Abstract
Background:
Medical compliance plays an essential role in the control of cancer and psychological factors such as metacognitive beliefs, positive psychology, and coping styles which are among the predictors of medical compliance.Objectives:
The aim of this study was to determine how much metacognitive beliefs, positive states of mind, and emotional approach coping can predict medical compliance in patients with breast cancer.Methods:
This was a descriptive correlational study. By available sampling method, 154 women with breast cancer who were medically treated and had inclusion criteria, responded to the Morisky Medication Adherence scale (MMAS), Metacognitive Beliefs questionnaire (MCBQ), Positive states of mind (PSOM) scale, and emotional approach coping (EAC) scale. Stepwise multiple regression analysis by SPSS statistics version 24 was applied for data analysis.Results:
There was a significant correlation between positive states of mind and metacognitive beliefs and between emotional approach coping with medical compliance (P < 0.05). Positive states of mind and metacognitive beliefs were the best predictors of medical compliance (P < 0.001), while the emotional approach coping could not predict medical compliance. Results also showed that positive states of mind (β = 0. 51) have the greatest predictive power to medical compliance, and the variable of emotional approach coping is not effective in predicting.Conclusions:
Research findings suggest that positive states of mind and orientation toward metacognitive beliefs can control anxiety among patients and predict medical compliance in patients with breast cancer but research about emotional approach coping needs to more investigation.Keywords
Metacognitive Awareness Emotional Stress Compliance Breast Cancer
1. Background
Cancer is an umbrella term for a large group of diseases that are characterized by abnormal growth beyond the normal range of cells and may affect the adjacent parts of the body (1). The basis of the progression of this disease is a mass of molecular changes in the genome of somatic cells (2). Breast cancer is highly prevalent in women and is the second leading cause of mortality in Iran (3). Medical compliance shows the degree of acceptance of the disease, understanding medical advice, and following medical instructions. Despite effective therapies to reduce the disease, medical compliance by patients with cancer including adopting a healthy lifestyle and regular medication use is one of the most important challenges for clinicians (4). In a cross-sectional study, the rate of non-adherence to cancer treatment was reported to be 50% and estimated to range between 16% and 100% in patients with breast cancer and hematologic malignancies (5). The concept of compliance is not only about patients taking or not taking medications, but also about how the patients manage their treatment and how they take care of themselves (6). In the field of psycho-oncology, one of the problems of care systems in patients with cancer is the lack of compliance with treatment and medical advice (7). Failure to follow the medication regimen will slow down the healing process and reduce the quality of life, and sometimes even lead to re-hospitalization. Some psychological factors such as personality characteristics and adaptability are the predictors of medical compliance in patients receiving oral medications (8-10). One of the psychological constructs associated with medical compliance in patients with cancer is metacognition beliefs. Metacognitive belief means how people organize their thoughts and can control their thoughts verbally and non-verbally. People with negative metacognitive beliefs lead to inability to control and dangerous cognitive thoughts and experiences such as “If I cough, then breast cancer will metastasize to me” or “If I forget to name things, it means I have brain cancer”. Therefore, modification of metacognitive function can increase medical compliance (11, 12). So far no research has been done on the relationship between metacognitive beliefs and medical compliance but the Self-Regulatory Executive Functioning model (S-REF) taken from meta-cognitive models describes that negative thoughts about cancer may activate negative metacognitive beliefs and concerns and do not directly cause distress (13). Therefore, patients are the first concerned and think of positive and negative aspects of the disease. Next, they evaluate their concerns and turn to metacognitive strategies to address emotional concerns (14). Research findings on the relationship between metacognitive beliefs, anxiety, and depression in patients with cancer and cardiovascular diseases showed that beliefs such as uncontrollability and risk, regardless of the type of physical illness, increase patients’ anxiety (15). A study using metacognitive interventions in 114 patients with breast cancer reduced the fear of relapse, and the results showed that increased metacognitive and interpersonal skills can promote medical compliance (16).
