Abstract
Introduction:
Neurofibroma is a rare benign tumor that often originates from peripheral nerve sheath. The solitary type can be seen in middle-aged people. Hyalinization is a rare phenomenon that can be observed in fibrous tumors.Case Presentation:
In this report, a 46-year-old male patient with a hard mass in proximal femoral is presented. He had central necrosis in the initial imaging studies. The mass was painful and caused signs of local anesthetic for the patient. Extensive hyalinization was observed in the central part of the mass in histopathological studies. S100 protein was widely positive, but CD34 and bcl2 were negative. No necrosis was observed.Conclusions:
The extensive central hyalinization is very rare in fibrous tumors and is observed for the first time in neurofibroma. Hyalizination in the work up prior to surgical treatment led to misdiagnosis of the radiologist and the surgeon. Detailed pathological examination is very important to definitive diagnosis.Keywords
Solitary neurofibroma Histopathologic Examination Immunohistochemistry
1. Introduction
Tumors of the peripheral nerves in the limbs are considered as rare tumors. Benign tumors of peripheral nerve sheath tumors (PNSTs) are classically divided into two Neuilemmoma (Shawannoma) and Neurofibroma types (1). Neurofibroma solitary can be more seen in middle-aged patients between 20 and 40 years. It can occur in childhood and adolescence in males associated with Neurofibromatosis (NF1) syndrome (1, 2).
Neurofibroma is considered a benign tumor which is common in soft tissues of the limbs. It consists about 5% of the tumors of the soft tissue. Neurofibroma is classically classified into three types including localized, diffuse, and plexiform (in neurofibromatosis) tumors (2).
Solitary neurofibroma often can be seen with capsule, is rubbery, and can be observed in the trunk in middle age, but it can also occur in the limbs. Symptoms of these tumors can be caused by touching mass, pain, numbness, and weakness in the nerve path. Management depends on the observed complications (3). Indication in surgical excision can be seen when it causes pain, progressive neurological deterioration, signs of pressure on surrounding tissue, organ dysfunction, aesthetic considerations, and the possibility of malignant degeneration (3). In this report, a patient with a painful palpable and numbness mass in the thigh is described. He had evidences of central necrosis with a high probability of malignancy according to the unusual radiography.
2. Case Presentation
A 46-year-old male patient with a mass in the top of left thigh for one year with the progressive development process referring to the orthopedic clinic was studied.
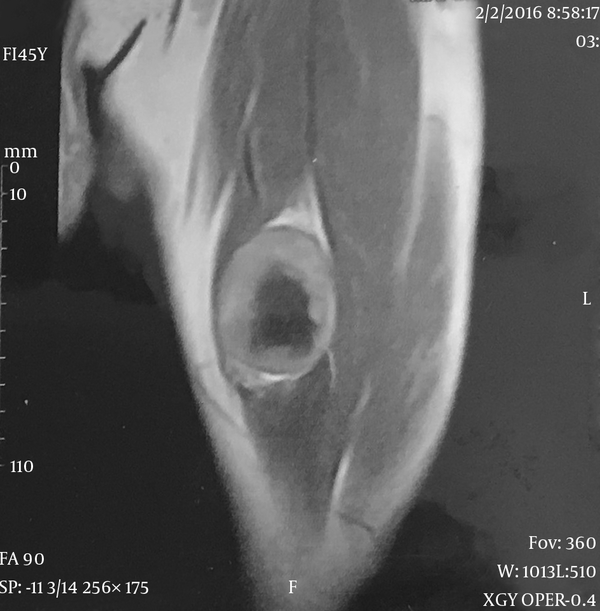
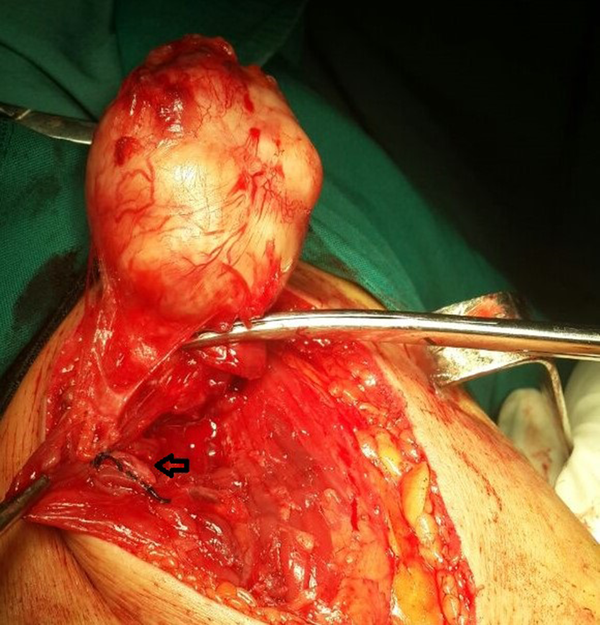
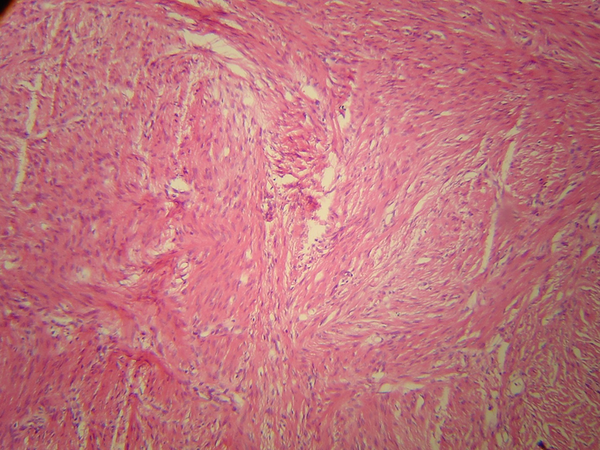
Initial examinations revealed a hard and non-mobile mass about 5.5 × 6 cm in proximal and anteromedial of left thigh. It was painful in deep palpation indicating numbness in the medial and anterior of the thigh. The skin over the mass was intact and no changes in the shape was observed. In the examination of the skin no stains skin changes was seen. The patient had no history of diseases and he was a perfectly healthy farmer. Radiography was performed for the patient at first demonstrating no disorder in the femur bone, but there was only one soft tissue mass with no evidence of calcification. A