Abstract
Background:
Breast cancer is the biggest risk factor that endangers women's health. It is considered the highest stress-causing disease due to the unpleasant effects of disease on different aspects of patients’ life. Breast cancer is commonly associated with the symptoms of post-traumatic stress and its comorbidities such as anxiety and depression. It appears that time perspective therapy (TPT), as a new psychological treatment, can reduce the symptoms of post-traumatic stress, anxiety, and depression in females with breast cancer.Methods:
This is a randomized controlled trial conducted from February to September 2019. A total of 30 patients with breast cancer were selected through a convenience sampling technique and were randomly divided into the control and treatment groups. The latter group attended 6-week sessions (each session lasted 90 minutes long) to receive TPT. To conduct pretest and posttest, all participants in the two groups were asked to fill out the following questionnaires: (1) Zimbardo Time Perspective Inventory (ZTPI); (2) The Post-traumatic Stress Disorder Checklist (PCL); (3) Beck Anxiety Inventory (BAI); and (4) the second version of Beck Depression Inventory (BDI-II). The analysis of covariance (ANCOVA) was used to evaluate the effects of treatment. A P-value smaller than 0.05 was considered significant.Results:
Data analysis of 28 patients from the experimental and control groups showed that TPT significantly reduced the symptoms of post-traumatic stress, anxiety, and depression in the treatment group (P < 0.001 for symptoms of post-traumatic stress and anxiety, and P = 0.002 for depression). Such a difference was not seen in the control group.Conclusions:
TPT may be an effective approach to reduce symptoms of post-traumatic stress, anxiety, and depression in Iranian women with breast cancer. Further investigations are required to confirm these findings, which may in turn help heath care professionals use TPT to promote the mental health of females with breast cancer.Keywords
Time Perspective Therapy Breast Cancer Post-traumatic Stress Anxiety Depression
1. Background
As a chronic and life-threatening disease, breast cancer can cause considerable psychological distress in patients. Among females, breast cancer is the most commonly diagnosed cancer in Iran and worldwide. Based on the international data, breast cancer accounts for 11.6% of cancer cases and it is responsible for 6.6% of cancer deaths (1, 2). As a result of such a disease, short-term side effects (such as hair loss, nausea, and vomiting, weight loss) and long-term side effects (such as chronic pain, sleep disorders, sexual problems, cognitive defect, loss of function) can be developed (3, 4). The bodies and identities of women are both affected by mastectomy surgeries or other breast surgery opinions, which lead to essential psychological consequences, such as depression and anxiety (5, 6). Studies revealed that 50% of patients with breast cancer developed symptoms of depression and anxiety within the first year of disease diagnosis (7). Being diagnosed with breast cancer, which follows a tolerance of long-term and difficult treatments, uncertainty about recurrence and metastasis, as well as the high likelihood of death are typically considered stressful experiences that lead to the diagnosis of symptoms of post-traumatic stress in patients with breast cancer (8). The publication of the diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV) in 1994 has led to an agreement on the life-threatening nature of cancer and its role as a stressful factor in provoking symptoms of post-traumatic stress (9). For those who have gone through a traumatic experience, symptoms of post-traumatic stress are considered a set of thoughts, emotions, behaviors, and attitudes. Such an experience is recognized as a significant danger, life-threatening problem, or strong injury, which contributes to severe fear, helplessness, depression, and anxiety (10). The incidence of breast cancer suggests the existence of a distinct stressor within the framework of post-traumatic stress disorder (PTSD) as the stress caused by the disease itself is evoked by an internal event rather than an external threat. This disease characteristic implies that the patient fails to avoid the stress factor due to the person’s internal condition (11). Since breast cancer is not an urgent and immediate threat to bodily integrity, the person’s worries arise from future events. Thus, breast cancer-related symptoms of post-traumatic stress are different from other types of external traumatic events, which are typically discrete and urgent threats (12).
Following the improvement in breast cancer diagnosis and treatment, the number of women who have completed their treatment and survived has significantly increased during the last years. The breast cancer-related symptoms of post-traumatic stress, anxiety, and depression may persist for some months or years after completion of therapy. These symptoms cause noticeable disruption in the life of patients and decrease their survival period by intensifying the symptoms of disease, establishing and reinforcing unhealthy behaviors, reducing adherence to medical treatment, having poor awareness about the treatment advice, and worrying too much about the side effects of treatment. Reports indicate intensified symptoms and increased mortality in cancer patients with depression (13, 14). Also, anxiety and stress contribute to tumor development, progression, and metastasis by weakening the immune system. It is, thus, vital to consider the psychological consequences of breast cancer in patients in the case of increased survival period (15, 16).
One therapeutic approach is time perspective therapy (TPT), which has recently been applied for treating patients with PTSD. TPT is a time-based therapeutic approach, which offers 5 time perspectives, focusing on patients' perception of their past, present, and future: past-positive, past-negative, present hedonism, present fatalism, and future (17). According to the time perspective theory, when these 5 time perspectives deviate from the balance to past-negative or present fatalism orientation, it would cause PTSD, as well as anxiety and depression in patients. Thus, when patients are treated with TPT, they recognize those negative self-talks that expose them to traumatic experiences and attempts to alter them by focusing on past-positive events. Such treatment helps patients create a more positive perspective of their life and have a hopeful view of the future (18). Throughout the psychological well-being promotion of patients, TPT diminishes the symptoms of both PTSD and anxiety and depression by weakening past-negative attitudes and present fatalism, improving the past-positive, present hedonistic, and future perspectives, and, creating a balanced time-perspective (19).