Positive states of mind are one of the psychological factors associated with medical compliance. Positive states of mind include focused attention, productivity, responsible care, mental relaxation, and sensory enjoyment (17, 18). There is a relationship between positive and negative thinking and mental health. The positive states of mind are a fraction of positive thoughts/(negative thoughts + positive thoughts). It is a type of cognitive balance that represents psychological self-regulation or cognitive homeostasis. Thus, the balance between positive and negative thoughts predicts mental health (19). In patients with cancer who are challenged with the physical and mental aspects of the disease, it is difficult to establish a positive balance, but by changing the way patients think, a positive cognitive balance can be achieved. Training positive thinking in patients with cancer will increase their quality of life and their level of resistance to the disease. In addition, focusing on positive thinking in patients with cancer reduces depression and increases the perception of their superior abilities (20). The researchers found that patients with high positive mental states experience less depression and perceive stress. Thus, a positive state of mind shows a mediating effect against the negative effects of stress in patients with cancer. Most research has been focused on the effects of positive thinking and improving post-illness mental health problems, so there is a scarcity of studies on medical compliance (21).
Emotional approach coping means trying to reduce negative emotions towards an event by using emotional expression (18). Where the patient is trying to deny and avoid the disease, expressing emotions seems a beneficial method. Deliberate confrontation with the stressor through processing and expressing emotions leads to receiving social support or revisiting the implications of the stressor. In the process of emotional expression, the patient is able to express his / her feelings and engage in emotional self-reflection instead of self-blame (22). A study on male patients with prostate cancer has revealed that emotional approach coping has reduced their pain, inflammation, and problems associated with the disease (23). A study aimed at changing emotional processing with supportive counseling intervention in 201 recently-diagnosed women with cancer showed that expressing emotions and emotional recognition can be effective in controlling the disease and medical compliance (24). Previous studies confirmed that medical compliance is related to patients’ psychological status and is necessary to examine metacognitive beliefs, positive states of mind, and emotional approach coping as predictors of medical compliance in patients with breast cancer. Previous research on these variables is scarce.
2. Objectives
The present study aimed at investigating metacognitive beliefs, positive states of mind, and emotional approach coping as predictors of medical compliance in patients with breast cancer.
3. Methods
3.1. Design and Study Subjects
This descriptive and correlational study was performed among women with breast cancer referred to Golestan Hospital Clinical Oncology Center, Ahvaz, Iran. During March to May 2019, 154 women were enrolled based on the inclusion criteria included (1) the diagnosis of breast cancer; (2) receiving medical treatment; (3) at least 6 months elapsed since diagnosis; (4) duration of illness less than five years; (5) lack of psychiatric illnesses; and (6) willingness to participate in the study. The Ethic committee of Shahid Chamran University of Ahvaz approved this study (by ethics code: EE/97.24.3.93332/scu.ac). Before conducting the research, the informed consent forms were completed by the patients. All participants were aware of research goals and the right to withdraw from the research at any time; they were also assured of non-disclosure of their identity. Their questions were answered in whole of the research process. Finally, they received some recommendations about metacognition beliefs and feel free to speak about breast cancer with a psychologist researcher. Multi regression analysis by SPSS statistics version 24 was applied for data analysis.
3.2. Instrument
3.2.1. The Medication Adherence Scale
The Medication Adherence scale (MMAS) is a self- report measurement developed by Morisky el al. (24). The MMAS was design to assess medical compliance and consists of eight statements which was categorized as poor, moderate, and high compliance with score of < 6, 6 to 8, and > 8, respectively. Higher scores indicate greater medical compliance. Patients completed the scale by yes (1) or no (0). In initial report of Morisky et al. (25), the Cronbach's alpha coefficient was reported 0.61 and the validity coefficient via the correlation between blood pressure of chronic patients and medical compliance was r = 0.72. In the current research, the reliability of scale among the sample of patients was 0.71.
