Abstract
Context:
Breast cancer in women can cause sexual dissatisfaction and hinder sexual function as a result of treatment processes. Several studies have been conducted on the impact of therapeutic-supportive interventions on sexual satisfaction and performance; nonetheless, contradictory results have been reported. The aim of this systematic review and meta-analysis was to review the effects of therapeutic-supportive interventions on sexual satisfaction and function in patients with breast cancer. In this study, a quality assessment of published articles was also conducted.Evidence Acquisition:
In this systematic review, electronic databases, including Google Scholar,Web of Sciences, Science Direct, Cochrane Library, ProQuest, Scopus, and PubMed (including Medline), were searched to retrieve articles published between 1990 and 2016.The articles were screened with regard to breast cancer in 4 stages. Articles, which focused on therapeutic-supportive interventions and sexual satisfaction and function of patients with breast cancer, were included in the study. According to the heterogeneity index between articles (Cochran’s Q and I square tests), the random effects model, inverse variance weighting method, and standardized Cohen’s statistics were applied to estimate the mean differences in sexual function and satisfaction.Results:
Six articles studied the effects of therapeutic-supportive interventions on sexual satisfaction, while 8 articles assessed the effects of these interventions on sexual function in patients with breast cancer. The standardized mean difference of sexual satisfaction between the intervention and control groups was -0.03 (95% CI, -0.55 - 0.49). In addition, the standardized mean difference of sexual function between the intervention and control groups was 0.14 (95% CI, -0.28 - 0.57).Conclusions:
The results showed that therapeutic-supportive interventions had no impact on the sexual satisfaction and function of patients with breast cancer.Keywords
Breast Cancer Sexual Function Sexual Satisfaction Therapeutic-Supportive Interventions
1. Context
Breast cancer is the most common cancer among women around the world (1-4) and is considered the second leading cause of mortality worldwide. Over the past 13 years, various efforts have been made to improve early detection, treatment, and alleviation of complications (5, 6). As a result of these efforts, the relative 5-year survival of patients from high-, middle-, and low-income countries has reached 80% - 90%, 60%, and 40%, respectively (7). However, diagnosis of breast cancer (8), chemotherapy (9), mastectomy (10), surgery (6, 9), radiotherapy (6), and mental problems (11) have many negative consequences for breast cancer patients.
Physical problems can lead to sexual dysfunction and dissatisfaction. Sexual function is defined as one’s anatomical and physiological capacity to engage in sexual activities. The components of sexual physiology include the sexual response cycle, human anatomy, and changes in the level of sex hormones and sexual life cycles as components of sexual anatomy (12), which are associated with softening of the vagina, frequency of sexual activity, and breast tenderness. Prior to the diagnosis and treatment of breast cancer, sexual dysfunction was not reported in 91.5% of patients (6). The prevalence of sexual complications was estimated at 30% - 100% using previous treatments and included decreased libido, sexual arousal, and vaginal lubrication, followed by dyspareunia and vaginal dryness (6, 13-15).
On the other hand, sexual satisfaction refers to one’s feelings about her body, sexual satisfaction, and even body image, and femininity (16). Since breast cancer causes common problems for couples (17), and sexual dissatisfaction compromises the marital life (9), healthcare providers, with the use of therapeutic-supportive interventions, can reduce sexual problems. In fact, support groups can help reduce stress and increase awareness about breast cancer, diet, healthy behaviors, and coping strategies. It has been reported that women who receive supportive care experience lower levels of distress (18). In a study on the effects of group counseling on the quality of sexual life, patients reported improvements in the quality of life in terms of sexuality, knowledge, and anxiety (15). However, an interventional study showed that sexual function and pleasure reduced within a week after the intervention, as quality of life and fatigue were mainly affected in patients (19).
There are contradictory results in previous studies regarding the effects of therapeutic-supportive interventions on the sexual satisfaction and function of women with breast cancer (20, 21). Systematic reviews can overcome the contradictions and ambiguities in the findings of original studies (22, 23). These studies can facilitate an accurate analysis of the impact of therapeutic-supportive interventions on sexual satisfaction and function. Therefore, by retrieving and investigating the literature, the present systematic review aimed to study the effects of therapeutic-supportive interventions on the sexual satisfaction and function of patients with breast cancer.
