Abstract
Context:
Various frequency rates of occult hepatitis B virus infection (OBI) are reported from different parts of Iran. This systematic review and meta-analysis aimed to characterize the OBI epidemiology in Iran and estimate the pooled prevalence among different populations.Evidence Acquisition:
Nine international and Persian electronic databases, as well as some conference proceedings, were searched. Original cross-sectional studies up to December 2018 were included if they investigated the prevalence of OBI by the detection of serum hepatitis B virus surface antigen and hepatitis B virus nucleic acid in at least 30 samples selected with any sampling methods. Comprehensive meta-analysis software was used to analyze the data, and Cochran’s Q-test and I-square statistics were applied to assess the heterogeneity. Meta-regression analysis was performed to assess the impact of the year of study on the OBI frequency. A P value < 0.05 was considered as the level of significance.Results:
Of 412 citations found in electronic sources and 35 relevant citations added by searching the gray literature, 83 non-duplicated non-overlapping studies were evaluated. A total of 55 documents comprising 14,485 individuals from 16 provinces met the inclusion criteria and were used in the analysis. The prevalence of OBI considerably varied in different parts of the country with the highest prevalence (63.1%) reported among the HIV-positive population in Fars province. The rates of the OBI prevalence were estimated at 0.06% (95% CI: 0.02 - 0.16%) among blood donors (BDs) regardless of their anti-HBc status, 7.90% (95% CI: 4.33 - 13.99%) among anti-HBc positive BDs, 2.49% (95% CI: 1.2 - 4.81%) among hemodialysis (HD) patients, 4.44% (95% CI: 1.56 - 12.02%) among HIV-positive patients, and 7.76% (95% CI: 4.57 - 12.86%) among HCV-positive patients. No significant trends were observed in OBI prevalence rates among different groups over time (P > 0.05).Conclusions:
This review revealed high rates of OBI prevalence among high-risk populations in Iran. It is strongly suggested that occult hepatitis B be investigated among populations with a high chance of its occurrence in our country.Keywords
Occult Hepatitis B Virus Infection Prevalence Review Meta-Analysis Iran
1. Context
Occult hepatitis B virus (HBV) infection is characterized by the detection of a low level of HBV DNA in the liver or serum of people who are seronegative for HBV surface antigen (HBsAg) in a period other than the window period of acute infection (1, 2). Occult HBV infection (OBI) has been proposed to occur in several clinical contexts such as the recovery of the past infection characterized by the presence of antibodies to HBsAg (anti-HBs); chronic HBV carriage with very low, undetectable HBsAg levels and the presence of anti-hepatitis B core antigen (anti-HBc) as the only serum marker (isolated anti-HBc) or without any serum marker of HBV (seronegative); and chronic hepatitis B with surface gene escape mutations (3).
Some significant clinical concerns have been suggested for OBI, including (1) The probability of HBV transmission through blood transfusion or organ transplantation (4, 5); (2) chronic liver disease progression toward cirrhosis due to persistent inflammatory necrosis (6); (3) hepatocellular carcinoma (HCC) development due to the direct oncogenicity effect of HBV and/or the formation of necrotic inflammation following persistent replication of the virus (7); and (4) The possibility of HBV reactivation in immunosuppression conditions such as receiving chemotherapy or other immunotherapy (8).
The prevalence rate of OBI has ranged from zero to 63% among different populations studied in various provinces of Iran. This diversity has been observed among different groups in one region, as well as among a specific group from different areas of the country. For instance, the OBI prevalence in Tehran province in the north of Iran varied from zero among blood donors (BDs) (9) and multi-transfused patients (MTPs) (10) to 18% in HIV-positive individuals (11), 20% in HCV-positive patients (12), and 22% among people who inject drugs (PWID) (13). On the other hand, some studies found no OBI cases among Iranian BDs in provinces such as Tehran (9), Razavi Khorasan (14), Khuzestan (15), Kermanshah (15, 16), and Yazd (17) and some surveys reported the high rates among BDs in Isfahan (11.6%) (18), Fars (15.8%) (19), and Kerman (16.2 %) provinces (20).
This systematic review and meta-analysis study was performed to characterize the OBI epidemiology in Iran and estimate the pooled prevalence among different low- and high-risk Iranian populations such as BDs, hemodialysis (HD) patients, and HIV- and HCV-positive patients. The results of our review would help health authorities to make appropriate decisions for control of OBI in Iran, especially among high-risk groups.
2. Methods
2.1. Data Sources and Search Strategies
This systematic review and meta-analysis study was conducted following the PRISMA 2009 statement. The main purpose of the investigation was the presence of HBV DNA identified by polymerase chain reaction (PCR) in the blood samples of different population groups in Iran. Indexing phrases included “Iran” and all terms that referred to occult HBV infection everywhere in the text (OBI OR “Occult Hepatitis B” OR “Occult HBV” OR “HBsAg negative” OR “HBs Antigen negative”). Language equivalents of these words were used to search the documents published in Persian sources. Some international electronic resources such as ISI, PubMed, Scopus, ScienceDirect, and Proquest, as well as four Iranian databases including Scientific Information Database (SID), Barakat Knowledge Network System (previously named as IranMedex), Iranian Database of Publication (Magiran), and the Regional Information Centre for Science and Technology (RICeST), were searched until the end of 2018. Furthermore, all references identified from bibliographies of relevant review articles were manually searched. Iranian databases were explored for gray literature such as research projects, dissertations, theses, and abstracts. Besides, some available pertinent abstract booklets and conference proceedings were manually reviewed.