3.2.2. The Metacognitive Beliefs Questionnaire (MCBQ)
The MCBQ-30 is a self-report measurement developed by Wells et al. (26). The MCBQ-30 measures individual differences in a selection of metacognitive beliefs, judgments, and monitoring tendencies. The MCBQ-30 consists of 30 items assessing maladaptive metacognitive beliefs. Items are scored on a 4-point scale from 1 (do not agree) to 4 (strongly agree). Higher scores indicating greater conviction in metacognitive beliefs. The MCBQ-30 has acceptable to excellent internal consistency (αs = 0.91). In the current study, the reliability of the scale in a sample of patients was 0.89.
3.2.3. The Positive States of Mind Scale
The positive states of mind (PSOM) is a self- report measurement developed by Horowitz et al. (19) and includes six items measuring positive emotional and cognitive experiences. It assesses experiences of focused attention, productivity, responsible caretaking, restful repose, sharing, and sensuous non-sexual pleasure. Responses are indicated on 5-point Likert-type scales from 1(not at all) to 5 (very much). Horowitz et al. reported high reliability (αs = 0.86). In the current study, the reliability of the scale in a sample of patients was 0.87.
3.2.4. Emotional Approach Coping Scale
The emotional approach coping (EAC) scale is a self- report measurement developed by Stanton et al. (27). It consists of eight questions and measures emotional processing (i.e. active attempts to knowledge and understanding emotion) and emotion expression. Responses are indicated on 4-point Likert- type scales from1 (I usually do not do this at all) to 4 (I usually do this a lot). In initial report of Stanton et al. reliability was reported 0.73. In the current study, the reliability of the scale in a sample of patients was 0.83.
4. Results
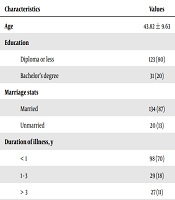
Demographic characteristics of the study participants included age (between 18 and 65 years with the mean age of 43.82 ± 9.63), education (80% diploma and under diploma minister and 20% undergraduate), disease duration (disease duration in 70% was less than one year, in 18% between one to three years and in 11% more than three years), marital status (13% single and 87% married) and treatment (83% chemotherapy and hormonotherapy and 17% hormonotherapy) (Table 1).
| Characteristics | Values |
|---|---|
| Age | 43.82 ± 9.63 |
| Education | |
| Diploma or less | 123 (80) |
| Bachelor’s degree | 31 (20) |
| Marriage stats | |
| Married | 134 (87) |
| Unmarried | 20 (13) |
| Duration of illness, y | |
| < 1 | 98 (70) |
| 1 - 3 | 29 (18) |
| > 3 | 27 (11) |
| Treatment | |
| Chemotherapy and hormone therapy | 121 (83) |
| Hormonotherapy | 27 (17) |
| Mastectomy | 0 (0) |
Table 2 shows the descriptive findings (i.e., mean, standard deviation, and correlation coefficients) of the research variables. There was a significant negative correlation between metacognitive beliefs and adherence to treatment and between positive states of mind and emotional approach coping (P < 0.05).
Descriptive Statistics and Inter-Correlations Matrix
Table 3 shows the stepwise regression analysis. Variables of positive states of mind and metacognitive beliefs were predictors of medical compliance, and both variables predicted 40% of the variance in compliance. Positive states of mind (β = 0.51) had the highest predictive power of medication compliance and the emotional approach coping variable based on emotional confrontation was not effective in predicting medication compliance.