It has been documented that TPT significantly reduced the symptoms of post-traumatic stress both in soldiers and veterans of wars (20). According to a study that was conducted on female students, the participants, who were treated by TPT, showed considerably reduced symptoms of depression (21). There is also evidence of a meaningful correlation of past-positive, present hedonistic, and future perspectives with personal responsibility with healthcare, nutrition, and spiritual growth in patients with cardiac disease (22). TPT was devised primarily to address the PTSD-related emotional difficulties and, consequently, previous research on its efficacy has mostly focused on patients with PTSD. However, as new evidence has drawn attention toward the traumatic nature of cancer diagnosis, this treatment may be beneficial in alleviating the relevant symptoms in patients with cancer. To the best of our knowledge, no study has investigated the potential benefits of TPT among patients with cancer.
2. Objectives
This randomized controlled trial aimed at investigating the efficacy of TPT in diminishing the symptoms of post-traumatic stress, anxiety, and depression in women with breast cancer within the first year following diagnosis.
3. Methods
A pretest-posttest control group design was used to investigate the effect of the independent variable in the current randomized controlled trial. The study was carried out at the Cancer Research Center of Shahid Beheshti University of Medical Sciences from February to September 2019. The inclusion criteria of this study included: (1) the diagnosis of breast cancer by a specialist in breast surgery (based on the patient’s medical record); (2) having significant clinical or subclinical symptoms of post-traumatic stress, anxiety, and depression as diagnosed by a clinical psychologist; (3) age between 25 and 55 years (since in Iran the considerable prevalence of breast cancer starts at the age of 25 years and reaches its highest level between 40 and 49 years (23), elder patients typically have more difficulty attending psychotherapy sessions and filling out questionnaires); (4) general literacy (e.g. reading, writing, etc.); (5) at least 1 month following the diagnosis of breast cancer; (6) no history of using psychological and psychiatric services until the time of participation in this study; (7) no history of other types of physical and mental illnesses (based on MMPI-2); (8) regular attendance at psychotherapy sessions by the treatment group; (9) and completion of the written consent form. The exclusion criteria included: (1) being absent in 2 psychotherapy sessions; (2) receiving other types of psychological and psychiatric services during the treatment period; (3) disease recurrence or metastasis during the study or incidence of a physical problem that causes difficulty in attending the psychotherapy sessions; (4) and not willing to participate anymore.
3.1. Sample Size Determination, Randomization, and Procedure
A power analysis was conducted in G*Power software. Considering that our analytic strategy was to use analysis of covariance (ANCOVA) to evaluate the effect of treatment, it seemed best to determine the sample size based on this method. Assuming a partial eta-squared of 0.25 for the grouping factor (which corresponds to a Cohen’s d of 0.34, given a pretest-posttest correlation of 0.8 and equal group size for the formula for calculating Cohen’s d from ANCOVA), we need a sample size of 26 to reach a statistical power of 0.8. Based on this power analysis and considering a 15% attrition, a sample of 30 would be sufficient (24).
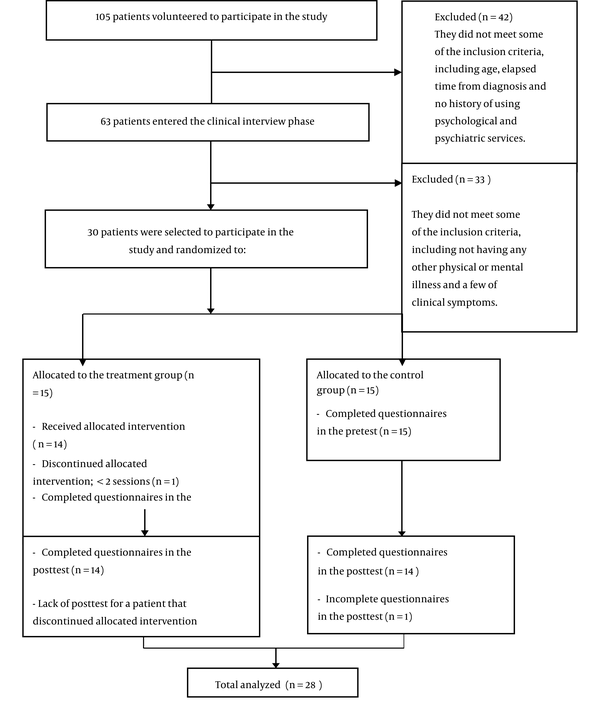
For carrying out the current experimental research, 30 females with breast cancer, who had undergone treatment at the Cancer Research Center, were selected by considering the inclusion criteria. A convenience sampling method was applied in this study and the participants were screened by a clinical psychologist; those who met the criteria and signed a written informed consent were allocated to either treatment or control group, using the random number table. During the research, a patient could not attend the regular psychotherapy sessions due to the disease exacerbation and patient hospitalization. The data of the patient were, therefore, excluded from the analytic procedures. Also, the data related to a patient in the control group were excluded from the analysis, as many questions in each questionnaire were left unanswered by the patient (Figure 1).