2. Evidence Acquisition
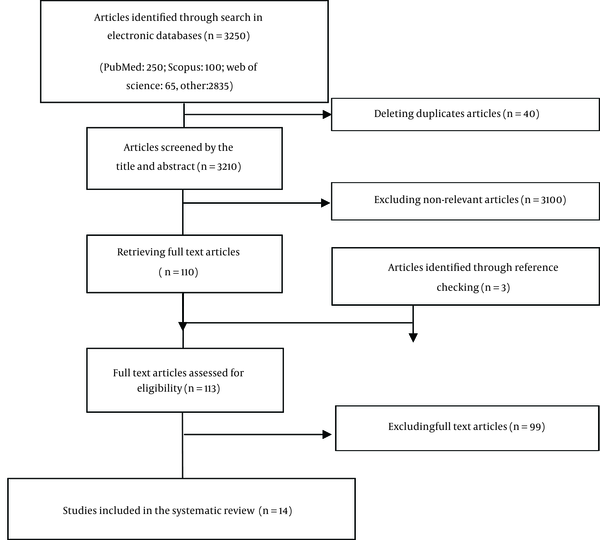
The keywords in the search process included “breast cancer”, “interventions”, “support programs”, “cognitive behavioral therapy”, “group counseling”, “Internet-based interventions”, “telephone intervention”, “sexual satisfaction”, and “sexual function”. The following steps were taken to select the articles and conduct the systematic review and meta-analysis: 1) identification of the research question; 2) search in databases for retrieving articles; 3) selection of articles; and 4) presentation of data in charts and tables (17, 24) (Figure 1).
The Search Process in the Present Study
2.1. Identification of the Research Question and PICOD
The research questions were as follows:
- What are the therapeutic-supportive interventions for sexual function in patients with breast cancer?
- What are the therapeutic-supportive interventions for sexual satisfaction in patients with breast cancer?
PICOD refers to patients with breast cancer (P), therapeutic-supportive interventions (C), effect of intervention (O), and meta-analysis (D).
2. 2. Search in Databases for Retrieving Articles
Electronic databases, including Google Scholar, Web of Sciences, Science Direct, Cochrane library, ProQuest, Scopus, and PubMed (including Medline) were searched for articles, using Medical Subject Headings (MeSH) and combinations of keywords, including “breast cancer”, “breast neoplasm”, “tumor”, “intervention program”, “education”, “sexual function”, “sexual dysfunction”, and “sexual satisfaction” with Boolean operators. The articles were published between 1990 and 2016. Also, a manual search was conducted to find articles on supportive interventions, cognitive behavioral therapy, Internet-based interventions, telephone interventions, sexual education, and peer support.
2.3. Selection of Articles
The articles were screened with regard to breast cancer in 4 stages: 1) screening for the selection of titles; 2) removing duplicate papers; 3) comparison of abstracts with the study objectives; and 4) appraisal of the full-texts of articles.
2.3.1. Inclusion Criteria
Articles, which focused on therapeutic-supportive interventions, as well as sexual satisfaction and function in patients with breast cancer, were included in the study.
2.3.2. Exclusion Criteria
Case-control and cross-sectional studies, along with articles focusing on other types of cancer or variables other than sexual satisfaction and function, were excluded from the analysis.
2.4. Quality Assessment
Two authors evaluated the studies, based on the Jadad quality assessment scale from a previous systematic review (25, 26). The checklist consisted of 3 direct items, which focused on random allocation, blinding, and withdrawal. In addition, the checklist incorporated 8 indirect items: 1) explaining the study objectives; 2) describing the findings; 3) describing the inclusion and exclusion criteria; 4) identifying the sample size; 5) explaining the intervention; 6) including at least 1 control group; 7) considering the intervention effects; and 8) explaining the statistical analysis.
Various studies used the direct items, while some used both direct and indirect items. Most articles used the direct items, as they have been used in all areas of applied sciences. In this study, for surveying all items, we used both direct and indirect items. The scoring system ranged from 0 to 2 for direct items and 0 to 1 for the indirect ones. Regarding the direct items, articles were scored 2 if considered eligible in comparison with the total items; they were scored 1 or 0 if they showed average or zero quality, respectively. On the other hand, the indirect items were scored 1 or 0. Finally, the score of items was calculated (score ≥ 3, good quality).
2.5. Data Extraction
The characteristics of each study, including title, authors, date and place of study, sample size, sampling method, age, type of intervention, and effect of intervention (mean and standard deviation), were determined (Tables 1 - 3).