hypoechoic mass with distinct borders inside thigh muscles with fluid retention in the central part was detected in ultrasonography. There were small collateral vessels in the posteromedial of the mass from femoral artery. MRI was requested for the patient according to the sonographic findings with the possibility of malignant masses. According to MRI, a mass with dimensions of 52 × 44 mm was diagnosed in the anterior left thigh in the rectus femuris muscle. The mass has central hyposignal in the T1 (Figure 1). The radiologist believed that the central necrosis evidence can imply a mass with the possibility of synovial sarcoma or soft tissue sarcoma. Blood tests were completely normal. Pulmonary and lymph nodes examinations were all normal. There was no metastasis in preoperative workup. Incisional biopsy was considered for the patient. The patient was under general anesthesia and an anteromedial incision on the tumor was used to open muscle compartment. A hard mass with a clear capsule with a specific blood vessel attached to the adjacent nerve which was seemed to be the branch of the femoral nerve was observed. That was attached to the mass and there was no possibility of separation (Figure 2). Blood vessel was first ligated. Given the state of the mass, decided decision was made to remove the entire mass. The mass was released from surrounding tissue and the entire mass was removed with an intact capsule. In histopathological examination, the mass was benign spindle cell tumor (Figure 3A) which is neurofibroma based on pathological findings. In the immunohistochemical study, SMA, BCL2, CD34 tumor cells were negative. S100 was diffused and positive (Figure 3B). B-catenin in staining was cytoplasmic dot like staining but not nuclear. No necrosis was observed in the central parts of the tumor, but the extensive hyalinization was seen in the central part of the tumor. The patient's parents had complete satisfaction form to publish this report.
Sagittal View of MRI Showing the Intra-Muscular Well-Defined and Capsulated Mass Without Expanding Into the Surrounding Tissue
Intraoperative View of the Mass with a Specific Capsule and Independent Ligated Blood Vessel
Microscopically (Hematoxylin and Eosin, 100 ×), Indicating Spindle Cell Tumor Was Observed in the Fibromyxoid Background.
3. Discussion
In this study, we presented a patient with palpable soft tissue mass in the proximal thigh. The symptoms included pain and numbness in the anterior and medial thigh. Solitary neurofibroma can be superficial or deep and it can also be formed next to each peripheral nerve (4). The mass is variant from asymptomatic to progressive pain, weakness, tingling and numbness. Palpable mass with rigid structure is regarded as the first clinical examination findings (4).
Ultrasonography plays an important role in the initial assessment of soft tissue tumors. Solitary neurofibroma is often a hypoechoic and uncompressed mass that can be with or without intrinsic blood flow (5). In the studied patient, contrary to the listed findings, accumulation of fluid in the central part of the primary tumor was misdiagnosed due to the central hyalinization of the tumor. According to the same protests of neurofibroma and neurilemmomas, it is difficult to differentiate the two types of tumors but both are benign (6). Central hyalinization could not be differentiated from the central necrosis which indicated the possibility of malignancy.
