Abstract
Introduction:
A neuroendocrine tumor has known as a neuroendocrine system tumor. Rarely, neuroendocrines have found in other areas, like the liver, gallbladder, bile ducts, kidneys, ovaries or testicles.Case Presentation:
We have a 41-year-old woman has referred to our medical center, complaining of fullness and vague pain on her right upper quadrant. The liver scan, sonography, MRI demonstrated multi lobular cysts in 6th and 7 th seg-ments of her liver and chest imaging was normal, oc-terotid scan has not shwon metastatic neuroendocrine tour of liver.Conclusions:
Liver could be the location of metastatic neuroendo-crine tumors, for example metastatic carcinoid tumor. Therefore, it was so important to diffrentatiate pri-mary neuroendocrine tumor from metastatic neuro-endocrine tumors.Keywords
1. Introduction
Neuroendocrine tumors have extremely been rare in liver. Totally, 151 cases have reported since now. Primary hepatic neuroendocrine tumors (PHNT) were a rarity, but represented about 0.3% of all neuroendocrine tumors (1). Therefore, the clinical features and treatment results have not well recognized. Of all GI tract neouroendocrine tumors, the most common were those of the small bowel (45%) (2).
Neuroendocrine tumors have initiated in peptide and Amin producing tissues. Histological confirmation of a primary neuroendocrine tumor of liver (PNTL) has needed as well as the exclusion of disease elsewhere. Most common area of neuroendocrine tumors would be gastro pancreatic region. However, primary tumors in liver were extremely rare. Because it was so rare, staging and prognosis for primary neuroendocrine tumor of liver have not well known. Imaging for diagnostic guide were Ultrasound, CT, and MRI. Until now, surgical resection has thought to be the most effective treatment for primary neuroendocrine tumor of liver (3, 4). Here, we have reported a right hepatic lobectomy for patient diagnosed as a PNTL.
2. Case Presentation
A 41-year-old woman has referred to our medical center, complaining of fullness and vague pain on her right upper quadrant. Her symptoms have initiated one year ago. Her pain has worsens after eating. The pain has occasionally radiated to her back between her scapulae. Patient has not complained of fever, nausea, vomiting or jaundice.
Her assessment has continued by liver sonography and abdominal CT scan and octerotid scan.
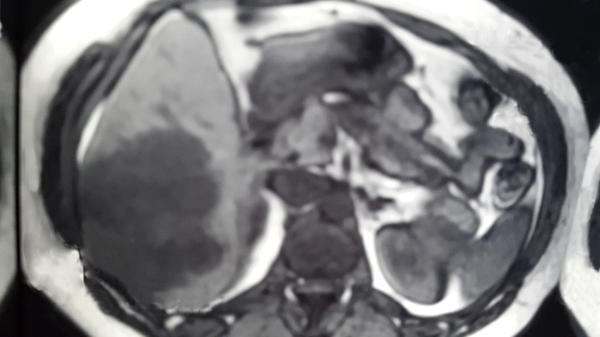
Sonography has demonstrated multi cystic lesion in lever, suggestive for “Hydatid cyst”. Abdominal CT scan has revealed multi cystic lesion in right liver lobe, measuring about 100 × 68 mm (Figures 1 and 2). This finding was compatible with “hydatid cyst” or “cyst adenoma”. Retroperitoneal area and pancreas appears normal. MRI demonstrated multi lobular cysts in 6th and 7 th segments of her liver and chest imaging was normal, octerotid scan has not shwon metastatic neuroendocrine tour of liver.
Multi Cystic Lesion in Right Liver Lobe

Multi Cystic Lesion in Right Liver Lobe
Cholecystectomy has performed on her 5 years ago, because of symptomatic cholelithiasis. Patient has occasionally taken oral contraceptive pills.
Immunogenic tests results were negative for hydatid cyst. Mammography has shown benign changes, thyroid scan was normal.
The patient has volunteered for hepatic resection due to these findings. Right hepatic lobectomy has performed; pathologic result has revealed well differentiated neuroendocrine neoplasm (G2).
Every single neuroendocrine tumor had considerable potential for malignancy. These tumors have well differentiated neuroendocrine tumors classified as caracinoid tumors. They might appear as poorly differentiated or mixed.
2.1. Treatment and Outcomes
Patient has undergone conservative surgery. Permanent pathology has shown that surgical margins were tumor free. Classic right hepatectomy has performed on the patient, tumor was nonfunctional, and therefore, there was no need to hormonal treatment such as somatostatin.