Characteristics of Studies Included in the Systematic Review
| Authors | Publication Year | Country | Sample Size | Type of Intervention | Data Collection Tool | Results |
|---|---|---|---|---|---|---|
| Bjorneklett | 2013 | Sweden | 362 | Support group | EORTC QLQ-C30; QLQ-BR23; HAD -FQ | The support intervention significantly improved cognitive function. |
| Rowland | 2009 | USA | 155 | Psychoeducational group | CES-D; RDAS; CARES | The intervention group was more likely to report improvement in relationship adjustment and communication, as well as increased sexual satisfaction, compared to the controls. |
| Heravi | 2006 | Iran | 144 | Group counseling | QLQ-BR23 | Counseling improved sexual satisfaction and function. |
| Schover | 2006 | USA | 48 | Peer counseling | FACIT-Sp; FSFI; demographic and medical history; BSI-18 | The program had positive effects. |
| Lotfi Kashani | 2014 | Iran | 25 | Sexual skills | ASEX | Sexual skill training improved sexual function and enhanced sexual satisfaction among patients with breast cancer. |
| Schover | 2011 | USA | 291 184 = 12-month follow-up | Peer counseling | FACIT-Sp; A-DAS; BSI-18; FSFI | Sexually active women had improved sexual function in the 6-month follow-up, but not after 1 year. |
| Young Jun | 2011 | Korea | 45 | Sexual life reframing program | CARES; sexual function (sexual interest, dysfunction, and satisfaction) | The sexual life reframing program was effective in increasing sexual satisfaction among breast cancer survivors. |
| Shariati | 2010 | Iran | 25 | Benson’s relaxation intervention | Demographic questionnaire; BR23-C; quality of life questionnaire | The intervention improved sexual satisfaction and function. |
| Salonen | 2009 | Finland | 228 | Telephone intervention | QLI-CV; EORTC QLQ-BR23 | The patients’ experiences showed that the telephone intervention was helpful. |
Characteristics of the Excluded Studies
| Authors/Publication Year | Article Title | Cause of Exclusion |
|---|---|---|
| Duijts, 2009 (27) | Cognitive behavioral therapy and physical exercise for climacteric symptoms in breast cancer patients experiencing treatment-induced menopause | Unrelated to sexual function |
| Hummel, 2015 (13) | Internet-based cognitive behavioral therapy for sexual dysfunction in women treated for breast cancer | Unrelated to sexual function |
| Hoey, 2008 (28) | Systematic review of peer-support programs for people with cancer | Systematic review |
| Brotto, 2008 (29) | A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer | Gynecologic cancer |
| Morone, 2014 (30) | Effects of a multidisciplinary educational rehabilitative intervention in breast cancer survivors: The role of body image on quality of life outcomes | Unrelated to sexual function |
| Malary, 2015 (31) | Biopsychosocial determinants of hypoactive sexual desire in women | Unrelated to sexual function |
| Pomery, 2015 (32) | Skills, knowledge, and attributes of support group leaders | Systematic review |
| Alpers, 2005 (33) | Evaluation of computerized text analysis in an Internet breast cancer support group | Unrelated to sexual function |
| Rezaei, 2016 (17) | Factors influencing body image in women with breast cancer | Narrative review |
The Demographic Characteristics of Patients in Studies Included in the Systematic Review
| First Author | Publication Year | Type of Outcome | Sample Size | Intervention Groupa | Control Groupa | |
|---|---|---|---|---|---|---|
| Intervention Group | Control Group | |||||
| Bjorneklett | 2013 | Sexual satisfaction | 181 | 181 | 64.4 ± 25.3 | 67.7 ± 26.5 |
| Lotfi | 2014 | Sexual satisfaction | 24 | 24 | 3.58 ± 0.997 | 4.25 ± 0.621 |
| Rowland | 2009 | Sexual satisfaction | 57 | 98 | 4.8 ± 1.1 | 4.4 ± 0.1 |
| Heravi Karimoui | 2006 | Sexual satisfaction | 51 | 63 | 12.19 ± 16.15 | 7.72 ± 4.14 |
| Schover | 2006 | Sexual satisfaction | 41 | 41 | 3.26 ± 1.88 | 5.04 ± 1.19 |
| Eun-Young | 2011 | Sexual satisfaction | 22 | 23 | 47.16 ± 9.49 | 38.96 ± 10.02 |
| Schover | 2006 | Sexual function | 47 | 47 | 17.85 ± 11.57 | 30.75 ± 4.8 |
| Schover | 2011 | Sexual function | 184 | 184 | 18.1 ± 10.7 | 18.2 ± 10.7 |
| Lotfi | 2014 | Sexual function | 35 | 35 | 42.41 ± 14.178 | 34.56 ± 11.803 |
| Eun-Young | 2011 | Sexual function | 22 | 23 | 1.37 ± 0.87 | 1.53 ± 0.73 |
| Shariati | 2010 | Sexual function | 25 | 25 | 24 ± 20.4 | 17.3 ± 17 |
| Salonen | 2009 | Sexual function | 120 | 108 | 29 ± 26 | 24 ± 22 |
| Bjorneklett | 2013 | Sexual function | 181 | 181 | 24.2 ± 23.9 | 19.9 ± 23 |
| HeraviKarimoui | 2006 | Sexual function | 51 | 63 | 25.19 ± 11.78 | 8.52 ± 11.48 |
2.6. Data Synthesis
Data analysis was carried out using Stata version 11. The heterogeneity index for the studies was calculated using Cochran’s Q and I square tests. According to the heterogeneity index among articles, the random effects model, inverse variance weighting method, and standardized Cohen statistics were applied to determine the differences in the mean values of sexual function and satisfaction.
