Abstract
Introduction:
Hypercoagulable state may be an important first presentation in malignancies especially pancreatic cancer. The trousseau syndrome is caused by venous thrombosis, non-bacterial thrombotic endocarditis and arterial thrombosis. We describe a patient who had the cerebral infarction as the initial manifestation of pancreatic cancer and we discuss that full work up for every patient with atypical stroke should be done.Case Presentation:
We report a 67-year-old man who developed multiple cerebral infarctions as the initial manifestation of pancreatic cancer. Cancer antigen 19-9 (CA 19-9) was 52,065 U/mL (Normal value: 0 - 33 U/mL), computerized tomography (CT) scan of the abdomen showed multiple hypodensities in both lobes of the liver and Heterogeneous hypodensity was seen in the pancreas that was highly suggestive of pancreas adenocarcinoma and was confirmed with the biopsy.Conclusions:
In the case of multiple brain infarctions in both anterior and posterior circulation, without evidence of common cause, trousseau syndrome and hypercoagulability state should be considered.Keywords
1. Introduction
Pancreatic cancer is currently one of the most common causes of mortality in the world that has a very poor prognosis. It presents with obstructive jaundice, abdominal discomfort, epigastric pain, lethargy, weight loss, acute pancreatitis and rarely trousseau syndrome. In 1865, Armand Trousseau showed that migratory thrombophlebitis could be due to an occult visceral malignancy (1). The common presentation of trousseau syndrome includes venous thrombosis, non-bacterial thrombotic endocarditis (NBTE) and arterial thrombosis (2). Trousseau’s can be identified by an early sign of gastric or pancreatic cancer typically appearing months to years before the diagnosis of cancer, because the tumor may be too small to be detected by conventional methods (3). Cancer and ischemic stroke independently carry a large burden of morbidity and mortality. An autopsy study shows 15% of patients with malignancy have evidence of stroke diagnosed pathologically. Only half of these patients showed clinical stroke during life, suggesting that hypercoagulability is an important presentation in cancer (4, 5). We will describe a patient who had the cerebral infarction as the first manifestation of pancreatic cancer.
2. Case Presentation
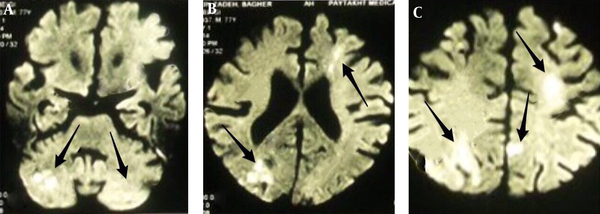
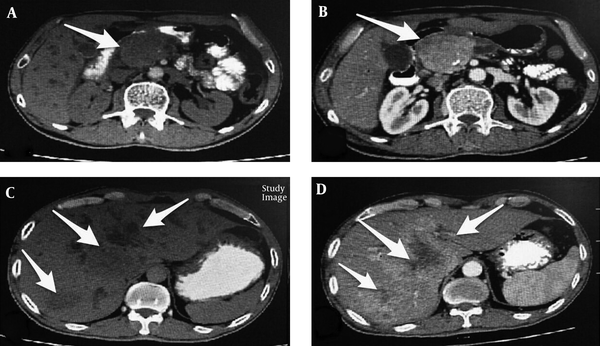
A 67-year-old man has been admitted because of investigation of multiple strokes. He was apparently normal until three months ago. Then he fell in catastrophic condition. First, he developed sudden ataxia; then 4 days later, developed right hemiparesis and then felt leg weakness. He has been admitted to a hospital and was managed as a case of acute ischemic stroke. BRAIN diffusion weighted magnetic resonance imaging (DWI MRI) showed (Figure 1) a bilateral frontal, RT occipital and RT cerebellar hyperintensity with apparent diffusion coefficient (ADC) mismatch, compatible with the new ischemic event. He had high blood pressure for 10 years, maintained on captopril 25 mg, twice daily with good compliance. The highest blood pressure was 160/80 mmHg and usual blood pressure is 130/70 mmHg. He had been diabetic for five years, maintained on metformin 500 mg twice daily. Personal and social history is non-contributory. There is no family history of heart disease, liver cancer and stroke. On physical examination, he was conscious and had stable vital signs. He had no neck vein engorgement, and no carotid bruit. Chest examination was normal. He had adynamic precordium, normal rate and regular rhythm, no murmur. Abdomen was flat, soft and non-tender with normal liver and spleen. Extremities had normal findings. Muscle strength was 4/5 in both left upper and lower extremities and 4/5 in right upper and 2/5 over right lower extremity. All deep tendon