Abstract
Context:
COVID-19 is a serious threat to the world as a whole, and pregnant women are at increased risk of the infection.Objectives:
In the present study, we have reviewed the outcomes of neonates of pregnant women with COVID-19.Data Sources:
We searched Medline, Web of Science, and Scopus databases from December 2019 to April 2020. The search was conducted using the following keywords: COVID-19, newborn, neonatal mortality, neonatal morbidity, pregnant women, pregnancy outcome, or combinations of these keywords. Inclusion and exclusion criteria were all English language articles about COVID-19 in pregnant women and outcomes of pregnancy. Review articles were excluded because of reporting repetitive articles.Study Selection:
Two researchers independently screened the titles of all recorded citations, removed duplicate records, and distinguished potentially relevant studies for inclusion. Then, abstracts of selected citations were independently reviewed by two researchers for further relevance, with full-text manuscripts retrieved as appropriate. In disagreement cases, a third consultant was asked to act as an intervener.Results:
In total, 6 articles had inclusion criteria. Newborns were examined by laboratory methods, including; the pharyngeal swab specimens, throat swab specimen, amniotic fluid, cord blood, breast milk. The neonatal complications such as a slight increase in the myocardial enzyme, fever, tachycardia, thrombocytopenia, vomiting and pneumothorax, shortness of breath, mild pulmonary infection, transient tachypnea and the skin rashes higher concentrations of IgG and IgM are reported. The shortness of breath was the most frequent clinical first symptom among neonates.Conclusions:
There are strong ambiguities concerning the vertical transmission from mother to fetus. Extensive research is needed to resolve ambiguities about the virus and its impact on pregnancy outcomes.Keywords
1. Context
The coronavirus-19, which is a pandemic, was first appeared in Wuhan (China) in December 2019 (1). Its morbidity and mortality rates are rising in most of the countries around the world (2).
2. Objectives
The virus spreads rapidly in the air through droplets thrown from patients’ respiratory systems (3). Several studies have investigated the transmission routes and risks of this deadly virus. The virus has a very high mortality rate and disability, particularly in certain individuals, including people with underlying diseases, the elderly, and those with immune system defects (4-7).
Pregnancy affects the immune system of pregnant women. Therefore, they are at increased risk of COVID-19 (8). There is a lot of ambiguity about the coronavirus. In this regard, the results reported by various studies are not consistent (9-11). However, a case study reported infection in newborns 36 hours after birth in China (12), but also, another study has reported that it is not possible to give a definite opinion about the possibility of vertical and neonatal transfer. Therefore, further research is needed (13). In the present study, we have reviewed the outcomes of neonates of pregnant women with COVID-19.
3. Study Design
We systematically searched Medline, Web of Science, and Scopus from December 2019 to April 2020. The search strategy consisted of free-text words, words in the title, or abstract and medical subject headings (MeSH).
Inclusion and exclusion criteria. All English language articles about COVID-19 in pregnant women and outcomes of pregnancy were included. Review articles were excluded because of reporting repetitive articles.
4. Study Selection
Initially, studies were independently screened by title and abstract by two researchers, and they searched for studies that had the following terms; novel coronavirus, COVID-19, newborn, neonatal mortality, neonatal morbidity, pregnant women, pregnancy outcome or combining these words, electronically.
In the present review, the following types of studies included; cross-sectional, case series, case-control, case reports, and letters to journal editors that were accepted.
Abstracts were independently reviewed by two researchers for further relevance, with full-text manuscripts retrieved as appropriate. In the case of disagreement between the two reviewers, the opinions of a third researcher were used. Finally, the researchers reviewed the articles and the extracted data to ensure the accuracy of the assessments.
5. Data Extraction
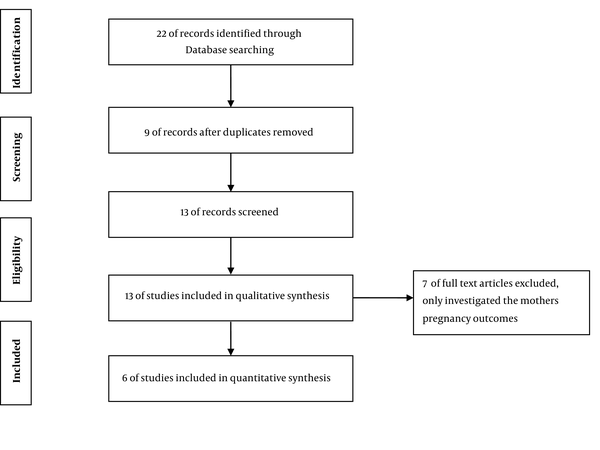
The search resulted in 22 abstracts. The following data were extracted: first author, study date, sample size, gestational age, infant’s survival to the end of the study, type of delivery, the onset of mothers’ clinical symptoms, neonatal samples tested, neonatal sex, neonatal first, and fifth minutes Apgar. All articles that met the inclusion criteria were reviewed. All duplicate and unrelated articles were excluded. Out of 22 abstracts, 6 were categorized as potentially eligible for the systematic review. In the last stage, 6 full-text articles were used in the review (Figure 1).