The point-standardized difference in the mean score of sexual satisfaction and function was estimated with 95% confidence interval (forest plots). In the graph, the size of cubic and surrounding lines indicated the weight of each article and 95% CI, respectively. Also, the Egger’s test was used to assess the publication bias. P value < 0.01 was considered statistically significant.
3. Results
In different stages of the study, 40 out of 3,250 articles were removed due to duplication. Also, 3100 other articles were excluded due to the following reasons: 1) being unrelated to the study objectives; and 2) performing no intervention affecting the variables. In the third stage, 110 studies were excluded, and 3 articles were found, based on the reference check. In the fourth stage, the full-text of 113 articles was read, and 99 articles were excluded. Finally, 14 articles were included in our systematic review and meta-analysis.
The articles, published between 2006 and 2016, were classified into “sexual satisfaction” and “sexual function”. The samples were collected from women with breast cancer (age range, 18 - 65 years) during 2011 - 2013. Regarding sexual satisfaction, the intervention and control groups included 376 and 430 subjects, respectively. Among 6 articles related to sexual satisfaction, two had a quasi-experimental design, while 4 articles were randomized controlled trials. The randomization method was applied in all studies for the allocation of patients to the control and intervention groups. Sexual interventions for sexual satisfaction consisted of group counseling, peer support, group support, skill training programs, and psychological sex education. The interventions continued for 1 to 12 weeks.
Regarding sexual function, the intervention and control groups consisted of 665 and 666 women, respectively. Among 8 articles related to sexual function, four had a quasi-experimental design, while 4 articles had a randomized controlled design. Also, the randomization method was used for the allocation of samples to the groups. The intervention programs consisted of group counseling, peer group, relaxation, telephone support, group support, skill training programs, and sex education programs. Also, the sexual function questionnaires were used for data collection in all studies.
Among the selected articles, six examined the effects of educational interventions on sexual satisfaction among women with breast cancer. The total sample size included 376 and 430 women in the intervention and control groups, respectively. In 3 studies, the mean of changes in sexual satisfaction was higher in the intervention group, compared to the controls, and the difference was statistically significant.
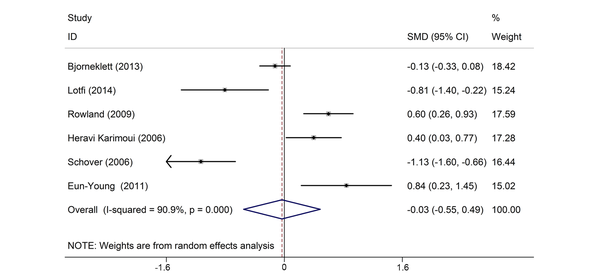
There were heterogeneities between the results of retrieved articles (I-square, 90.9%; Q, 55.2; P < 0.05). Therefore, the random effects model was used to estimate the standardized mean differences of sexual satisfaction scores. The standardized mean difference of sexual satisfaction between the intervention and control groups was -0.03 (95% CI, -0.55 - 0.49). In fact, the score of sexual satisfaction in the intervention group was -0.03 lower than that of the control group; however, the difference was not statistically significant (Figure 2).
The Standardized Mean Difference of Sexual Satisfaction Between the Intervention and Control Groups
Eight studies examined the effect of education on sexual function in women with breast cancer. The population of the intervention and control groups included 665 and 666 women, respectively. Five studies reported greater mean changes in sexual function in the intervention group; nonetheless, only 1 study showed a significance change.
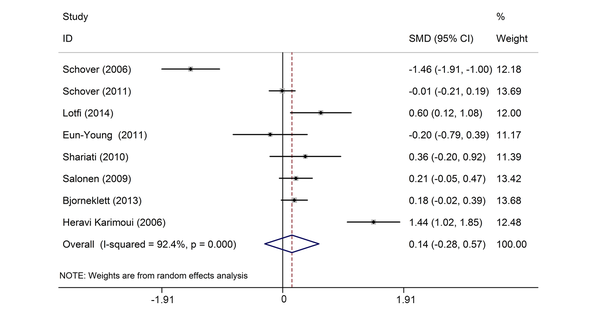
There were heterogeneities between the studies (I-square, 92.4%; Q, 92.6; P < 0.01). Therefore, the random effects model was used to estimate the standardized mean differences of sexual function scores. The standardized mean difference of sexual function score was 0.14 between the intervention and control groups (95% CI, -0.28 - 0.57). Accordingly, the score of sexual function in the intervention group was 0.14 higher than that of the control group; the difference was not statistically significant (Figure 3).