reflexes were normal and plantar response was bilateral extensor. On the 7th day after admission, he experienced severe epigastric pain without radiation that was not relieved by antacids. His pain was an intermittent, occurring two to three times per week, with a duration of 10 - 15 minutes each. Carotid duplex scan result showed approximately 1% - 15% stenosis in both internal carotid arteries and common carotid arteries. Transthoracic two-dimensional echocardiography and transesophageal echo (TEE) did not show any significant valvular lesions or an intramural thrombus. Chest radiograph was essentially normal and further workup revealed elevated transaminases and alkaline phosphatase. CA 19-9 was 52,065 U/mL (Normal value: 0 - 33 U/mL). CT scan of the abdomen (Figure 2) showed multiple hypodensities in both lobes of the liver and heterogeneous hypodensity was seen in pancreas, that was highly suggestive of pancreas adenocarcinoma. According to the oncology consultation, a biopsy was done and pancreatic cancer finally was diagnosed based on abdominal CT, elevated CA 19-9 and biopsy finding. He was undergoing chemotherapy but eventually succumbed two months after discharge.
Axial Diffusion Weighted Magnetic Resonance Imaging Shows Reduced Diffusion in Right and Left Cerebellar Hemispheres; A, and multiple hypersignalities in bilateral frontal and parietal lobes compatible with ischemic stroke (B and C).
Spiral Abdominal Computerized Tomography with Contrast Shows Heterogenous Lesion with Enhancement in Pancreas (A and B) and Multiple Hypodensities with Enhancement in the Liver (C and D)
We obtained the written informed consent from the patient for publication of the case report.”
3. Discussion
Malignancies cause cerebrovascular complications with different mechanisms including direct effect of the tumor, complication of chemotherapy, metastasis and rarely paraneoplastic disorder. Trousseau syndrome is a paraneoplastic phenomenon due to activation of Coagulation by the malignant tumors such as pancreatic, lung and ovarian cancers (6, 7). These tumors are usually Mucin producing adenocarcinomas (8). Sack and colleague reported that 40 percent of Trousseau syndrome is due to pancreatic cancer as the most common cause (9); whereas Cestari and colleagues showed that Lung cancer causes 30 percent of cases (10). Chen et al. reported a patient with myocardial and cerebral infarction as an initial presentation of pancreatic adenocarcinoma (11). Our patient had no any marker for a cancer on his history unless abdominal pain and acute ischemic stroke. Due to multiple ischemic lesions in different ages and bihemispheric on his brain MRI, we extensively investigated to find an etiology, but carotid and vertebral dopplex and TEE did not find any vascular occlusion, cardiac thrombosis and vegetation. This subject made us consider thrombosis as a cause of stroke. During malignancy work-up for occult cancer ultimately we found a mass lesion in abdominal CT in favor of pancreatic cancer. Most pancreatic cancers are histologically invasive ductal carcinomas that invade surrounding tissues. It is rarely diagnosed in early stages, for this reason in most cases is largely incurable. The average survival time of Trousseau syndrome patients after cerebral infarction is reportedly 4.5 month. The first step in treating Trousseau’s syndrome is to eliminate the underlying tumor to reduce the risk of recurrence, but it is not always possible because in many cases, the tumor is unresectable. Heparin is the preferred treatment in this condition. Heparin can activate both activated factor Xa and thrombin, thereby preventing thrombosis, as well as, preventing mucin binding to P- and L-selectin and secondary platelet activation (12). Walsh-McMonagle and colleagues showed that heparin is effective in the treatment and prevention of thrombophlebitis in patients with cancer (13).