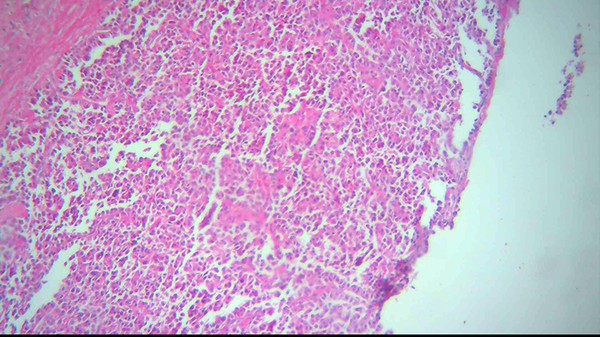
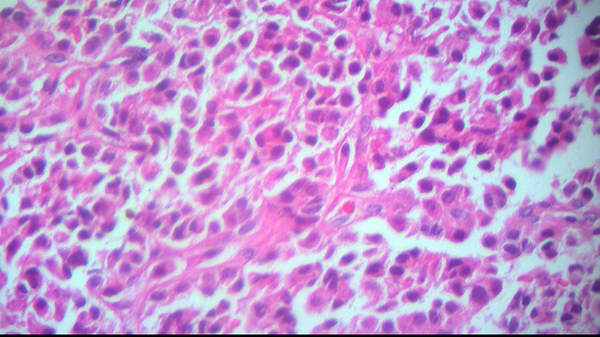
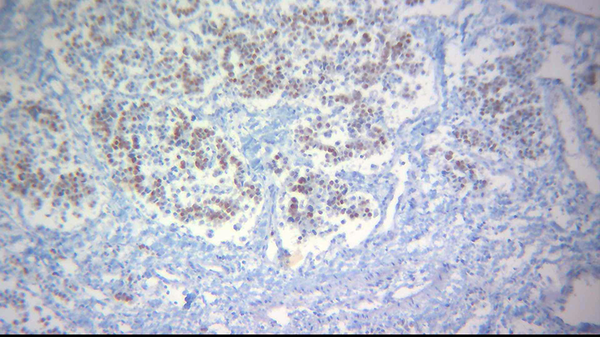
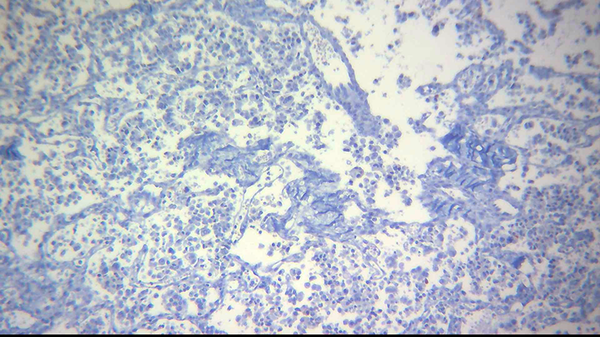
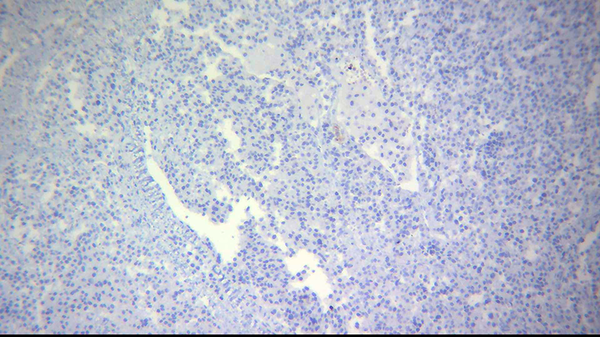
Pathologic report after tumor resection (right lobectomy) was well differentiated neurendocine neoplasm findings have shown mildly atypical cells with small and pepper nuclei and eosinophilic cytoplasm arranged in trabecular and glandular pattern with some nest formation. Few mitotic figures hemorrhage and foci of necrosis have seen. Immunohistochemistry has done after tumor resection ki 67 was positive in about 3% of tumoral cells, ck7 was positive, TTf1 and ck20 were negative. Synaptophysin and chromogranin were positive (Figures 3 - 7).
Post op period was uneventful, patient symptoms disappear entirely.
Neuroendocrine Tumor of Liver (Low Magnification) has Shown Sheets of Uniform Small and Bland Tumor Cells
High Power Examination Has Shown Loosely Cohesive Uniform Cells Which Had a Round to Oval Stippled Nucleus and Scant and Pink Granular Cytoplasm
IHC Study for CK 7 has Shown Diffuse and Strong Immunoreactivity
IHC Study for TTF-1 was Negative
IHC Study for ck 20 was Negative
3. Discussion
Neuroendocrine tumor of liver has known as a rare tumor of liver. There was few study about its symptoms, treatment and outcome.
Neuroendocrines have often grown slowly, and it might be several years before the symptoms have appeared and the tumor has diagnosed.