The Standardized Mean Difference of Sexual Function Scores Between the Intervention and Control Groups
In addition, quality assessment of articles on sexual function and satisfaction (Tables 4 and 5) showed that 62.5% and 66.66% of articles used random methods, while 12.5% and 16.67% focused on description of this approach, respectively. The greatest shortcomings of the articles were related to the double-blind design and full description of sample loss. In fact, 25% and 33.33% of studies related to sexual performance and satisfaction presented a full description of the cause of sample loss, respectively.
Quality Assessment of Articles Related to Sexual Function
| Items | Score | No. (%) |
|---|---|---|
| Direct Items | ||
| 1. Was the study described as randomized? | 0 | 2 (25) |
| 1 | 5 (62.5) | |
| 2 | 1 (12.5) | |
| 2. Was the study described as double-blind? | 0 | 8 (100) |
| 1 | - | |
| 2 | - | |
| 3. Was there a description of withdrawals and dropouts? | 0 | 6 (75) |
| 0.5 | - | |
| 1 | 2 (25) | |
| Indirect items | ||
| 4. Were the study objectives defined? | 0 | - |
| 1 | 8 (100) | |
| 5. Were the outcome measures defined clearly? | 0 | - |
| 1 | 8 (100) | |
| 6. Was there a clear description of the inclusion and exclusion criteria? | 0 | - |
| 1 | 8 (100) | |
| 7. Was the sample size justified? | 0 | - |
| 1 | 8 (100) | |
| 8. Was there a clear description of the interventions? | 0 | 1 (12.5) |
| 1 | 7 (87.5) | |
| 9. Was there at least 1 control (comparison) group? | 0 | 1 (12.5) |
| 1 | 7 (87.5) | |
| 10. Was the assessment method of adverse effects described? | 0 | 8 (100) |
| 1 | - | |
| 11. Were the methods of statistical analysis described? | 0 | 1 (12.5) |
| 1 | 7 (87.5) | |
Quality Assessment of Articles Related to Sexual Satisfaction
| Items | Score | No. (%) |
|---|---|---|
| Direct Items | ||
| 1. Was the study described as randomized? | 0 | 1 (16.67) |
| 1 | 4 (66.66) | |
| 2 | 1 (16.67) | |
| 2. Was the study described as double-blind? | 0 | 6 (100) |
| 1 | - | |
| 2 | - | |
| 3. Was there a description of withdrawals and drop outs? | 0 | 4 (66.67) |
| 0.5 | - | |
| 1 | 2 (33.33) | |
| Indirect items | ||
| 4. Were the study objectives defined? | 0 | - |
| 1 | 6 (100) | |
| 5. Were the outcome measures defined clearly? | 0 | - |
| 1 | 6 (100) | |
| 6. Was there a clear description of the inclusion and exclusion criteria? | 0 | 1 (16.67) |
| 1 | 5 (83.33) | |
| 7. Was the sample size justified? | 0 | 1 (16.67) |
| 1 | 5 (83.33) | |
| 8. Was there a clear description of the interventions? | 0 | 1 (16.67) |
| 1 | 5 (83.33) | |
| 9. Was there at least 1 control (comparison) group? | 0 | - |
| 1 | 6 (100) | |
| 10. Was the assessment method of adverse effects described? | 0 | 6 (100) |
| 1 | - | |
| 11. Were the methods of statistical analysis described? | 0 | - |
| 1 | 6 (100) | |
The survey of 8 indirect items showed that 100% of articles related to sexual function explained the study objectives, results, inclusion and exclusion criteria, and sample size, which are strengths of these studies. Also, 100% of articles related to sexual satisfaction explained the study objectives and results and included at least 1 control group with complete scores.
4. Discussion
This meta-analysis aimed to investigate the effects of therapeutic-supportive interventions on the sexual satisfaction and function of patients with breast cancer in a systematic review. The findings showed that the scores of sexual function and satisfaction were 0.14 and -0.03, respectively.
Two studies from Korea and Sweden assessed the effects of interventional programs in patients with breast cancer (19, 21). In the study from Sweden, among 382 patients with breast cancer, 191 cases participated in a supportive intervention for 1 week. The intervention included presentation of information on the etiology of cancer, risk factors, physical and psychological consequences, and coping strategies, using lectures and group discussions. Also, physical exercises, such as relaxation, Qigong, nonverbal communication, and art/dance therapy, were included in the intervention. Data were collected before the intervention and 2, 6, and 12 months after the intervention.
In the mentioned study, quality of life dimensions, such as bodily pain, physical function, and sexual satisfaction, were measured, using the short-form health survey (SF-36). It was reported that sexual function and satisfaction reduced after the intervention. Therefore, the intervention influenced the patients’ quality of life and fatigue (19). Moreover, the study from Korea focused on education about sexual issues. The findings showed an improvement in the sexual satisfaction of 22 patients (P < 0.01) (21).