Results of Multiple Regression Analysis in Predicting Medication Compliance
| R2 | F | Sig | B | β | T | Sig | |
|---|---|---|---|---|---|---|---|
| Positive states of mind | 0.26 | 53.62 | < 0.001 | 0.39 | 0.51 | 7.32 | < 0.001 |
| Positive states of mind and metacognitive believes | 0.40 | 50.48 | < 0.001 | -0.06 | -0.38 | -5.93 | < 0.001 |
5. Discussion
The results showed that positive states of mind and orientation toward metacognitive beliefs could control anxiety among patients and predict breast cancer patients’ medical compliance. The medical compliance was not predicted by emotional approach coping. Despite effective therapies to reduce breast cancer, medical compliance by patients with cancer including adopting a healthy lifestyle, regular attendance at therapeutic sessions, and regular use of prescription drugs are some of the most important challenges for clinicians (4). Previous research has documented high rates of noncompliance to prescribed medical therapy in patients with cancer. Psychological barriers to medical compliance can be divided into intentional and unintentional. Intentional non-medical compliance means lack of follow-up for treatment refers to cases in which patients decide to discontinue treatment (e.g., long-term withdrawal of cancer control medications) or change the recommended treatment. unintentional non- medical compliance means lack of follow-up for treatment refers to cases in which patients mistakenly think they are following the desired treatment (for example, taking an iron, while eating and do not need to take more iron tablets) (7). Different psychological factors are effective in medical compliance in patients with cancer (8, 9). One of the psychological models of the Self-Regulatory Executive Functioning model (S-REF) is taken from metacognitive models describing that negative thoughts activate worry about cancer in patients with cancer through the development of cognitive-attentional syndrome (CAS) (10, 11). CAS consistent thinking styles such as anxiety or helplessness, extreme attention to threats, denial, and avoidance of disease acceptance. So, they lead patients to negative metacognitive beliefs about uncontrollable disease and automatic reduction medical compliance. The present research showed that Metacognitive beliefs have high correlation with medical compliance and this finding is in line with the Butow et al. study (14) that suggested attentional bias and negative metacognition could lead patients with cancer to non-medical compliance. The results of another research conducted by Cheli et al. (13) is congruent with our research and showed that using meta-cognitive interventions in 114 patients with breast cancer reduced the fear of relapse, increasing metacognitive, it also showed that interpersonal skills could improve the quality of life of patients and increased their medical compliance. In the current research, positive states of mind (β = 0.51) had the highest predictive power of medical compliance because positive thinking leads the patient to seek support and effective treatments. This finding is in line with the study of Mousavi et al. (18). So, Balance between negative and positive thoughts improves patients’ mental state. Therefore, positive thinking training in patients with cancer increase their quality of life and their level of resistance to the disease. In addition, not only thoughts but also emotional approach coping is a valuable way to medical compliance in patients with cancer. Marroquin, et al. (28) explained that emotional approach coping is a form of emotional regulation in which can be relieved the processing of negative emotional experiences such as speak with family and friends about illness and kind of painful treatment or even crying for why it is happens to them. When a patient tries to deny the disease and avoid treatment, a useful method is emotional guidance and expression of emotions. Hoyt et al. (23) and Weihs et al. (29) have studied on men with prostate cancer and women with breast cancer and their findings showed that intimacy and emotional expression can help the patient to protect against negative emotions and concerns about the disease. Emotional approach coping in this study did not predict medical compliance and it was inconsistent with previous results. Research finding of Andrykowski et al. (22) showed that emotional expression during the treatment in patients with cancer need social support from their family and friends and without psychological support this coping be just a disturbing thought about treatment and cancer. In this research, patients were in stage 2 or 3 of breast cancer and may need to take more time to emotional expression. This psychological construct needs further investigation.
5.1. Conclusions
Overall, the present study showed a significant positive correlation between positive states of mind and emotional approach coping and negatively with metacognition beliefs. Also, the results of current study showed that positive states of mind and metacognition beliefs can predict medical compliance but emotional approach coping in the patients with cancer was not predictable.
5.2. Limitations
The present study had some limitations. First, a self-report test was used to collect the data, which had a limit to the Likert response. Second, participants were female with breast cancer, therefore the results cannot be generalized to other kinds of cancers. These limitations suggest that the correlation coefficient only shows the relationship between the variables, and to find the causal relationship, one must use the path analysis method with the mediation of social support. It is suggested that an open interview method can be used to collect data so that patients have more opportunities to express their emotions. Finally, for more result generation, more similar studies to other type of cancer or mastectomy patients are required.