CONSORT diagram of participants’ progress through each phase of the study
3.2. Treatment
In the current study, the efficacy of TPT is investigated in 14 patients with breast cancer through a clinical diagnosis of symptoms of post-traumatic stress, anxiety, and depression. Each participant of the treatment group attended 6 individual psychotherapy sessions. All sessions lasted 90 minutes and were held every week (once per week). The treatments were carried out every morning on 3 patients undergoing TPT. Pretest and posttest were performed in both the control and treatment groups in the interval between two chemotherapy sessions to reduce the consequences affecting the accuracy of the test material's completion. All psychotherapy sessions were held based on the protocols developed by Zimbardo et al. (17) and Sword et al. (25). The process of TPT involves creating a therapeutic relationship, assessing psychological symptoms, examining patient’s attitudes toward the past, present, and future, giving patients insight as to how each time perspective develops and maintains psychological symptoms and, eventually, treating patient's time attitudes to establish a balanced time perspective. Along with the careful implementation of the therapeutic protocol, the present research used patients, whose similar cancer had been cured as the models in the final psychotherapy session when the researcher attempted to modify the future time perspective. An in-depth description of the therapeutic protocol is presented in Table 1.
Structure and Content of TPT Sessions and Home Practice
| Sessions | Values |
|---|---|
| Session 1 | Content: Establishing and strengthening a therapeutic relationship by focusing on the elements related to post-traumatic stress disorder, the theory of time, and TPT principles; teaching patients deep breathing and muscle relaxation techniques. |
| Practices: Carrying out deep breathing and muscle relaxation exercises when feeling stressed and anxious. | |
| Session 2 | Content: Implementing ZTPI, PCL, BAI, and BDI-II questionnaires, and examining a patient’s time perspective based on the ZTPI test. |
| Practice: Watching the River of Time video. | |
| Session 3 | Content: Sharing the results of psychological tests with patients; defining both past negative and positive to a patient and examining the patient’s status in these time perspectives; making efforts to replace a past-negative attitude with a past-positive one. |
| Practice: Attempt to remind and note positive events that patients experienced or carried out in the past. | |
| Session 4 | Content: Describing both present hedonism and fatalism, examining the patient’s status in these time perspectives, and attempting to alter present fatalism to become a responsible present hedonist deliberately. |
| Practice: Performing the activities that are pleasurable for the patient and, at the same time, are not irresponsible and traumatic. | |
| Session 5 | Content: Defining a positive future for a patient and trying to change a negative future perspective with a positive one; setting up discussions to establish short-term and long-term goals. |
| Practice: Writing detailed and realistic short-term and long-term goals. | |
| Session 6 | Content: Analyzing a patient’s chosen short-term and long-term goals; tracking patient’s progress from the first session to the present time; creating a balance among a patient’s time perspectives; concluding a session and asking patients to fill out the questionnaires once more. |
| Practice: Regularly and continuously performing deep breathing and muscle relaxation tasks following the completion of the psychotherapy sessions; carrying out the activities that are pleasurable for the patient, which is not irresponsible and traumatic. |
3.3. Outcomes and Measurement Tools
A demographic checklist (containing age, marital status, education, job, economic status, stage of the disease, and type of therapy) was used in this study.
3.3.1. The Post-traumatic Stress Disorder Checklist
The Post-traumatic Stress Disorder Checklist (PCL) is a self-report scale, which was developed by Weather et al. in 1993, based on the diagnostic criterion of DSM. The test includes 17 items, which offer the examinee a 5-point Liker Scale. The total score range is 17 to 85 with a score of 50 or higher, indicating the presence of PTSD in the patient. Weather et al. documented test-retest reliability of 0.96, internal consistency of 0.97, and overall of 0.62 to 0.87 for item-test correlation of the PCL (26). This questionnaire was translated to Persian by Hagh-Shenas et al. and is known as ESHEL. The ESHEL showed adequate validity and reliability (27).
3.3.2. Beck Anxiety Inventory
Beck Anxiety Inventory (BAI) is a self-report test, which was formed to assess the levels of anxiety. The BAI contains 21 items with 4 different choices for every question. The scoring of the scale ranges from 0 for never to 3 for severe. Thus, a total score of 0 to 63 will be obtained. A score of 0 to 7 indicates the absence of anxiety in the examinee, while a score of 8 to 15 shows mild anxiety, 6 to 25 implies moderate anxiety, and a score of 26 to 63 denotes severe anxiety of the examinee. A high internal consistency value has been documented for the BAI (α = 0.92). Some evidence shows that the test-retest reliability of the questionnaire was r (81) = 0.75 for a week (28). In a study on the Iranian population, a validity coefficient of 0.72, a test-retest validity coefficient of 0.83 for a one-month interval, and an internal consistency of 0.92 were obtained for the BAI based on Cronbach's alpha calculation (29).