Moreover, two studies from Iran and the United States used group and peer counseling (15, 34). In the study from Iran, group discussion involved 114 patients with breast cancer, 51 of whom participated in group discussions (4 - 5 patients per group). Five group discussions were held for 1.5 hours and focused on disease education, knowledge of treatments, consequences of chemotherapy, and effects of intervention on sexual organs. Patients were asked to apply their learning to their daily life over 3 months. The results showed an improvement in sexual satisfaction and function (P < 0.001) (15).
In the study from the United States, 48 patients participated in the peer-counseling intervention about menopause and cancer (including hot flashes, vaginal dryness, urinary incontinence, and prevention of fungal urinary tract infections), breast cancer and sexual issues (talking to the partner, resuming sex after cancer, and dyspareunia), and cancer and family (reproductive and breast cancer, family history of breast cancer, genetic counseling, and screening). The intervention was held in 3 sessions (30 - 60 minutes per session). The findings showed improvements in the knowledge of sexual function and satisfaction, stress, and menopause, based on the scores of the sexual function questionnaire. The SPIRIT program could increase the knowledge of patients (P < 0.001).
In another study from the United States, the psychoeducational group intervention was implemented with a focus on understanding sexuality and intimacy in patients with breast cancer. The inclusion criteria were diagnosis of breast cancer (stage 0 - II), established diagnosis for 1 - 5 years, tamoxifen treatment, no history of other diseases or skin involvement, and proficiency in English language. Patients from different age groups were included in this study. Among 284 subjects, 57 and 98 were assigned to the intervention and control groups, respectively; the duration of intervention was 6 weeks. Four months after the intervention, the data collection tool was applied. The intervention focused on lectures about breast and sexuality for cancer patients and survivors. Based on the findings, after the intervention, the patients felt comfortable about being naked and touched during sexual activities; in other words, patients reached sexual satisfaction and comfort (35).
Moreover, in an interventional study from Iran, 35 patients with breast cancer, aged below 60 years, received education on sexual skills for 12 sessions (90 minutes per session). The findings showed an improvement in the sexual satisfaction of the intervention group (0.997 ± 5.25), compared with the controls (0.621 ± 4.25). Also, similar improvements were reported in the sexual function of both groups (intervention, 1.115 ± 15.83 vs. control, 1.055 ± 20.25) (20).
In conclusion, the present study investigated the effects of therapeutic-supportive interventions on the sexual function and satisfaction of patients with breast cancer. Based on the findings, age, social status, and economic condition affect sexual issues. Also, perceived differences and marital discords influence sexual problems. However, the findings of this study did not show any significant differences between the type of intervention and sexual satisfaction and function. A probable reason is the type of counseling intervention and supportive method. Lack of homogeneity in the applied tools and scales can be also effective. Furthermore, the social context, culture, and partner support may affect sexual issues in women. Overall, systematic analysis of the literature can be helpful in knowledge production, improvement of shortcomings and defects, and design of optimal plans.
4.1. Strengths
In this systematic review and meta-analysis, the authors incorporated all interventions influencing sexual function and satisfaction in patients with cancer.
4.2. Limitations
The limitations of this study include focus on 2 languages and lack of access to the full-text of some abstracts.
Acknowledgements
References
-
1.
Jankowska M. Sexual functioning in young women in the context of breast cancer treatment. Rep Pract Oncol Radiother. 2013;18(4):193-200. [PubMed ID: 24416553]. https://doi.org/10.1016/j.rpor.2013.04.032.
-
2.
Shariati AA, Salehi M, Ansari M, Latifi SM. [Survey the effect of Benson relaxation intervention on quality of life (QOL) in breast cancer patients undergoing chemotherapy]. Jundishapur Sci Med J. 2011;9(6):625-32. Persian.
-
3.
Khalili R, Bagheri-Nesami M, Janbabai G, Nikkhah A. Lifestyle in Iranian Patients with Breast Cancer. J Clin Diagn Res. 2015;9(7):XC06-9. [PubMed ID: 26393190]. https://doi.org/10.7860/JCDR/2015/13954.6233.
-
4.
Haghshenas MR, Mousavi T, Moosazadeh M, Afshari M. Human papillomavirus and breast cancer in Iran: a meta- analysis. Iran J Basic Med Sci. 2016;19(3):231-7. [PubMed ID: 27114791].
-
5.
Gilbert E, Ussher JM, Perz J. Sexuality after breast cancer: a review. Maturitas. 2010;66(4):397-407. [PubMed ID: 20439140]. https://doi.org/10.1016/j.maturitas.2010.03.027.
-
6.
Sbitti Y, Kadiri H, Essaidi I, Fadoukhair Z, Kharmoun S, Slimani K, et al. Breast cancer treatment and sexual dysfunction: Moroccan women's perception. BMC Womens Health. 2011;11:29. [PubMed ID: 21668971]. https://doi.org/10.1186/1472-6874-11-29.