As a conclusion, multiple cerebral infarction may be the first manifestations of an undiagnosed occult cancer. If there is multiple infarctions in both anterior and posterior circulation of brain or in the bihemispheric, hypercoagulability situations due to the occult malignancy in a patients with an unknown etiology, should be considered.
3.1. Conclusion
Stroke as the first presentation of pancreatic cancer is rare. But in the cases of multiple infarctions in different parts of the brain, without evidence of common causes, trousseau syndrome and hypercoagulability state should be considered.
Acknowledgements
References
-
1.
Varki A. Trousseau's syndrome: multiple definitions and multiple mechanisms. Blood. 2007;110(6):1723-9. [PubMed ID: 17496204]. https://doi.org/10.1182/blood-2006-10-053736.
-
2.
Kwon HM, Kang BS, Yoon BW. Stroke as the first manifestation of concealed cancer. J Neurol Sci. 2007;258(1-2):80-3. [PubMed ID: 17408695]. https://doi.org/10.1016/j.jns.2007.02.035.
-
3.
Callander N, Rapaport SI. Trousseau's syndrome. West J Med. 1993;158(4):364-71. [PubMed ID: 8317122].
-
4.
Graus F, Rogers LR, Posner JB. Cerebrovascular complications in patients with cancer. Medicine (Baltimore). 1985;64(1):16-35. [PubMed ID: 3965856].
-
5.
Prandoni P, Falanga A, Piccioli A. Cancer and venous thromboembolism. Lancet Oncol. 2005;6(6):401-10. [PubMed ID: 15925818]. https://doi.org/10.1016/S1470-2045(05)70207-2.
-
6.
Taccone FS, Jeangette SM, Blecic SA. First-ever stroke as initial presentation of systemic cancer. J Stroke Cerebrovasc Dis. 2008;17(4):169-74. [PubMed ID: 18589335]. https://doi.org/10.1016/j.jstrokecerebrovasdis.2008.01.007.
-
7.
Bell WR, Starksen NF, Tong S, Porterfield JK. Trousseau's syndrome. Devastating coagulopathy in the absence of heparin. Am J Med. 1985;79(4):423-30. [PubMed ID: 4050830]. https://doi.org/10.1016/0002-9343(85)90028-2.
-
8.
Sutherland DE, Weitz IC, Liebman HA. Thromboembolic complications of cancer: epidemiology, pathogenesis, diagnosis, and treatment. Am J Hematol. 2003;72(1):43-52. [PubMed ID: 12508268]. https://doi.org/10.1002/ajh.10263.
-
9.
Sack GJ, Levin J, Bell WR. Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic, and therapeutic features. Medicine (Baltimore). 1977;56(1):1-37. [PubMed ID: 834136]. https://doi.org/10.1097/00005792-197756010-00001.
-
10.
Cestari DM, Weine DM, Panageas KS, Segal AZ, DeAngelis LM. Stroke in patients with cancer: incidence and etiology. Neurology. 2004;62(11):2025-30. [PubMed ID: 15184609].
-
11.
Chen L, Li Y, Gebre W, Lin JH. Myocardial and cerebral infarction due to nonbacterial thrombotic endocarditis as an initial presentation of pancreatic adenocarcinoma. Arch Pathol Lab Med. 2004;128(11):1307-8. [PubMed ID: 15504074]. https://doi.org/10.1043/1543-2165(2004)128<1307:MACIDT>2.0.CO;2.
-
12.
Alderman CP, McClure AF, Jersmann HP, Scott SD. Continuous subcutaneous heparin infusion for treatment of Trousseau's syndrome. Ann Pharmacother. 1995;29(7-8):710-3. [PubMed ID: 8520087]. https://doi.org/10.1177/106002809502907-812.
-
13.
Piatek C, O'Connell CL, Liebman HA. Treating venous thromboembolism in patients with cancer. Expert Rev Hematol. 2012;5(2):201-9. [PubMed ID: 22475288]. https://doi.org/10.1586/ehm.11.86.