3.3.3. Beck Depression Inventory-II
The first version of the Beck Depression Inventory (BDI) was developed by Aaron Beck in 1961 and the second version of such scale (BDI-II) was published by Beck, Steer, and Brown in 1996. The current research uses the BDI-II, which encompasses 21 items, each measuring one of the depression symptoms (cognitive, emotional, and physical). Each item is scored from 0 to 3. Scoring 0 for each item indicates the presence of depression symptoms and the score of 3 suggests the existence of severe symptoms. The BDI-II total score ranges from 0 to 63. Beck et al. have found an internal consistency ranging from 0.73 to 0.93 based on Cronbach's alpha coefficient and a test-retest reliability coefficient ranging from 0.48 to 0.86 for this questionnaire (30). Studies in Iran have obtained a Cronbach's alpha coefficient of 0.91, a split-half correlation coefficient of 0.89, and a retest coefficient of 0.94 with a one-week interval for the BDI-II, and found a value of 0.93 for the correlation of BDI-II with its first version (31).
3.3.4. Zimbardo Time Perspective Inventory
The time perspective inventory was developed by Zimbardo and Boyd in 1995. It contains 56 items, which are scored on a 5-point Likert Scale ranging from “totally agree” to “totally disagree”. The former indicates the examinee’s full agreement and the latter implies the total disagreement of the examinee. This scale encompasses such time perspectives as past-negative, past-positive, present hedonism, present fatalism, and future. The reported Cronbach’s alpha by Zimbardo and Boyd was 0.82 for past-negative, 0.80 for past-positive, 0.79 for present hedonism, 0.74 for present fatalism, and 0.77 for future time perspective (32). The construct and face validity of the questionnaire, as well as the reliability of this scale, have been confirmed in several studies (33).
3.4. Data Analysis
The analysis of data was carried out, using SPSS ver. 25. ANCOVA was used to investigate the treatment efficacy of the target variables. The pretest scores were entered as a covariate into the model to control their effects to compare the difference between the mean scores of the posttest in the two groups. The assumptions for ANCOVA were assessed thoroughly to ensure valid inference. When one assumption was violated, a useful method (e.g. bootstrapping method or outlier removal) was performed to ensure that the violated assumption causes no effect on the results of the study. Shapiro-Wilk test was used in the current study to examine the normality of the residual errors in the model. Also, Levene's test was used to assess the homogeneity of (error) variance, and the scatter plot was used to study whether the dependent variable is linear. To evaluate the homogeneity of regression slopes in two groups, an examination of group factors and interactions between pretest and posttest was performed. Moreover, the presence of outliers in data was studied by calculating standardized residuals.
4. Results
Thirty participants were enrolled in this study. Two participants were dropped out, one from the treatment group due to disease recurrence and one from the control group due to incomplete data on the posttest. The data of 28 patients were analyzed. The current study involved 28 patients with stage 1, 2, or 3 breast cancer. The median age of participants in the treatment and control groups was 40.5 and 40.9 years of age, respectively. Other demographic characteristics of the patients in both control and treatment groups are represented in Table 2. The mean and standard deviation of the pretest and posttest scores in anxiety, depression, symptoms of post-traumatic stress, and time perspective dimensions in the control and treatment groups are demonstrated in Table 3.
Demographic and Clinical Characteristics of Women with Breast Cancer in the Intervention and Control Groups a
| Demographic Characteristics | Treatment Group | Control Group |
|---|---|---|
| Age | 14 (100); 40.5 ± 7.5 | 14 (100); 40.9 ± 6.8 |
| Marital status | ||
| Married | 12 (86) | 11 (79) |
| Unmarried | 2 (14) | 3 (21) |
| Education | ||
| High school | 5 (36) | 4 (28) |
| Diploma degree | 1 (7) | 4 (28) |
| Bachelor degree | 6 (34) | 5 (36) |
| Master degree | 2 (14) | 1 (7) |
| Job | ||
| Housewife | 10 (71) | 9 (64) |
| Employee | 4 (29) | 4 (29) |
| Student | 0 (0) | 1 (7) |
| Economic status | ||
| Good | 3 (21) | 5 (36) |
| Average | 8 (58) | 4 (28) |
| Bad | 3 (21) | 5 (36) |
| Stage of cancer | ||
| I | 4 (29) | 7 (50) |
| II | 10 (71) | 6 (43) |
| III | 0 (0) | 1 (7) |
| Type of treatment | ||
| Chemotherapy | 10 (70) | 12 (85) |
| Combination | 4 (30) | 2 (15) |
The Mean and Standard Deviation of Pretest and Posttest Scores of Clinical Variables and Process Variables in Treatment and Control Groups
| Variables | Treatment Group | Control Group | ANCOVA Test for Treatment Effect |
|---|---|---|---|
| PTSS | < 0.001 b | ||
| Pretest | 48.00 ± 3.258 | 46.14 ± 5.362 | |
| Posttest | 36.86 ± 2.445 | 45.21 ± 4.980 | |
| Anxiety | < 0.001 b | ||
| Pretest | 25.14 ± 2.033 | 23.36 ± 2.023 | |
| Posttest | 18.64 ± 1.865 | 22.64 ± 2.530 | |
| Depression | < 0.001 c | ||
| Pretest | 26.07 ± 4.969 | 26.14 ± 4.452 | |
| Posttest | 18.14 ± 3.997 | 29.14 ± 5.376 | |
| Past negative | 0.010 b | ||
| Pretest | 3.06 ± 0.434 | 3.17 ± 0.489 | |
| Posttest | 2.79 ± 0.517 | 3.17 ± 0.512 | |
| Past positive | < 0.001 d | ||
| Pretest | 3.40 ± 0.542 | 3.38 ± 0.571 | |
| Posttest | 3.66 ± 0.322 | 3.32 ± 0.530 | |