Articles assessment of the initial search process to record the data in the final review
6. Results
In total, 6 articles were fully reviewed. General features of reviewed articles are presented in Table 1. Infants were examined by laboratory methods, including; the pharyngeal swab specimens, throat swab specimen, amniotic fluid, cord blood, breast milk. General characteristics of infants born to women with COVID-19 are presented in Table 2.
General Features of Reviewed Articles
| Authors | Study Date | Sample Size | Gestational Age | Infants Survival to the End of the Study | Type of Delivery | ||||
|---|---|---|---|---|---|---|---|---|---|
| Preterm | Full term | Discharged | Died | Hospitalization | CS | NVD | |||
| Chen et al. (14) | NA | 4 | 0 | 4 | 4 | 0 | 0 | 3 | 1 |
| Chen et al. (15) | Jan, 2020 | 9 | 4 | 5 | 9 | 0 | 0 | 9 | 0 |
| Zhu et al. (9) | January to February 2020 | 9 | 6 | 4 | 5 | 1 | 4 | 7 | 2 |
| Liu et al. (16) | January to February 2020 | 15 | 3 | 8 | 11 | 0 | 0 | 10 | 1 |
| Yu et al. (17) | Jan to Feb 2020 | 7 | 0 | 7 | 7 | 0 | 0 | 7 | 0 |
| Zeng et al. (18) | Feb to March 6, 2020 | 6 | NA | NA | NA | NA | NA | 6 | 0 |
General Characteristics of Infants Born to Women with COVID-19
| Authors | Onset of Mothers Clinical Symptoms | Sex | Apgar Scores (1 min, 5 min) | Asphyxia | Neonatal Samples Tested | Birth Weight | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before Delivery | Day of Delivery | After Delivery | Female | Male | Intrauterine | Neonatal | Low Birth Weight | Normal | |||
| Chen et al. (14) | 9 | 9 | NA | NA | NA | (7 - 8, 8 - 9) | NA | NA | Throat swabs specimen | 0 | 4 |
| Chen et al. (15) | 4 | 1 | NA | 1 | 3 | (8 - 9, 9 - 10) | 1 | 1 | Amniotic fluid, cord blood, throat swab, breast milk | 2 | 7 |
| Zhu et al. (9) | 4 | 2 | 3 | 2 | 8 | (7 - 10, 8 - 10) | 3 | 6 | Pharyngeal swab specimens | 7 | 2 |
| Liu et al. (16) | 15 | NA | NA | NA | NA | (8, 8 - 10) | 0 | 0 | NA | NA | NA |
| Yu et al. (17) | 7 | NA | NA | NA | NA | NA | 0 | 0 | Nasopharyngeal swabs | 0 | 7 |
| Zeng et al. (18) | NA | NA | NA | NA | NA | (8 - 9, 9 - 10) | NA | NA | Blood, throat swab samples | NA | NA |
Some neonatal complications such as slight increases in the myocardial enzyme (15), fever, tachycardia, thrombocytopenia, vomiting, and pneumothorax (9), shortness of breath, mild pulmonary infection (17), transient tachypnea and the skin rashes (14), higher concentrations of IgG and IgM (18) have been reported. The shortness of breath was the most prevalent clinical symptom in the neonates (9). The babies were immediately separated from their mothers and fed formula (14, 18). The neonates’ positive sputum sample is reported in some cases, and the neonates who were discharged after two negative tests (17). Some major prenatal problems, such as fetal distress, preterm labor, premature rupture of membranes, and amniotic fluid abnormalities are also reported among infected women (9). COVID-19 is a high-risk pandemic. Despite the efforts of scientists, there are many ambiguities about COVID-19. There is an inconsistency between the results of studies on vertical transmission from mothers to neonates (7, 14, 15, 18).
In total, 50 pregnant mothers were investigated in the reviewed studies, the pregnancy continued in 4 pregnant mothers at the end of the study (16). Pregnant women reported different symptoms concerning COVID-19 infection. Fever and cough were the most poetic presentations (9, 14). However, in one article, no symptom was reported (18).
As reported in Table 1, most neonates are born at full term through C-section. We know that the transmission of infectious diseases from mother to newborn occurs through contact with infectious droplets. Therefore, in cases that the mother was infected with COVID-19, the infants were separated immediately from the mother, and the formula was selected as the safest way to feed the newborns (14, 18).
