Abstract
Background:
Fractures of the middle and distal diaphysis of the forearm are common in children. Conservative treatment is effective in this regard. Some studies have discussed the risk factors and predictive indicators of re-displacement; however, the objects of the study are all fixed with tubular plaster or double sugar splint.Objectives:
This study was performed to determine the risk factors of re-displacement after closed reduction and double splint plaster fixation of unstable pediatric fractures of the middle and distal diaphysis of the forearm.Methods:
This retrospective study was conducted on 57 patients undergoing closed reduction and plaster fixation after unstable diaphyseal fractures of the middle and distal forearm in Wuxi Children's Hospital of Nanjing Medical University within May 2014 to May 2020. A total of 35 male and 22 female subjects aged 6 - 9 years (average: 7.3 years) participated in this study. They were followed up for more than 6 weeks after fracture healing. According to whether experiencing a secondary displacement within 2 weeks after the fracture, the subjects were divided into two groups, namely displacement, and non-displacement. Gender, age, double fracture, reduction quality, and plaster fixation type were analyzed as relevant, effective factors.Results:
All 57 patients were followed up, and all fractures reached clinical healing standards at the last follow-up. Moreover, 20 and 37 cases were in the shift and non-shift groups, respectively. No statistically significant difference was reported in gender (c2 = 0.168; P = 0.780), age (t = 1.003; P = 0.217), double fracture (c2 = 0.021; P = 1), and plaster fixation type (c2 = 0.416; P = 0.699) between the two groups. The reduction quality (c2 = 7.480; P = 0.025) showed a statistically significant difference. Binary logistic regression analysis showed that reduction quality was a risk factor for fracture relocation providing a predictive value.Conclusions:
Good reduction quality can reduce the risk of fracture displacement.Keywords
1. Background
Forearm fractures are among the most common fractures in children (1-8). Since forearm fractures exhibit strong self-shaping, closed reduction and external fixation are commonly used and effective treatments (9, 10). However, this surgical method shows a higher incidence of relocation (9, 11, 12). At present, there have been studies exploring the risk factors of relocation. The summarized high-risk factors include complete fracture displacement (9), fractures with large initial displacement (12, 13) and improper initial reduction (9, 12), poor plaster shaping and fixation (14), distance from the fracture line to the epiphyseal plate, and double fracture with an ulnar fracture (13). The subjects of these studies are fixed with cast or double sugar splints. The Wuxi Children's Hospital of Nanjing Medical University that conducted this study has been using traditional double-splint plaster fixation for the past 10 years and has achieved good clinical results. For providing a better summary of the treatment experience, the authors conducted a retrospective analysis and summarized the factors related to the displacement of the plaster splint after fixation.
2. Objectives
This study collected the data of patients with unstable diaphyseal fractures of the middle and distal forearm treated by Pediatric orthopaedic outpatient department from May 2014 to May 2020. Five indicators of gender, age, double fracture, reduction quality, and plaster fixation type were analyzed, and the related risk factors for re-displacement were summarized.
3. Methods
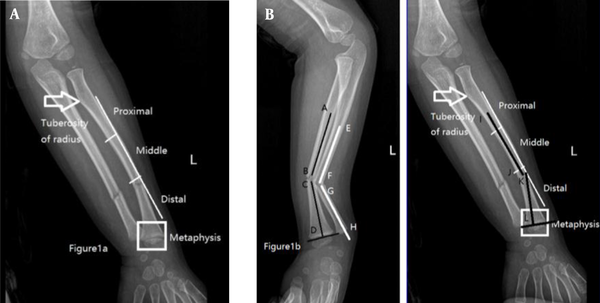
This study was carried out on patients aged 6 - 9 years undergoing manual reduction and plaster splinting in Pediatric orthopaedic outpatient department due to unstable diaphyseal fractures of the middle and distal forearm from May 2014 to May 2020. If the fracture line was blurred, the patient’s fracture line was determined to be healed, and the plaster was removed immediately. Patients with a follow-up duration under 6 weeks were excluded. Patients with pathological fractures, open fractures, multiple fractures, or combined vascular and nerve damage were also excluded. The middle and distal forearm fracture was defined as the position of the fracture line above the metaphysis to the middle 1/3 of the forearm (Figure 1A). Unstable fractures were defined as angles > 10° in either the sagittal or coronal plane, and/or malrotation > 30°, and/or overlap and shortening displacement (angle measurement in Figure 1B). The re-displacement of the fracture was defined as an angle > 15° or an angle of 10 - 15° and a secondary displacement > 30%.