Benign tumors of the peripheral nerves are notable microscopic heterogeneity present even with full origin from neural crest. The differential diagnosis of these tumor is very difficult using Hematoxylin-Eosin stained section (2). Immunohistochemical evaluation is needed for a definitive diagnosis. Neurofibroma has special features of immunoprofile. This tumor is an aggregation of multiple cells. Most of these cells express S100 proteins in neurofibroma which are often shwann cells. A minority of these cells express CD34 and are seen in perineurial fibroblasts cells (2). S100 protein was extensively positive in immunohistochemical findings, but CD34 was negative. Traistaru et al. reported similar histopathologic findings regarding neurofibroma beside the shoulder joint associated with the brachial plexus which is consistent with our results. CD34 and bcl2 are both positive in other solitary fibrous tumors (2).
Hyalinizing in spindle cell tumor in soft tissue masses have similar protests as low grade fibromyxoidsarcoma (7). The tumor is primary painless with the slow growth and it can be seen in depth in the proximal of the limbs of middle-aged people (14 to 64 years) (7). Accordingly, the tumor was considered as one of the important differential diagnosis for our patient. The most important characteristic features of the tumor were its scattered large rosette like structure that often merged with serpiginous area of dense hyalinization (7). However, unlike neurofibroma, diffused S100 tumor is not positive. According to Lane et al. hyalinizing in spindle cell tumor with giant rosettes definitively confirms low grade fibroblastic tumor similar to low grade fibromyxoid sarcoma (7). We report the first case of neurofibroma with extensive hyalinization in the central part of the tumor. In the preoperative workup the hyalinization led to the wrong diagnosis. Surgical therapy and removing the entire mass is considered the best therapy for the tumor originated from the peripheral nerves. Ten to 23% of fibrous solitary tumors of the soft tissue can be malignant (8). These tumors are unpredictable and long-term follow-up after surgery and removing the tumor should be done (9).
A patient with solitary neurofibroma in the proximal thigh with central extensive hyalinization was studied. Hyalizination in the work up prior to surgical treatment led to misdiagnosis of the radiologist and the surgeon. The patient was likely to have malignant mass. Low grade fibromyxoid sarcoma is one of the tumors with similar demonstration in differential diagnosis. This tumor is similar to neurofibroma and accurate histopathologic investigation must be performed for differentiation.
Acknowledgements
References
-
1.
Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164(2):395-402. [PubMed ID: 7839977]. https://doi.org/10.2214/ajr.164.2.7839977.
-
2.
Traistaru R, Rogoveanu O, Popescu R, Enachescu V, Ghilusi M. Periarticular diffuse neurofibroma of the upper limb. Rom J Morphol Embryol. 2011;52(4):1377-83. [PubMed ID: 22203949].
-
3.
Gottfried ON, Viskochil DH, Fults DW, Couldwell WT. Molecular, genetic, and cellular pathogenesis of neurofibromas and surgical implications. Neurosurgery. 2006;58(1):1-16. discussion 1-16. [PubMed ID: 16385324].
-
4.
Crawford AH, Schorry EK. Neurofibromatosis update. J Pediatr Orthop. 2006;26(3):413-23. [PubMed ID: 16670560]. https://doi.org/10.1097/01.bpo.0000217719.10728.39.
-
5.
Reynolds DJ, Jacobson JA, Inampudi P, Jamadar DA, Ebrahim FS, Hayes CW. Sonographic characteristics of peripheral nerve sheath tumors. AJR Am J Roentgenol. 2004;182(3):741-4. [PubMed ID: 14975979]. https://doi.org/10.2214/ajr.182.3.1820741.
-
6.
Joe YS, Chen HS, Meng NH, Fong YC, Chou LW. Solitary Neurofibroma at the Popliteal Fossa in a Patient With Leg Numbness—A Case Report. J Med Ultrasound. 2010;18(3):136-40. https://doi.org/10.1016/s0929-6441(10)60019-7.
-
7.
Lane KL, Shannon RJ, Weiss SW. Hyalinizing spindle cell tumor with giant rosettes: a distinctive tumor closely resembling low-grade fibromyxoid sarcoma. Am J Surg Pathol. 1997;21(12):1481-8. [PubMed ID: 9414192].
-
8.
Mentzel T, Bainbridge TC, Katenkamp D. Solitary fibrous tumour: clinicopathological, immunohistochemical, and ultrastructural analysis of 12 cases arising in soft tissues, nasal cavity and nasopharynx, urinary bladder and prostate. Virchows Arch. 1997;430(6):445-53. [PubMed ID: 9230909].
-
9.
Njoumi N, Elabsi M, Attolou G, Elouazzani H, Elalami FH, Chkoff MR. Solitary preperitoneal neurofibroma: a case report. BMC Res Notes. 2015;8:115. [PubMed ID: 25879938]. https://doi.org/10.1186/s13104-015-1098-8.