Acknowledgements
References
-
1.
World Health Organization. International agency for research on cancer (IARC). Geneva, Switzerland: WHO; 2018.
-
2.
DeVita VT, Lawrence TS. Rosenberg’s cancer: Principles and practice of oncology. Philadelfia: Wolters Kluwer; 2008.
-
3.
Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. Breast J. 2007;13(4):383-91. [PubMed ID: 17593043]. https://doi.org/10.1111/j.1524-4741.2007.00446.x.
-
4.
Anthony SL. The influence of depression on medication adherence among cancer survivors. Carolina: East Carolina University; 2019.
-
5.
Lang-Rollin I, Berberich G. Psycho-oncology. Dialogues Clin Neurosci. 2018;20(1):13-22. [PubMed ID: 29946207]. [PubMed Central ID: PMC6016045].
-
6.
Bouwman L, Eeltink CM, Visser O, Janssen J, Maaskant JM. Prevalence and associated factors of medication non-adherence in hematological-oncological patients in their home situation. BMC Cancer. 2017;17(1):739. [PubMed ID: 29121889]. [PubMed Central ID: PMC5679497]. https://doi.org/10.1186/s12885-017-3735-1.
-
7.
Lima MP, Machado WL, Irigaray TQ. Predictive factors of treatment adherence in cancer outpatients. Psychooncology. 2018;27(12):2823-8. [PubMed ID: 30239056]. https://doi.org/10.1002/pon.4897.
-
8.
Hall AE, Paul C, Bryant J, Lynagh MC, Rowlings P, Enjeti A, et al. To adhere or not to adhere: Rates and reasons of medication adherence in hematological cancer patients. Crit Rev Oncol Hematol. 2016;97:247-62. [PubMed ID: 26412718]. https://doi.org/10.1016/j.critrevonc.2015.08.025.
-
9.
Dawson LA. What factors affect adherence to medicines? Arch Dis Child Educ Pract Ed. 2019;104(1):49-52. [PubMed ID: 29374624]. https://doi.org/10.1136/archdischild-2017-312820.
-
10.
Mutlu HH, Bilican FI, Mutlu HH, Gumus M. A comparison of metacognitive factors among patients with cancer and the control group. Psychooncology. 2018;27(4):1277-83. [PubMed ID: 29466609]. https://doi.org/10.1002/pon.4667.
-
11.
Hargis MB, Castel AD. Improving medication understanding and adherence using principles of memory and metacognition: In press - policy insights from behavioral and brain sciences. Policy Insights Behav Brain Sci. 2018;5(2):147-54. [PubMed ID: 31552287]. [PubMed Central ID: PMC6758907]. https://doi.org/10.1177/2372732218781643.
-
12.
Cook SA, Salmon P, Dunn G, Holcombe C, Cornford P, Fisher P. The association of metacognitive beliefs with emotional distress after diagnosis of cancer. Health Psychol. 2015;34(3):207-15. [PubMed ID: 25133826]. [PubMed Central ID: PMC4321533]. https://doi.org/10.1037/hea0000096.
-
13.
Cheli S, Caligiani L, Martella F, De Bartolo P, Mancini F, Fioretto L. Mindfulness and metacognition in facing with fear of recurrence: A proof-of-concept study with breast-cancer women. Psychooncology. 2019;28(3):600-6. [PubMed ID: 30656783]. https://doi.org/10.1002/pon.4984.
-
14.
Butow P, Kelly S, Thewes B, Hruby G, Sharpe L, Beith J. Attentional bias and metacognitions in cancer survivors with high fear of cancer recurrence. Psychooncology. 2015;24(4):416-23. [PubMed ID: 25156065]. https://doi.org/10.1002/pon.3659.
-
15.
Anderson R, Capobianco L, Fisher P, Reeves D, Heal C, Faija CL, et al. Testing relationships between metacognitive beliefs, anxiety and depression in cardiac and cancer patients: Are they transdiagnostic? J Psychosom Res. 2019;124:109738. [PubMed ID: 31443817]. https://doi.org/10.1016/j.jpsychores.2019.109738.