A, white box illustrating metaphysis; from radial tuberosity to metaphysis, backbone regarded as backbone; backbone divided into three equal parts, followed by proximal, middle, and distal segments; B, in lateral radiograph, CD considered perpendicular to the epiphyseal plate of distal radius; angle between AB and CD considered the angle of radius fracture; angle between EF and GH considered the angle of ulna fracture; in the orthographic film, KL considered perpendicular to the epiphyseal plate of the distal radius, and angle between IJ and KL considered -3.7° (i.e., the angle of radius fracture).
All patients underwent manual traction reduction and cast in traction state by two or more attending physicians in the emergency room. The fracture was fixed with a plaster splint in a flexed or extended position over the elbow. X-rays were taken to confirm the fracture reduction shortly after plaster fixation. The fracture reduction standards were evaluated according to the preset fracture reduction standards, and the next treatment measures were judged. The reduction quality was defined as an anatomical reduction with an angle < 5° and a displacement < 10%, good reduction with an angle of 5 - 10° or a displacement of 10 - 30%, and normal reduction with an angle of 5 - 10° and a displacement > 30%.
X-rays were taken immediately after the reduction. Within 2 weeks after plaster fixation, the re-displaced patients were classified into the displacement group, and the patients without displacement were classified into the non-displacement group. The samples were divided into two groups according to secondary displacement, and the five indicators of gender, age, double fracture, reduction quality, and plaster fixation type were analyzed in the two groups. The angle of the fracture was measured by three orthopedic surgeons. Concerning the radial arch and ulnar arch, correction on the coronal plane was performed with an anatomical angle of 3.7°. The authors finally adopted the average of the results of the three surveyors.
The fracture angle was measured by picture archiving and communication system (PACS). Statistical analysis was carried out by SPSS statistical analysis software (version 20.0; SPSS Inc., Chicago, IL, USA). The measurement data that did not conform to the normal distribution are expressed by the median (interquartile range). The count data are expressed by the rate or composition ratio. The non-parametric Mann-Whitney U test was used to compare the two groups of measurement data that did not conform to the normal distribution. A t-test was used to conform to the normal distribution. The Chi-square test was used for enumeration data (Table 1). The respective variables were analyzed by binary logistic regression. The odds ratio was used to express the strength of association, and the 95% confidence interval was determined. A p-value less than 0.05 was considered statistically significant.
Data from Patients with Unstable Fracture of the Middle-distal Forearm
| Variables | Non-displacement Group; n = 37 | Displacement Group; n = 20 | c2/t | P-Value |
|---|---|---|---|---|
| Gender | 0.168 | 0.780 | ||
| Male | 22 | 14 | ||
| Female | 15 | 7 | ||
| Age (y) | 7.90 ± 1.210 | 7.35 ± 1.348 | 1.003 | 0.217 |
| Double fracture | 0.021 | 1 | ||
| Single | 8 | 5 | ||
| Double | 29 | 15 | ||
| Reduction quality | 11.892 | 0.003 | ||
| General | 8 | 10 | ||
| Good | 6 | 5 | ||
| Anatomic | 23 | 5 | ||
| Plaster fixation method | 0.416 | 0.699 | ||
| Extension | 31 | 18 | ||
| Flexion | 6 | 2 |
4. Results
This study was conducted on a total of 57 patients, including 36 male and 21 female subjects, with an average age of 7.3 years (range: 6 - 9 years). The anatomical reduction was performed in 28 cases. In addition, 11 and 18 cases had good and general reductions, respectively. Furthermore, 49 cases were fixed with a gypsum splint in the extended position, and 8 cases were fixed with gypsum in the flexion position. There were 37 cases with no secondary displacement and 20 cases with displacement. Gender (c2 = 0.168; P = 0.780), age (t = 1.003; P = 0.217), double fracture (c2 = 0.021; P = 1), and plaster fixation type (c2 = 0.416; P = 0.699) in the two groups showed no significant difference. The reduction quality (c2 = 7.480; P = 0.025) showed a statistically significant difference (Table 1). Binary logistic regression analysis showed that reduction quality was a risk factor for fracture relocation (Table 2). As the reduction treatment became worse, the re-displacement became easier.