-
7.
Ganz PA, Yip CH, Gralow JR, Distelhorst SR, Albain KS, Andersen BL, et al. Supportive care after curative treatment for breast cancer (survivorship care): resource allocations in low- and middle-income countries. A Breast Health Global Initiative 2013 consensus statement. Breast. 2013;22(5):606-15. [PubMed ID: 24007941]. https://doi.org/10.1016/j.breast.2013.07.049.
-
8.
Aguilar Cordero MJ, Mur Villar N, Neri Sanchez M, Pimentel-Ramirez ML, Garcia-Rillo A, Gomez Valverde E. Breast cancer and body image as a prognostic factor of depression: a case study in Mexico City. Nutr Hosp. 2014;31(1):371-9. [PubMed ID: 25561132]. https://doi.org/10.3305/nh.2015.31.1.7863.
-
9.
Kashani FL, Vaziri S, Akbari ME, Jamshidi Far Z, Smaeeli Far N. Sexual Skills, Sexual Satisfaction and Body Image in Women with Breast Cancer. Proc Soc Behav Sci. 2014;159:206-13. https://doi.org/10.1016/j.sbspro.2014.12.358.
-
10.
Brandberg Y, Sandelin K, Erikson S, Jurell G, Liljegren A, Lindblom A, et al. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: a prospective 1-year follow-up study. J Clin Oncol. 2008;26(24):3943-9. [PubMed ID: 18711183]. https://doi.org/10.1200/JCO.2007.13.9568.
-
11.
Alicikus ZA, Gorken IB, Sen RC, Kentli S, Kinay M, Alanyali H, et al. Psychosexual and body image aspects of quality of life in Turkish breast cancer patients: a comparison of breast conserving treatment and mastectomy. Tumori. 2009;95(2):212-8. [PubMed ID: 19579868].
-
12.
Chow KM, H. Chan CW, Chan JCY. Effects of psychoeducational interventions on sexual functioning, quality of life and psychological outcomes in patients with gynaecological cancer: A systematic review. JBI Database System Rev Implement Rep. 2012;10(58):4077-164. https://doi.org/10.11124/jbisrir-2012-406.
-
13.
Hummel SB, van Lankveld JJ, Oldenburg HS, Hahn DE, Broomans E, Aaronson NK. Internet-based cognitive behavioral therapy for sexual dysfunctions in women treated for breast cancer: design of a multicenter, randomized controlled trial. BMC Cancer. 2015;15:321. [PubMed ID: 25927495]. https://doi.org/10.1186/s12885-015-1320-z.
-
14.
Molavi A, Hekmat K, Afshari P, Hoseini M. [Evaluation of couples' sexual function and satisfaction after mastectomy]. Iran J Obstetr Gynecol Infertil. 2015;17(134):17-24. Persian.
-
15.
Heravi Karimovi M, Pourdehqan M, Jadid Milani M, Foroutan SK, Aieen F. [Study of the effects of group counseling on quality of sexual life of patients with breast cancer under chemotherapy at Imam Khomeini Hospital]. J Mazandaran Univ Med Sci. 2006;16(54):43-51. Persian.
-
16.
Naghipoor L, Bahram Abadi Zarea M, Taghiloo S, Heydari H. [Sexual satisfaction, body image and quality of life: A comparison of unaffected women and women with breast cancer in two groups: Mastectomy surgery and surgery-preserving breast]. Q Womens Stud. 2013;4(33):41-62. Persian.
-
17.
Rezaei M, Elyasi F, Janbabai G, Moosazadeh M, Hamzehgardeshi Z. Factors Influencing Body Image in Women with Breast Cancer: A Comprehensive Literature Review. Iran Red Crescent Med J. 2016;18(10). e39465. [PubMed ID: 28184329]. https://doi.org/10.5812/ircmj.39465.
-
18.
Cozaru GC, Papari AC, Sandu ML. The Effects of Psycho-education and Counselling for Women Suffering from Breast Cancer in Support Groups. Proc Soc Behav Sci. 2014;128:10-5. https://doi.org/10.1016/j.sbspro.2014.03.110.
-
19.
Bjorneklett HG, Rosenblad A, Lindemalm C, Ojutkangas ML, Letocha H, Strang P, et al. Long-term follow-up of a randomized study of support group intervention in women with primary breast cancer. J Psychosom Res. 2013;74(4):346-53. [PubMed ID: 23497838]. https://doi.org/10.1016/j.jpsychores.2012.11.005.
-
20.
Lotfi Kashani F, Vaziri S, Hajizadeh Z. Sexual Skills Training, Body Image and Sexual Function in Breast Cancer. Proc Soc Behav Sci. 2014;159:288-92. https://doi.org/10.1016/j.sbspro.2014.12.374.