The report published by the Centers for Disease Control and Prevention did not prohibit breastfeeding for infected mothers. Also, Chen et al. (15) reported no coronavirus in maternal milk. One of the concerns of women with infectious diseases is the vertical transmission from mother to fetus. Wang et al. (12) reported the symptoms of infection in newborns 36 hours after birth in China. Although Yu and colleagues reported a case of newborn pulmonary infection among their study population, this newborn was discharged after two weeks without any particular problem (17). However, a study found that all swab throat tests of neonates born to mothers with COVID-19 infection were negative. Meanwhile, there are strong ambiguities in the vertical transmission of COVID-19 (9).
7. Conclusions
Although most studies have not reported vertical mother-to-child transmission in the third trimester, sufficient information is not available on the effect of the virus on pregnancy outcomes of mothers who become infected early in pregnancy.
Besides, it is not clear whether infection during early pregnancy causes fetal defects or risk of miscarriage. Answering all these questions require more detailed studies with higher sample size in different parts of the world.
References
-
1.
Hui DS, Azhar EI, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases. 2020;91:264. [PubMed ID: 31953166]. https://doi.org/10.1016/j.ijid.2020.01.009.
-
2.
Malik YS, Sircar S, Bhat S, Vinodhkumar OR, Tiwari R, Sah R, et al. Emerging Coronavirus Disease (COVID-19), a pandemic public health emergency with animal linkages: Current status update. PrePrints. 2020. https://doi.org/10.20944/preprints202003.0343.v1.
-
3.
Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):210-7. [PubMed ID: 32027573]. https://doi.org/10.1148/radiol.2020200274.
-
4.
World Health Organization. Novel Coronavirus ( 2019-nCoV): situation report, 3. 2020.
-
5.
Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance. 2020;25(5):2000062. [PubMed ID: 32046819]. https://doi.org/10.2807/1560-7917.ES.2020.25.5.2000062.
-
6.
Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance. 2020;25(3):2000045. [PubMed ID: 31992387]. https://doi.org/10.2807/1560-7917.ES.2020.25.3.2000045.
-
7.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497-506. https://doi.org/10.1016/S0140-6736(20)30183-5.
-
8.
Arabi S, Vaseghi G, Heidari Z, Shariati L, Amin B, Rashid H, et al. Clinical characteristics of COVID-19 infection in pregnant women: a systematic review and meta-analysis. medRxiv. 2020. https://doi.org/10.1101/2020.04.05.20053983.
-
9.
Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Translational pediatrics. 2020;9(1):51. [PubMed ID: 32154135]. https://doi.org/10.21037/tp.2020.02.06.
-
10.
Ludvigsson JF. Systematic review of COVID‐19 in children show milder cases and a better prognosis than adults. Acta Paediatrica. 2020. [PubMed ID: 32202343]. https://doi.org/10.1111/apa.15270.
-
11.
Khan MMA, Khan MN, Mustagir MG, Rana J, Haque MR, Rahman MM. COVID-19 infection during pregnancy: a systematic review to summarize possible symptoms, treatments, and pregnancy outcomes. medRxiv. 2020. https://doi.org/10.1101/2020.03.31.20049304.
-
12.
Wang S, Guo L, Chen L, Liu W, Cao Y, Zhang J, et al. A case report of neonatal COVID-19 infection in China. Clinical Infectious Diseases. 2020.
-
13.
Zaigham M, Andersson O. Maternal and Perinatal Outcomes with COVID‐19: a systematic review of 108 pregnancies. Acta Obstetricia et Gynecologica Scandinavica. 2020. [PubMed ID: 32259279]. https://doi.org/10.1111/aogs.13867.
-
14.
Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H, et al. Infants born to mothers with a new coronavirus (COVID-19). Frontiers in Pediatrics. 2020;8:104. [PubMed ID: 32266184]. https://doi.org/10.3389/fped.2020.00104.
-
15.
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet. 2020;395(10226):809-15. https://doi.org/10.1016/S0140-6736(20)30360-3.
-
16.
Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, et al. Pregnancy and Perinatal Outcomes of Women With Coronavirus Disease (COVID-19) Pneumonia: A Preliminary Analysis. American Journal of Roentgenology. 2020:1-6. [PubMed ID: 32186894]. https://doi.org/10.2214/AJR.20.23072.
-
17.
Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. The Lancet Infectious Diseases. 2020. https://doi.org/10.1016/S1473-3099(20)30176-6.
-
18.
Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. Jama. 2020. https://doi.org/10.1001/jama.2020.4861.