Logistic Regression Analysis Results of Two Categories of Factors Related to Displacement of Middle-distal Forearm Fractures
| Variables | Univariate | |
|---|---|---|
| Odds Radio (95% Confidence Interval) | P-Value | |
| Age (y) | 1.203 (0.659 - 2.196) | 0.547 |
| Gender | 0.348 | |
| Male | 1 | |
| Female | 0.537 (0.147 - 1.968) | |
| Double fracture | 0.817 | |
| Single | 1 | |
| Double | 1.205 (0.248 - 5.868) | |
| Reduction quality | ||
| General | 1 | 0.033 |
| Good | 9.221 (1.589 - 53.506) | 0.013 |
| Anatomic | 4.215 (0.830 - 21.401) | 0.043 |
| Plaster fixation method | 0.388 | |
| Extension | 1 | |
| Flexion | 2.319 (0.343 - 15.683) | |
| Constant | 0.026 | 0.206 |
5. Discussion
The definition of unstable fractures in the distal forearm is unknown. Khaled et al. defined unstable diaphyseal fractures as diaphyseal fractures between the distal and proximal metaphysis, with an angle > 10°, and/or malrotation > 30°, and/or a displacement > 10 mm after an attempted closed reduction (15). Kay et al. defined that the closed reduction of fractures of the middle ulna and radius over 10 years with an angle of more than 10° is unstable (16).
This study referred to the descriptions of Cheng et al. (2), Bae (3), Haddad and Williams (7) integrated with the present clinical experience to define unstable fractures of the middle and distal forearm as the fracture line above the metaphysis to the middle 1/3 of the forearm, angle > 10°, and/or poor rotation > 30°, and/or overlap shortening displacement. Treatment options for ulna and radius fractures in children are controversial. In most cases, considering that young patients have excellent remodeling potential, numerous angulated fractures can be accepted (17, 18). Because the sculpting ability decreases with the age of children, there have still been debates about acceptable angles and displacements (19-21). Rang deems that closed reduction can treat most forearm fractures. The authors of the present study accept the opinions of scholars, such as Khaled et al., Price et al., Bowman et al., and Kutsikovich et al. (15, 22-24), and consider that the failure rate of closed reduction in children over 10 years is high and the acceptable angle range is small. Finally, this study limited the age of children to 6 - 9 years, thereby reducing the effect of age on fracture shaping.
The treatment plan adopted by the authors was that all mid-distal fractures were first manually reduced and fixed with plaster splints. If the initial reduction was satisfactory, patient follow-up continued. If re-displacement occurred within 2 weeks, the reduction was re-manipulated. The reduction quality was referred to a literature report of Yang et al. (9) and defined as an anatomical reduction with an angle < 5° and a displacement < 10%, good reduction with an angle of 5 - 10° or a displacement of 10 - 30%, and normal reduction with an angle of 5 - 10° and a displacement > 30%. Considering that the patients in this study had a small age range and a clear fracture location, integrated with the acceptable angle of fracture proposed by Price et al. (22), this is a reliable classification scheme.
The authors’ hospital is still using gypsum splints to treat children’s fractures for several reasons. Firstly, the price of gypsum splints is low, and the shaping effect is good. Secondly, there are numerous migrant workers in the area where the authors are located, and the population is highly mobile. After the children go back to their home city, there is a lack of pediatric orthopedics physicians, and it is inconvenient to remove the plaster. Thirdly, when the cast is fixed, the forearm will move to the proximal end in the cast during the swelling process (25); however, the traditional cast can be used to directly tighten the external fixation. In summary, the research on the fixed and re-displaced factors of gypsum splint has practical significance to the current situation.
The fracture angle was corrected considering that every backbone stage has a certain curvature on average for the forearm arch (26). Roberts showed an anatomical angle of 3.7º in the middle of the forearm (27). The data of the study by Roberts were used in the present study to make corrections. Three physicians used the PACS system to measure the angle and then calculated the average of their measurements.
In this study, the cases were divided into displaced and non-displaced groups. Before reduction, there were no significant differences in age, gender, and fracture angle (P > 0.05). The factor of fracture angulation before the reduction was not a risk factor for re-displacement, which is different from the re-displacement of distal radius fractures (24, 28, 29). The authors are skeptical about this conclusion due to several reasons. Firstly, children’s first-time radiographs were often not standard due to pain and fear. Secondly, the quality of imaging in different levels of hospitals was different. Thirdly, in the X-rays obtained before reduction, the film’s fracture angulation and displacement data were biased, which is a possible reason for this conclusion.
