. Clin J Pain. 2010;26(5):393-402. [PubMed ID: 20473046]. https://doi.org/10.1097/AJP.0b013e3181cf59ce.
-
43.
Joyce S, Shand F, Bryant RA, Lal TJ, Harvey SB. Mindfulness-Based Resilience Training in the Workplace: Pilot Study of the Internet-Based Resilience@Work (RAW) Mindfulness Program. J Med Internet Res. 2018;20(9). e10326. [PubMed ID: 30206055]. [PubMed Central ID: PMC6231729]. https://doi.org/10.2196/10326.
-
44.
Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: a study of treatment effectiveness and process. J Consult Clin Psychol. 2008;76(3):397. [PubMed ID: 18540733]. https://doi.org/10.1037/0022-006X.76.3.397.
-
45.
McCracken LM, Velleman SC. Psychological flexibility in adults with chronic pain: a study of acceptance, mindfulness, and values-based action in primary care. Pain. 2010;148(1):141-7. [PubMed ID: 19945795]. https://doi.org/10.1016/j.pain.2009.10.034.
-
46.
Ryan AK, Pakenham KI, Burton NW. A pilot evaluation of a group acceptance and commitment therapy‐informed resilience training program for people with diabetes. Aust Psychol. 2020;55(3):196-207. https://doi.org/10.1111/ap.12429.
-
47.
Kashdan TB, Barrios V, Forsyth JP, Steger MF. Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behav Res Ther. 2006;44(9):1301-20. [PubMed ID: 16321362]. https://doi.org/10.1016/j.brat.2005.10.003.
-
48.
Jones S, Hurrell E. A single case experimental design: how do different psychological outcome measures capture the experience of a client undergoing CBT for chronic pain. Br J Pain. 2019;13(1):6-12. [PubMed ID: 30671233]. [PubMed Central ID: PMC6327351]. https://doi.org/10.1177/2049463718802873.
-
49.
Olason M, Andrason RH, Jonsdottir IH, Kristbergsdottir H, Jensen MP. Cognitive Behavioral Therapy for Depression and Anxiety in an Interdisciplinary Rehabilitation Program for Chronic Pain: a Randomized Controlled Trial with a 3-Year Follow-up. Int J Behav Med. 2018;25(1):55-66. [PubMed ID: 29094283]. https://doi.org/10.1007/s12529-017-9690-z.
-
50.
Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2019;4. CD011118. [PubMed ID: 30939227]. [PubMed Central ID: PMC6445568]. https://doi.org/10.1002/14651858.CD011118.pub3.
-
51.
Urits I, Hubble A, Peterson E, Orhurhu V, Ernst CA, Kaye AD, et al. An Update on Cognitive Therapy for the Management of Chronic Pain: a Comprehensive Review. Curr Pain Headache Rep. 2019;23(8). [PubMed ID: 31292747]. https://doi.org/10.1007/s11916-019-0794-9.
-
52.
Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, et al. Effect of Digital Cognitive Behavioral Therapy for Insomnia on Health, Psychological Well-being, and Sleep-Related Quality of Life: A Randomized Clinical Trial. JAMA Psychiatry. 2019;76(1):21-30. [PubMed ID: 30264137]. [PubMed Central ID: PMC6583463]. https://doi.org/10.1001/jamapsychiatry.2018.2745.
-
53.
Riyahi N, Ziaee M, Dastjerdi R. The Effects of Cognitive Behavioral Therapy on Quality of Life Among Patients with Hepatitis B. Mod Care J. 2018;15(3). https://doi.org/10.5812/modernc.82748.
-
54.
Abdollahi L, Mirghafourvand M, Babapour JK, Mohammadi M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: a randomized controlled clinical trial. J Psychosom Obstet Gynaecol. 2019;40(4):283-93. [PubMed ID: 30175648]. https://doi.org/10.1080/0167482X.2018.1502265.
-
55.
Stapersma L, van den Brink G, van der Ende J, Szigethy EM, Beukers R, Korpershoek TA, et al. Effectiveness of Disease-Specific Cognitive Behavioral Therapy on Anxiety, Depression, and Quality of Life in Youth With Inflammatory Bowel Disease: A Randomized Controlled Trial. J Pediatr Psychol. 2018;43(9):967-80. [PubMed ID: 29850915]. [PubMed Central ID: PMC6147749]. https://doi.org/10.1093/jpepsy/jsy029.
-
56.
Kunzler LS, Naves LA, Casulari LA. Cognitive-behavioral therapy improves the quality of life of patients with acromegaly. Pituitary. 2018;21(3):323-33. [PubMed ID: 29644512]. https://doi.org/10.1007/s11102-018-0887-1.
-
57.
Qiu H, Ren W, Yang Y, Zhu X, Mao G, Mao S, et al. Effects of cognitive behavioral therapy for depression on improving insomnia and quality of life in Chinese women with breast cancer: Results of a randomized, controlled, multicenter trial. Neuropsychiatr Dis Treat. 2018;14:2665. [PubMed ID: 30349264]. [PubMed Central ID: PMC6188154]. https://doi.org/10.2147/NDT.S171297.
-
58.
Sun H, Huang H, Ji S, Chen X, Xu Y, Zhu F, et al. The Efficacy of Cognitive Behavioral Therapy to Treat Depression and Anxiety and Improve Quality of Life Among Early-Stage Breast Cancer Patients. Integr Cancer Ther. 2019;18:1534735419829570. [PubMed ID: 30791739]. [PubMed Central ID: PMC6432673]. https://doi.org/10.1177/1534735419829573.
-
59.
Kalmbach DA, Cheng P, Arnedt JT, Cuamatzi-Castelan A, Atkinson RL, Fellman-Couture C, et al. Improving Daytime Functioning, Work Performance, and Quality of Life in Postmenopausal Women With Insomnia: Comparing Cognitive Behavioral Therapy for Insomnia, Sleep Restriction Therapy, and Sleep Hygiene Education. J Clin Sleep Med. 2019;15(7):999-1010. [PubMed ID: 31383238]. [PubMed Central ID: PMC6622507]. https://doi.org/10.5664/jcsm.7882.
-
60.
Hassanzadeh R, Abedini M. [Effectuality of cognitive-behavioral therapy on the life expectancy of patients with multiple sclerosis]. J Mazandaran Univ Med Sci. 2012;22(93):58-65. Persian.