| Present hedonistic | < 0.001 | ||
| Pretest | 2.73 ± 0.098 | 3.00 ± 0.195 | |
| Posttest | 3.40 ± 0.175 | 2.84 ± 0.135 | |
| Present fatalistic | < 0.001 b | ||
| Pretest | 3.29 ± 0.450 | 3.11 ± 0.508 | |
| Posttest | 2.40 ± 0.371 | 3.45 ± 0.428 | |
| Future | < 0.001 | ||
| Pretest | 2.95 ± 0.273 | 3.28 ± 0.353 | |
| Posttest | 3.61 ± 0.212 | 3.03 ± 0.227 |
According to Table 3, the mean of the posttest scores in anxiety, depression, symptoms of post-traumatic stress, past-negative, and present fatalism scales was lower than the mean of pretest scores in the same scales. Also, the posttest mean scores in present hedonism, past-positive, and future perspective were higher than the pretest mean scores in the same scales. Such differences were not found in the control group. Thus, the ANCOVA method was used to investigate whether these differences are meaningful.
4.1. Primary Outcomes
Table 3 shows the results of ANCOVA, which are related to the clinical variables. According to Table 3, the results of ANCOVA showed that the symptoms of post-traumatic stress and anxiety are significantly reduced in the treatment group after conducting the treatment (P < 0.001). Such a meaningful decrease can be seen for the variable of depression. Yet, there was a significant Pretest × Group interaction (P = 0.002), indicating that the treatment effect is moderated by the level of baseline depression, such that individuals with baseline scores above 12 were significantly improved by the treatment, while individuals with low baseline depression were not. According to the results of this study, the patients with breast cancer experienced lower symptoms of post-traumatic stress, anxiety, and depression than those in the control group after participating in the psychotherapy sessions based on TPT.
4.2. Secondary Outcomes
In the second part of Table 3, the results of ANCOVA, which are related to the variables of the treatment processes, show whether the treatment has successfully influenced the hypothesized processes of change, which is assumed to mediate the effect of treatment. All the ANCOVA assumptions were precisely examined for each of the clinical and procedural variables in Table 3. In the case where the assumption of homogeneity of regression slopes was violated, both the pretest (covariate) and the variable of the treatment group interaction were retained in the analyses. This occurred for past-positive and depression variables. In the case of violating other assumptions, the bootstrapping method was employed to ensure the accuracy of the study results. This was observed for the past-negative, present fatalism, anxiety, and symptoms of post-traumatic stress variables, and the related data were confirmed through the method of bootstrapping. According to Table 3, the variable of the treatment group impact on the past-negative was P = 0.010 and a value of P = 0.001 was found for such an impact on the present hedonism, present fatalism, and future scales. Also, for the past-positive time perspective, a P = 0.001 was obtained for the treatment. Yet, there was a significant pretest × group interaction (P = 0.005), indicating that the effect of treatment is moderated by the baseline level of past-positive perspective, with individuals with a lower level of baseline past-positive perspectives gaining more improvement. The results of ANCOVA showed that TPT significantly made differences between different time perspectives of patients in both control and treatment groups.
5. Discussion
In the present research, the efficacy of TPT in reducing symptoms of post-traumatic stress, anxiety, and depression in females with breast cancer was examined. The results suggest that treatments through the use of TPT can significantly affect the symptoms of post-traumatic stress, anxiety, and depression. To the best of our knowledge, no study has yet explored the effect of TPT on patients with breast cancer.
Previous research on the efficacy of TPT has provided evidence on its efficacy on post-traumatic stress symptoms in soldiers and veterans of wars (20). In another study on female students, the participants, who were treated by TPT, showed significantly lower depressive symptoms (21). The current study generalizes the evidence to patients with breast cancer as well, suggesting that TPT is effective in reducing post-traumatic stress, anxiety, and depression.
According to its underlying theory, TPT is effective because it facilitates the balance between different aspects of time-perspective, which in turn leads to the treatment effects. The present study showed that TPT significantly reduced past-negative and present fatalism in patients in the treatment group compared with those in the control group. Such a meaningful difference between the two groups was also observed in past-positive, present hedonism, and future perspectives as patients of the treatment group achieved higher scores in each of these scales than those in the control group. This study has also documented that patients with breast cancer, who experienced symptoms of post-traumatic stress, rarely recalled the incidence of the disease in the past and their cancer failed to significantly change the patients’ past perspective. Yet, these patients achieved high scores in the attitude of present fatalism and low scores in the present hedonistic attitude. It, therefore, appears that patients with breast cancer are unable to enjoy the present moment and have a weak tendency to carry out pleasurable activities.