The traditional view is that due to the swelling of the affected limb and the gravity of the plaster, the flexion position of the plaster slides to the distal end to generate longitudinal shear force and fracture displacement (25). The data in this study showed that the type of plaster fixation was not an effective factor in fracture relocation. Some scholars have conducted studies on distal radius fractures, and the results showed that combined ulnar fractures are a factor for re-displacement (13, 30). The present study’s data came to the opposite conclusion that double fractures were not a risk factor for re-displacement. The reduction quality was a risk factor for the re-displacement of the fracture. As reduction quality became worse, re-displacement risk became higher. This conclusion is less controversial (9, 13, 30).
There were several limitations in this study. The authors only analyzed the factors of re-displacement and did not study the treatment and prognosis after re-displacement. The follow-up time set was short. The fractures with the anatomical reduction in the sample had a large buffer space during the progress to the re-displacement process. A sample with a general reduction quality had a large fracture angle, and even a slight displacement was judged to be displaced again. The small sample size in this study limited the need to increase the sample size and perform in-depth analyses on fracture angles, such as the coronal and sagittal angles before fracture reduction, body mass index, and subcutaneous fat thickness. Propensity score matching analyzed confounding factors.
5.1. Conclusion
The results of this study showed that the quality of reduction is a risk factor affecting the re-displacement of unstable fractures in the middle and distal forearm of children. The selection of a good fracture reduction is an effective measure to reduce the re-displacement of fractures.
References
-
1.
Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908-15. [PubMed ID: 11561245]. https://doi.org/10.1053/jhsu.2001.26322.
-
2.
Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop. 1999;19(3):344-50. [PubMed ID: 10344317].
-
3.
Bae DS. Pediatric distal radius and forearm fractures. J Hand Surg Am. 2008;33(10):1911-23. [PubMed ID: 19084202]. https://doi.org/10.1016/j.jhsa.2008.10.013.
-
4.
de Putter CE, van Beeck EF, Looman CW, Toet H, Hovius SE, Selles RW. Trends in wrist fractures in children and adolescents, 1997-2009. J Hand Surg Am. 2011;36(11):1810-1815 e2. [PubMed ID: 22036281]. https://doi.org/10.1016/j.jhsa.2011.08.006.
-
5.
Hedstrom EM, Svensson O, Bergstrom U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81(1):148-53. [PubMed ID: 20175744]. [PubMed Central ID: PMC2856220]. https://doi.org/10.3109/17453671003628780.
-
6.
Helenius I, Lamberg TS, Kaariainen S, Impinen A, Pakarinen MP. Operative treatment of fractures in children is increasing. A population-based study from Finland. J Bone Joint Surg Am. 2009;91(11):2612-6. [PubMed ID: 19884435]. https://doi.org/10.2106/JBJS.H.01519.
-
7.
Haddad FS, Williams RL. Forearm fractures in children: avoiding redisplacement. Injury. 1995;26(10):691-2. [PubMed ID: 8745807]. https://doi.org/10.1016/0020-1383(95)00136-0.
-
8.
Khosla S, Melton L3, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290(11):1479-85. [PubMed ID: 13129988]. https://doi.org/10.1001/jama.290.11.1479.
-
9.
Yang JJ, Chang JH, Lin KY, Lin LC, Kuo CL. Redisplacement of diaphyseal fractures of the forearm after closed reduction in children: a retrospective analysis of risk factors. J Orthop Trauma. 2012;26(2):110-6. [PubMed ID: 21804412]. https://doi.org/10.1097/BOT.0b013e318216b403.
-
10.
Mehlman CT. Injuries to the shafts of the radius and ulna. In: Beaty JH, Kasser JR, editors. Rockwood and Wilkins' fractures in children. 3. 7th ed. Philadelphia, USA: Lippincott Williams & Wilkins; 2010.
-
11.
Voto SJ, Weiner DS, Leighley B. Redisplacement after closed reduction of forearm fractures in children. J Pediatr Orthop. 1990;10(1):79-84. [PubMed ID: 2298900].
-
12.
Monga P, Raghupathy A, Courtman NH. Factors affecting remanipulation in paediatric forearm fractures. J Pediatr Orthop B. 2010;19(2):181-7. [PubMed ID: 19907346]. https://doi.org/10.1097/BPB.0b013e3283314646.
-
13.
Fenton P, Nightingale P, Hodson J, Luscombe J. Factors in redisplacement of paediatric distal radius fractures. J Pediatr Orthop B. 2012;21(2):127-30. [PubMed ID: 21934633]. https://doi.org/10.1097/BPB.0b013e3283492117.
-
14.
Iltar S, Alemdaroglu KB, Say F, Aydogan NH. The value of the three-point index in predicting redisplacement of diaphyseal fractures of the forearm in children. Bone Joint J. 2013;95-B(4):563-7. [PubMed ID: 23539712]. https://doi.org/10.1302/0301-620X.95B4.31143.