-
21.
Jun EY, Kim S, Chang SB, Oh K, Kang HS, Kang SS. The effect of a sexual life reframing program on marital intimacy, body image, and sexual function among breast cancer survivors. Cancer Nurs. 2011;34(2):142-9. [PubMed ID: 20885305]. https://doi.org/10.1097/NCC.0b013e3181f1ab7a.
-
22.
Moosazadeh M. Meta-Analysis of Prevalence of Smoking in 15-64-year-old Population of West of Iran. Int J Prev Med. 2013;4(10):1108-14. [PubMed ID: 24319549].
-
23.
Moosazadeh M, Nekoei-Moghadam M, Aliram-Zany M, Amiresmaili M. Identification of Mutation of Glucose-6-Phosphate Dehy-drogenase (G6PD) in Iran: Meta- analysis Study. Iran J Public Health. 2013;42(9):1007-15. [PubMed ID: 26060661].
-
24.
Hajizade-Valokolaee M, Yazdani-Khermandichali F, Shahhosseini Z, Hamzehgardeshi Z. Adolescents' sexual and reproductive health: an ecological perspective. Int J Adolesc Med Health. 2016;29(4). [PubMed ID: 26812768]. https://doi.org/10.1515/ijamh-2015-0097.
-
25.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12. [PubMed ID: 8721797].
-
26.
Li J, Liu Z, Chen R, Hu D, Li W, Li X, et al. The quality of reports of randomized clinical trials on traditional Chinese medicine treatments: a systematic review of articles indexed in the China National Knowledge Infrastructure database from 2005 to 2012. BMC Complement Altern Med. 2014;14:362. [PubMed ID: 25256890]. https://doi.org/10.1186/1472-6882-14-362.
-
27.
Duijts SF, Oldenburg HS, van Beurden M, Aaronson NK. Cognitive behavioral therapy and physical exercise for climacteric symptoms in breast cancer patients experiencing treatment-induced menopause: design of a multicenter trial. BMC Womens Health. 2009;9:15. [PubMed ID: 19500403]. https://doi.org/10.1186/1472-6874-9-15.
-
28.
Hoey LM, Ieropoli SC, White VM, Jefford M. Systematic review of peer-support programs for people with cancer. Patient Educ Couns. 2008;70(3):315-37. [PubMed ID: 18191527]. https://doi.org/10.1016/j.pec.2007.11.016.
-
29.
Brotto LA, Heiman JR, Goff B, Greer B, Lentz GM, Swisher E, et al. A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Arch Sex Behav. 2008;37(2):317-29. [PubMed ID: 17680353]. https://doi.org/10.1007/s10508-007-9196-x.
-
30.
Morone G, Iosa M, Fusco A, Scappaticci A, Alcuri MR, Saraceni VM, et al. Effects of a multidisciplinary educational rehabilitative intervention in breast cancer survivors: the role of body image on quality of life outcomes. ScientificWorldJournal. 2014;2014:451935. [PubMed ID: 25405222]. https://doi.org/10.1155/2014/451935.
-
31.
Malary M, Khani S, Pourasghar M, Moosazadeh M, Hamzehgardeshi Z. Biopsychosocial Determinants of Hypoactive Sexual Desire in Women: A Narrative Review. Mater Sociomed. 2015;27(6):383-9. [PubMed ID: 26889096]. https://doi.org/10.5455/msm.2015.27.383-389.
-
32.
Pomery A, Schofield P, Xhilaga M, Gough K. Skills, knowledge and attributes of support group leaders: A systematic review. Patient Educ Couns. 2016;99(5):672-88. [PubMed ID: 26654957]. https://doi.org/10.1016/j.pec.2015.11.017.
-
33.
Alpers GW, Winzelberg AJ, Classen C, Roberts H, Dev P, Koopman C, et al. Evaluation of computerized text analysis in an Internet breast cancer support group. Comput Human Behav. 2005;21(2):361-76. https://doi.org/10.1016/j.chb.2004.02.008.
-
34.
Schover LR, Jenkins R, Sui D, Adams JH, Marion MS, Jackson KE. Randomized trial of peer counseling on reproductive health in African American breast cancer survivors. J Clin Oncol. 2006;24(10):1620-6. [PubMed ID: 16575013]. https://doi.org/10.1200/JCO.2005.04.7159.
-
35.
Rowland JH, Meyerowitz BE, Crespi CM, Leedham B, Desmond K, Belin TR, et al. Addressing intimacy and partner communication after breast cancer: a randomized controlled group intervention. Breast Cancer Res Treat. 2009;118(1):99-111. [PubMed ID: 19390963]. https://doi.org/10.1007/s10549-009-0398-x.