The current research has also found that patients with breast cancer are extremely hopeless and skeptical about the future and have no plan. It seems that such desperation and pessimism arise from their fear of death, having a bad outcome, and the disease exacerbation or recurrence, which all play the main role in intensifying and preserving symptoms of post-traumatic stress, anxiety, and depression. Thus, the patients’ scores in the future attitude were low.
While the longitudinal link between the change in time perspectives and change in treatment outcomes has not yet been established, there is cross-sectional evidence linking these time perspectives to mental health conditions. For instance, Oyanadel and Buela-Casal compared a clinical sample of patients with mental disorders (depressive disorder, bipolar disorder, schizophrenia disorder, and cluster B personality disorder) to healthy controls in terms of 5 aspects of time perspectives and their deviation from a balanced time perspective. Their findings showed that the obtained scores in the deviation from the balanced time perspective (DBTP), past-negative, and present fatalism in all clinical groups were higher than the control group. The researchers also found that the mental health-related quality of life was negatively associated with deviation from a balanced time perspective and past-negative, and positively correlated with future time perspective (34).
A study on depressed and normal people has documented that patients with depression exhibited more past-negative attitudes, more present fatalism, and less present hedonism. The study revealed an association of depression and anxiety symptoms with past-negative and present fatalism (35).
Concerning the therapeutic protocol, the last psychotherapy session involved promoting the future time orientation through the establishment of short-term and long-term goals, as well as the prediction of a positive future. By having the fear of recurrence, metastasis, painful surgeries, and even death, patients suppose that the future looks dark and frightening, which is the underlying cause of symptoms of post-traumatic stress, anxiety, and depression. Thus, to create a picture of a bright and hopeful future that is sustainable, each of the patients met an individual with the same disease, whose cancer was cured. Cancer survivors spoke with the treatment group patients about experiences and emotions they had when living with this disease, and expressed the lessons from overcoming breast cancer. They also encouraged the participants to live life by emphasizing the importance of making efforts to preserve life and improve family relationships. After meeting the survivors, the participants truly believed that their disease could be treated and they could improve their overall health through medication adherence, as well as recognition and control of negative emotions. Previous studies have well documented the effect of living models on behavior (36, 37). It appears that the increase in the scores of the treatment group in the future time perspective was contributed to the meetings these patients had with similar and cured models.
Psychological, emotional, and social effects of a breast cancer diagnosis can contribute to the disease's medical impacts and cause mental psychological trauma in patients, such as depression, anxiety, and adjustment disorder, which negatively affect the patients’ quality of life (38). When the breast cancer-related symptoms of post-traumatic stress, as well as anxiety and depression outcomes in such a disorder, do not receive psychological intervention and treatment, it may result in intensified symptoms, prolonged recovery time, reduced medication adherence, poor treatment outcome, and tendency to death (8). Following the diagnosis of breast cancer, it is, thus, necessary to employ a psychotherapy method, which provides the most efficiency in the least possible time to support the psychological needs of patients. Through a 6-session therapeutic protocol via identifying the 5 time perspectives of patients to provide a balance among them, support a more positive orientation toward the future, and eventually change the patient to a healthy and efficient person, TPT has been shown to treat the symptoms of post-traumatic stress.
The current research still does not indicate whether both TPT and theory that arises from TPT have led to positive changes in patients' psychological symptoms. However, concerning the examination of TPT processes in the current study, evidence supports the hypothesis that TPT can be effective through the theory use, changes implementation in the patients’ 5 time perspectives, and balances establishment in past, present, and future time perspectives. In this investigation, TPT significantly affected the patients in the treatment group compared with those in the control group. Thus, one should not point out whether TPT is more effective than other treatment options. To confirm the results of this study, more evidence is required. Also, future studies are recommended to focus on TPT to compare its effectiveness with other types of therapy, which may result either in confirmation of the findings of this study or their correction.
5.1. Limitations
Some limitations should be noted, the most important of which was the small number of participants. As another limitation, those chemotherapy sessions frequently interfere with psychological treatment as the side effects of chemotherapy sometimes affected the results of psychological treatment. However, this research aimed at discovering solutions, from which active patients (undergoing treatment) can benefit. Also, some efforts were carried out in this study to prevent overlap in both of the sessions. An inevitable limitation in this study was the withdrawal of participants due to their condition. This research suggests preparing online facilitation for virtual counseling services for such participants. This method of treatment has sufficient flexibility, which can be applied based on the patient’s condition. It is, therefore, suggested to compare the effectiveness of this type of method with face-to-face techniques of treatment.
5.2. Conclusions
The findings of this study indicate that TPT may be an effective approach to reduce symptoms of post-traumatic stress, anxiety, and depression in Iranian women with breast cancer. Future studies are required to confirm these findings to allow common medical treatments to benefit from TPT to promote the psychological condition of females with breast cancer.
Acknowledgements
References
-
1.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. [PubMed ID: 30207593]. https://doi.org/10.3322/caac.21492.
-
2.
Fouladi N, Feizi I, Nadermohammadi M, Mehrara E, Adldoosti R, Alimohammadi S. The Predictors of Sexual Satisfaction among Iranian Women with Breast Cancer. Asian Pac J Cancer Prev. 2021;22(2):391-6. [PubMed ID: 33639652]. [PubMed Central ID: PMC8190366]. https://doi.org/10.31557/APJCP.2021.22.2.391.