-
15.
Khaled M, Fadle AA, Attia AK, Sami A, Hafez A, Abol Oyoun N. Single-bone versus both-bone plating of unstable paediatric both-bone forearm fractures. A randomized controlled clinical trial. Int Orthop. 2021. [PubMed ID: 34120195]. https://doi.org/10.1007/s00264-021-05097-z.
-
16.
Kay S, Smith C, Oppenheim WL. Both-bone midshaft forearm fractures in children. J Pediatr Orthop. 1986;6(3):306-10. [PubMed ID: 3711323]. https://doi.org/10.1097/01241398-198605000-00009.
-
17.
Fuller DJ, McCullough CJ. Malunited fractures of the forearm in children. J Bone Joint Surg Br. 1982;64(3):364-7. [PubMed ID: 7096406]. https://doi.org/10.1302/0301-620X.64B3.7096406.
-
18.
Hogstrom H, Nilsson BE, Willner S. Correction with growth following diaphyseal forearm fracture. Acta Orthop Scand. 1976;47(3):299-303. [PubMed ID: 952216]. https://doi.org/10.3109/17453677608991994.
-
19.
Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop. 2005;25(4):507-12. [PubMed ID: 15958905]. https://doi.org/10.1097/01.bpo.0000158005.53671.c4.
-
20.
Ogden JA, Beall JK, Conlogue GJ, Light TR. Radiology of postnatal skeletal development. IV. Distal radius and ulna. Skeletal Radiol. 1981;6(4):255-66. [PubMed ID: 7292022]. https://doi.org/10.1007/BF00347198.
-
21.
Johari AN, Sinha M. Remodeling of forearm fractures in children. J Pediatr Orthop B. 1999;8(2):84-7. [PubMed ID: 10218165].
-
22.
Price CT, Scott DS, Kurzner ME, Flynn JC. Malunited forearm fractures in children. J Pediatr Orthop. 1990;10(6):705-12. [PubMed ID: 2250053]. https://doi.org/10.1097/01241398-199011000-00001.
-
23.
Bowman EN, Mehlman CT, Lindsell CJ, Tamai J. Nonoperative treatment of both-bone forearm shaft fractures in children: predictors of early radiographic failure. J Pediatr Orthop. 2011;31(1):23-32. [PubMed ID: 21150728]. [PubMed Central ID: PMC3073825]. https://doi.org/10.1097/BPO.0b013e318203205b.
-
24.
Kutsikovich JI, Hopkins CM, Gannon E3, Beaty JH, Warner WJ, Sawyer JR, et al. Factors that predict instability in pediatric diaphyseal both-bone forearm fractures. J Pediatr Orthop B. 2018;27(4):304-8. [PubMed ID: 28777160]. https://doi.org/10.1097/BPB.0000000000000480.
-
25.
Gainor JW, Hardy JH. Forearm fractures treated in extension. Immobilization of fractures of the proximal both bones of the forearm in children. J Trauma. 1969;9(2):167-71. [PubMed ID: 5763341].
-
26.
Sage FP. Medullary fixation of fractures of the forearm. A study of the medullary canal of the radius and a report of fifty fractures of the radius treated with a prebent triangular nail. J Bone Joint Surg Am. 1959;41-A:1489-516. [PubMed ID: 13854617].
-
27.
Roberts JA. Angulation of the radius in children's fractures. J Bone Joint Surg Br. 1986;68(5):751-4. [PubMed ID: 3782237]. https://doi.org/10.1302/0301-620X.68B5.3782237.
-
28.
McQuinn AG, Jaarsma RL. Risk factors for redisplacement of pediatric distal forearm and distal radius fractures. J Pediatr Orthop. 2012;32(7):687-92. [PubMed ID: 22955532]. https://doi.org/10.1097/BPO.0b013e31824b7525.
-
29.
Asadollahi S, Ooi KS, Hau RC. Distal radial fractures in children: risk factors for redisplacement following closed reduction. J Pediatr Orthop. 2015;35(3):224-8. [PubMed ID: 24978123]. https://doi.org/10.1097/BPO.0000000000000239.
-
30.
Jordan RW, Westacott D, Srinivas K, Shyamalan G. Predicting redisplacement after manipulation of paediatric distal radius fractures: the importance of cast moulding. Eur J Orthop Surg Traumatol. 2015;25(5):841-5. [PubMed ID: 25877430]. https://doi.org/10.1007/s00590-015-1627-0.