-
16.
Branstrom R, Kvillemo P, Moskowitz JT. A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. Int J Behav Med. 2012;19(4):535-42. [PubMed ID: 21931958]. [PubMed Central ID: PMC3518555]. https://doi.org/10.1007/s12529-011-9192-3.
-
17.
Schwartz RM, Caramoni GL. Cognitive balance and psychopathology: Evaluation of an information processing model of positive and negative states of mind. Clin Psychol Rev. 1989;9(3):271-94. https://doi.org/10.1016/0272-7358(89)90058-5.
-
18.
Mousavi E, Esmaeili A, Shahid Saless S. The effect of positive thinking on quality of life and resiliency of cancer patients. Razavi Int J Med. 2015;3(3). https://doi.org/10.17795/rijm27122.
-
19.
Horowitz M, Adler N, Kegeles S. A scale for measuring the occurrence of positive states of mind: A preliminary report. Psychosom Med. 1988;50(5):477-83. [PubMed ID: 3186891]. https://doi.org/10.1097/00006842-198809000-00004.
-
20.
Khodabakhsh R, Khosravi Z, Shahangian S. The effect of positive psychotherapy on depression and personal abilities in cancer patients. Positive Psychol Bull. 2014;1(1):35-49.
-
21.
Huffman JC, DuBois CM, Mastromauro CA, Moore SV, Suarez L, Park ER. Positive psychological states and health behaviors in acute coronary syndrome patients: A qualitative study. J Health Psychol. 2016;21(6):1026-36. [PubMed ID: 25114026]. [PubMed Central ID: PMC4490125]. https://doi.org/10.1177/1359105314544135.
-
22.
Andrykowski MA, Pavlik EJ. Response to an abnormal ovarian cancer-screening test result: Test of the social cognitive processing and cognitive social health information processing models. Psychol Health. 2011;26(4):383-97. [PubMed ID: 20419561]. [PubMed Central ID: PMC2911487]. https://doi.org/10.1080/08870440903437034.
-
23.
Hoyt MA, Stanton AL, Irwin MR, Thomas KS. Cancer-related masculine threat, emotional approach coping, and physical functioning following treatment for prostate cancer. Health Psychol. 2013;32(1):66-74. [PubMed ID: 23316854]. https://doi.org/10.1037/a0030020.
-
24.
Manne SL, Myers-Virtue S, Darabos K, Ozga M, Heckman C, Kissane D, et al. Emotional processing during psychotherapy among women newly diagnosed with a gynecological cancer. Palliat Support Care. 2017;15(4):405-16. [PubMed ID: 27964770]. https://doi.org/10.1017/S1478951516000845.
-
25.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67-74. [PubMed ID: 3945130]. https://doi.org/10.1097/00005650-198601000-00007.
-
26.
Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behav Res Ther. 2004;42(4):385-96. [PubMed ID: 14998733]. https://doi.org/10.1016/S0005-7967(03)00147-5.
-
27.
Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: Scale construction and validation. J Pers Soc Psychol. 2000;78(6):1150-69. [PubMed ID: 10870915]. https://doi.org/10.1037//0022-3514.78.6.1150.
-
28.
Marroquin B, Czamanski-Cohen J, Weihs KL, Stanton AL. Implicit loneliness, emotion regulation, and depressive symptoms in breast cancer survivors. J Behav Med. 2016;39(5):832-44. [PubMed ID: 27287618]. [PubMed Central ID: PMC5014704]. https://doi.org/10.1007/s10865-016-9751-9.
-
29.
Weihs KL, Enright TM, Simmens SJ. Close relationships and emotional processing predict decreased mortality in women with breast cancer: Preliminary evidence. Psychosom Med. 2008;70(1):117-24. [PubMed ID: 18158376]. https://doi.org/10.1097/PSY.0b013e31815c25cf.