-
3.
Cook SA, Salmon P, Hayes G, Byrne A, Fisher PL. Predictors of emotional distress a year or more after diagnosis of cancer: A systematic review of the literature. Psychooncology. 2018;27(3):791-801. [PubMed ID: 29318702]. [PubMed Central ID: PMC5873392]. https://doi.org/10.1002/pon.4601.
-
4.
Jim HS, Andrykowski MA, Munster PN, Jacobsen PB. Physical symptoms/side effects during breast cancer treatment predict posttreatment distress. Ann Behav Med. 2007;34(2):200-8. [PubMed ID: 17927558]. https://doi.org/10.1007/BF02872674.
-
5.
Fingeret MC, Nipomnick SW, Crosby MA, Reece GP. Developing a theoretical framework to illustrate associations among patient satisfaction, body image and quality of life for women undergoing breast reconstruction. Cancer Treat Rev. 2013;39(6):673-81. [PubMed ID: 23380309]. [PubMed Central ID: PMC3681916]. https://doi.org/10.1016/j.ctrv.2012.12.010.
-
6.
Hamidian P, Rezaee N, Shakiba M, Navidian A. The Effect of Cognitive-Emotional Training on Post-traumatic Growth in Women with Breast Cancer in Middle East. J Clin Psychol Med Settings. 2019;26(1):25-32. [PubMed ID: 29572619]. https://doi.org/10.1007/s10880-018-9561-z.
-
7.
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A. Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ. 2005;330(7493):702. [PubMed ID: 15695497]. [PubMed Central ID: PMC555631]. https://doi.org/10.1136/bmj.38343.670868.D3.
-
8.
French-Rosas LN, Moye J, Naik AD. Improving the recognition and treatment of cancer-related posttraumatic stress disorder. J Psychiatr Pract. 2011;17(4):270-6. [PubMed ID: 21775828]. [PubMed Central ID: PMC4365935]. https://doi.org/10.1097/01.pra.0000400264.30043.ae.
-
9.
Arnaboldi P, Riva S, Crico C, Pravettoni G. A systematic literature review exploring the prevalence of post-traumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory. Breast Cancer (Dove Med Press). 2017;9:473-85. [PubMed ID: 28740430]. [PubMed Central ID: PMC5505536]. https://doi.org/10.2147/BCTT.S111101.
-
10.
Yehuda R. Post-traumatic stress disorder. N Engl J Med. 2002;346(2):108-14. [PubMed ID: 11784878]. https://doi.org/10.1056/NEJMra012941.
-
11.
Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer. A conceptual and empirical review. Clin Psychol Rev. 2002;22(4):499-524. [PubMed ID: 12094509]. https://doi.org/10.1016/s0272-7358(01)00118-0.
-
12.
Cordova MJ, Riba MB, Spiegel D. Post-traumatic stress disorder and cancer. Lancet Psychiatry. 2017;4(4):330-8. [PubMed ID: 28109647]. [PubMed Central ID: PMC5676567]. https://doi.org/10.1016/S2215-0366(17)30014-7.
-
13.
Bower JE. Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol. 2008;26(5):768-77. [PubMed ID: 18258985]. [PubMed Central ID: PMC3057774]. https://doi.org/10.1200/JCO.2007.14.3248.
-
14.
Palesh O, Koopman C. Breast cancer: Post-traumatic stress disorder--prevalent and persistent. Nat Rev Clin Oncol. 2013;10(5):252-4. [PubMed ID: 23568418]. https://doi.org/10.1038/nrclinonc.2013.49.
-
15.
Rogers LQ, Courneya KS, Anton PM, Verhulst S, Vicari SK, Robbs RS, et al. Effects of a multicomponent physical activity behavior change intervention on fatigue, anxiety, and depressive symptomatology in breast cancer survivors: randomized trial. Psychooncology. 2017;26(11):1901-6. [PubMed ID: 27530961]. [PubMed Central ID: PMC5511085]. https://doi.org/10.1002/pon.4254.
-
16.
Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer. 2019;125(9):1417-31. [PubMed ID: 30768779]. [PubMed Central ID: PMC6467795]. https://doi.org/10.1002/cncr.31943.
-
17.
Ryback D. Review of "The Time Cure: Overcoming PTSD With the New Psychology of Time Perspective Therapy," by Philip G. Zimbardo, Richard M. Sword, and Rosemary K. M. Sword. Am J Fam Ther. 2013;41(5):452-4. https://doi.org/10.1080/01926187.2012.760962.
-
18.
McKay MT, Worrell FC, Zivkovic U, Temple E, Mello ZR, Musil B, et al. A balanced time perspective: Is it an exercise in empiricism, and does it relate meaningfully to health and well-being outcomes? Int J Psychol. 2019;54(6):775-85. [PubMed ID: 30206944]. https://doi.org/10.1002/ijop.12530.
-
19.
Boniwell I, Osin E, Sircova A. Introducing time perspective coaching: A new approach to improve time management and enhance well-being. Int J Evid Based Coach Mentor. 2014;12(2):24-40.