Liver could be the location of metastatic neuroendocrine tumors, for example metastatic carcinoid tumor. Therefore, it was so important to diffrentatiate primary neuroendocrine tumor from metastatic neuroendocrine tumors. Octreotide scan was 90% sensitive in metastatic neuroendocrine tumor of liver. Otherwise, octretide scan was not sensitive for primary neuroendocrine tumor of primary tumors in liver was extremely rare. They were typically metastatic tumors. Primary tumors have usually originated from biliary tracts, lead to neuroendocrine tumors in liver. Hepatic resection was a treatment of choice for neuroendocrines tumor of the liver (5). Neuroendocrine tumors, have although considered slow growing tumors and mildly aggressive, tend to develop distant metastatic disease with relative frequency, and the liver was the most affected organ (6). For patients with restricted but unresectable liver disease, transplantation has appeared to be the best therapeutic alternative (7). Complete surgical resection (Rt lobe hepatectomy) of liver tumor has achieved, although the operation with curative intent has intended in this patient. The percentage of incomplete resection was due to the low sensitivity of preoperative diagnostic methods (8).
In suspicion cases use of intraoperative ultrasonography has known as a great importance, and guide to surgeon for margin free of tumor. Surgical resection has needed not only for curative purposes but also for symptom relief by cytoreduction (9, 10).
WHO has classified neuroendocrine tumors in three classes: low grade (G1). Intermediate grade and high grade (G3).
The prolferative rate C mitotic index or ki.67 labeling rate was a critical factor for grading these neoplasms. Otherwise, in metastatic neuroendocrine tumors of GI system (G2), TNM classification has recommended. There was no specific classification for liver neuroendocrine tumors. The liver could be the primary origin of neuroendocrine tumors, and if the tumors have diagnosed as primary hepatic neuroendocrine tumors, surgical resection must be considered for curative treatment (11).
Acknowledgment
None declared.
References
-
1.
Caplin ME, Buscombe JR, Hilson AJ, Jones AL, Watkinson AF, Burroughs AK. Carcinoid tumour. Lancet. 1998;352(9130):799-805. [PubMed ID: 9737302]. https://doi.org/10.1016/S0140-6736(98)02286-7.
-
2.
Fenoglio LM, Severini S, Ferrigno D, Golle G, Serraino C, Bracco C, et al. Primary hepatic carcinoid: a case report and literature review. World J Gastroenterol. 2009;15(19):2418-22. [PubMed ID: 19452590].
-
3.
Knox CD, Anderson CD, Lamps LW, Adkins RB, Pinson CW. Long-term survival after resection for primary hepatic carcinoid tumor. Ann Surg Oncol. 2003;10(10):1171-5. [PubMed ID: 14654473].
-
4.
Zhang A, Xiang J, Zhang M, Zheng S. Primary hepatic carcinoid tumours: clinical features with an emphasis on carcinoid syndrome and recurrence. J Int Med Res. 2008;36(4):848-59. [PubMed ID: 18652782].
-
5.
Spolverato G, Vitale A, Ejaz A, Kim Y, Cosgrove D, Schlacter T, et al. Net health benefit of hepatic resection versus intraarterial therapies for neuroendocrine liver metastases: A Markov decision model. Surgery. 2015;158(2):339-48. [PubMed ID: 25999251]. https://doi.org/10.1016/j.surg.2015.03.033.
-
6.
Valadares LJ, Costa Junior W, Ribeiro HS, Diniz AL, Coimbra FJ, Herman P. Resection of liver metastasis from neuroendocrine tumors: evaluation of results and prognostic factors. Rev Col Bras Cir. 2015;42(1):25-31. [PubMed ID: 25992697]. https://doi.org/10.1590/0100-69912015001006.
-
7.
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R, et al. Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol. 2014;15(1):e8-21. [PubMed ID: 24384494]. https://doi.org/10.1016/S1470-2045(13)70362-0.
-
8.
Elias D, Lasser P, Ducreux M, Duvillard P, Ouellet JF, Dromain C, et al. Liver resection (and associated extrahepatic resections) for metastatic well-differentiated endocrine tumors: a 15-year single center prospective study. Surgery. 2003;133(4):375-82. [PubMed ID: 12717354]. https://doi.org/10.1067/msy.2003.114.
-
9.
Osborne DA, Zervos EE, Strosberg J, Boe BA, Malafa M, Rosemurgy AS, et al. Improved outcome with cytoreduction versus embolization for symptomatic hepatic metastases of carcinoid and neuroendocrine tumors. Ann Surg Oncol. 2006;13(4):572-81. [PubMed ID: 16511671]. https://doi.org/10.1245/ASO.2006.03.071.
-
10.
Chambers AJ, Pasieka JL, Dixon E, Rorstad O. The palliative benefit of aggressive surgical intervention for both hepatic and mesenteric metastases from neuroendocrine tumors. Surgery. 2008;144(4):645-51. [PubMed ID: 18847650]. https://doi.org/10.1016/j.surg.2008.06.008.
-
11.
Park CH, Chung JW, Jang SJ, Chung MJ, Bang S, Park SW, et al. Clinical features and outcomes of primary hepatic neuroendocrine carcinomas. J Gastroenterol Hepatol. 2012;27(8):1306-11. [PubMed ID: 22414232]. https://doi.org/10.1111/j.1440-1746.2012.07117.x.