-
20.
Sword RM, Sword RK, Brunskill SR. Time Perspective Theory; Review, Research and Application. In: Stolarski M, Fieulaine N, van Beek W, editors. Time Perspective Therapy: Transforming Zimbardo’s Temporal Theory into Clinical Practice. Cham, Bavaria: Springer; 2015. p. 481-98. https://doi.org/10.1007/978-3-319-07368-2_31.
-
21.
Emsaki G, Karimian N, Nouri A. The Effectiveness of Time Perspective Therapy on Reducing Depressive Symptoms. Int J Psychol. 2018;12(1):81-90. https://doi.org/10.24200/ijpb.2018.55629.
-
22.
Hamilton JM, Kives KD, Micevski V, Grace SL. Time perspective and health-promoting behavior in a cardiac rehabilitation population. Behav Med. 2003;28(4):132-9. [PubMed ID: 14663920]. https://doi.org/10.1080/08964280309596051.
-
23.
Jazayeri SB, Saadat S, Ramezani R, Kaviani A. Incidence of primary breast cancer in Iran: Ten-year national cancer registry data report. Cancer Epidemiol. 2015;39(4):519-27. [PubMed ID: 26070507]. https://doi.org/10.1016/j.canep.2015.04.016.
-
24.
Borenstein M, Hedges LV. The Handbook of Research Synthesis and Meta-Analysis. In: Cooper H, Hedges LVVJ, editors. Effect Sizes for Meta-Analysis. 3rd ed. New York, USA: The Russell Sage Foundation; 2019. p. 207-44. https://doi.org/10.7758/9781610448864.14.
-
25.
Sword RM, Sword RK, Brunskill SR, Zimbardo PG. Time Perspective Therapy: A New Time-Based Metaphor Therapy for PTSD. J Loss Trauma. 2014;19(3):197-201. https://doi.org/10.1080/15325024.2013.763632.
-
26.
Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM, editors. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Annual Convention of the International Society for Traumatic Stress Studies. 1993; San Antonio, USA. International Society for Traumatic Stress Studies; 1993.
-
27.
Hagh-Shenas H, Goodarzi MA, Dehbozorgi G, Farashbandi H. Psychological consequences of the Bam earthquake on professional and nonprofessional helpers. J Trauma Stress. 2005;18(5):477-83. [PubMed ID: 16281245]. https://doi.org/10.1002/jts.20055.
-
28.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893-7. [PubMed ID: 3204199]. https://doi.org/10.1037//0022-006x.56.6.893.
-
29.
Kaviani H, Mousavi AS. Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI). Tehran Uni Med J. 2008;66(2):136-40.
-
30.
Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77-100. https://doi.org/10.1016/0272-7358(88)90050-5.
-
31.
Fata L, Birashk B, ATEF VM, Dabson KS. [Meaning assignment structures/schema, emotional states and cognitive processing of emotional information: comparing two conceptual frameworks]. Iran J Psychiatry Clin Psychol. 2005;11(3 (42)):312-26. Persian.
-
32.
Zimbardo PG, Boyd JN. Putting time in perspective: A valid, reliable individual-differences metric. In: Stolarski M, Fieulaine N, van Beek W, editors. Time Perspective Therapy: Transforming Zimbardo’s Temporal Theory into Clinical Practice. Cham, Bavaria: Springer; 2015. p. 17-55. https://doi.org/10.1007/978-3-319-07368-2_2.
-
33.
Alizadeh-Fard S. Predicting Pain Catastrophizing of Women with Breast Cancer Based on Perceived Injustice and Past Time Perspective. Int J Cancer Manag. 2020;13(4). e98949. https://doi.org/10.5812/ijcm.98949.
-
34.
Oyanadel C, Buela-Casal G. Time perception and psychopathology: Influence of time perspective on quality of life of severe mental illness. Actas Esp Psiquiatr. 2014;42(3):99-107. [PubMed ID: 24844809].
-
35.
Kaya Lefevre H, Mirabel-Sarron C, Docteur A, Leclerc V, Laszcz A, Gorwood P, et al. Time perspective differences between depressed patients and non-depressed participants, and their relationships with depressive and anxiety symptoms. J Affect Disord. 2019;246:320-6. [PubMed ID: 30594874]. https://doi.org/10.1016/j.jad.2018.12.053.
-
36.
Bandura A, Blahard EB, Ritter B. Relative efficacy of desensitization and modeling approaches for inducing behavioral, affective, and attitudinal changes. J Pers Soc Psychol. 1969;13(3):173-99. [PubMed ID: 5389394]. https://doi.org/10.1037/h0028276.
-
37.
Bellini S, Akullian J. A Meta-Analysis of Video Modeling and Video Self-Modeling Interventions for Children and Adolescents with Autism Spectrum Disorders. Except Child. 2016;73(3):264-87. https://doi.org/10.1177/001440290707300301.
-
38.
Andersen BL, Kiecolt-Glaser JK, Glaser R. A biobehavioral model of cancer stress and disease course. Am Psychol. 1994;49(5):389-404. [PubMed ID: 8024167]. [PubMed Central ID: PMC2719972]. https://doi.org/10.1037//0003-066x.49.5.389.