2.2. Study Selection and Data Extraction
After reviewing the titles and abstracts, all records that reported the prevalence of OBI among healthy individuals or different patient groups of Iran were chosen to review their full texts. Variables such as the first author, year of publication, year of study, study location, study population, sampling method, the number of cases with HBsAg and HBV DNA seropositivity, anti-HBc test results, and diagnostic methods used to assess the serum HBV genome were extracted from each study. The main inclusion criteria were the assessment of the HBV genome among at least 30 HBsAg seronegative samples selected through random or non-random sampling methods in a cross-sectional survey. Laboratory methods included Enzyme-Linked Immunosorbent Assay (ELISA) or chemiluminescence immunoassay to screen serum HBsAg and PCR techniques to detect serum HBV DNA. Surveys that evaluated HBV DNA in peripheral blood mononuclear cells or liver tissue samples were excluded. Besides, case reports, review articles, editorials, or letters with no report of OBI prevalence in a specific population were not included. The quality of studies was independently evaluated by two investigators, and eligible studies were selected based on their agreement.
2.3. Data Analysis
Data were analyzed using comprehensive meta-analysis software Ver. 3.3.070 (Biostat, Englewood, NJ, USA). Binomial distribution was used to calculate the prevalence in each study. The number of cases with detectable HBV DNA and the total number of studied samples were entered to calculate the event rate and its 95% confidence interval (CI). If a study referred to the event rate but did not provide the number of positive cases, it was recalculated through multiplying the total number of samples by the reported rate of OBI frequency in percentage. A weight was assigned to each study as the inverse variance. Using the Der-Simonian and Laird method, a random-effect model was applied when heterogeneity between studies was identified based on Cochran’s Q-test (P < 0.05) and I-square (I2) statistics (values of > 50%). The point prevalence rates and their 95% CIs for different populations were illustrated by forest plots.
Subgroup analyses were performed to explore the possible factors associated with heterogeneity. A meta-analysis was also implemented after removing surveys with most influences on the heterogeneity due to the reporting of a very high prevalence rate among a specific population. Moreover, additional analysis was done after excluding studies assessing the OBI rate among only cases with anti-HBc seropositivity. Furthermore, a meta-regression analysis was used to investigate significant changes in the prevalence rates over time. All statistical data were considered significant if a P value was less than 0.05.
3. Results
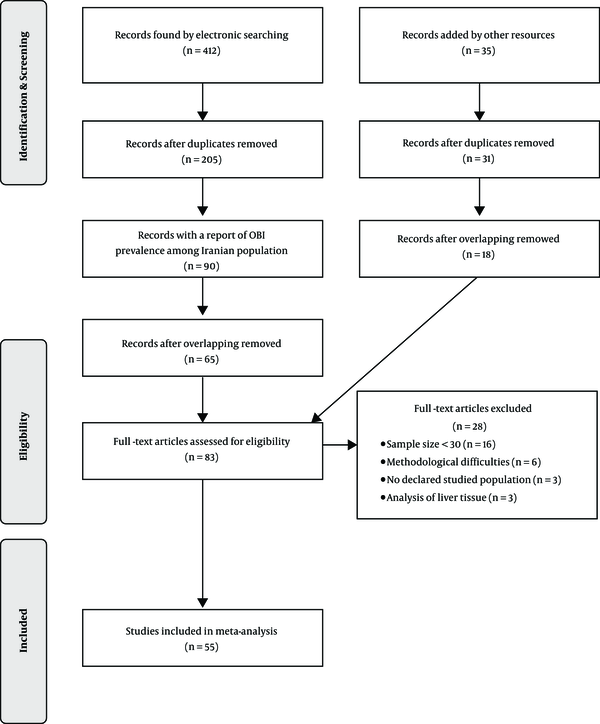
In the initial search of 254 citations retrieved from international electronic sources and 158 citations found in Iranian databases, 205 non-duplicated documents were selected, of which 90 surveys determined the prevalence of OBI in the Iranian population (Figure 1). The search for gray literature added 31 non-duplicate pertinent citations. After removing 38 overlapping surveys (the same studied population, sample sizes, methods, and findings), 83 non-duplicated and non-overlapping surveys were evaluated. A total of 55 non-duplicate and non-overlapping documents met the inclusion criteria and were used in the analysis (Table 1) (9-63). They reported OBI prevalence among 14,485 individuals (min: 31, max: 5000) from 16 provinces of Iran during 2004 - 2018 (Table 1). The studied population included healthy populations such as BDs, tissue donors, and healthcare personnel, as well as high-risk groups including thalassemia, hemophilia, and HD patients, HCV and/or HIV-positive individuals, PWID, patients with unknown liver disease, and family members of HBsAg-positive cases. All studies applied a PCR technique to detect OBI, comprising conventional PCR (20 studies), nested PCR (15 studies), and real-time PCR (20 studies).
Document search and selection for systematic review and meta-analysis of occult hepatitis B prevalence in Iran
Selected Studies for Systematic Review and Meta-Analysis of Occult Hepatitis B Prevalence in Irana
| Study | Date (Years) | Province | Population | Sample Size | HBV Serology | HBV DNA Detection Method | OBI | |
|---|---|---|---|---|---|---|---|---|
| Conduction | Publication | |||||||
| Ghaziasadi et al. (21) | Un | 2017 | Markazi | GP (Children) | 558 | HBsAg- | Real-time PCR | 54 (9.68) |
| Azarkar et al. (22) | 2016 - 2018 | 2019 | South Khorasan | GP | 596 | Isolated anti-HBc+ | Nested PCR | 61 (10.23) |
| Karimi et al. (15) | 2013 | 2016 | Kermanshah/Khuzestan | BDs | 2031 | HBsAg- | Real time PCR | 0 (0) |
| Abbasi et al. (16) | 2013 | 2016 | Khuzestan | BDs | 184 | HBsAg- | Nested PCR | 0 (0) |
| Ahmadi Ghezeldasht et al. (14) | 2018 | 2018 | Razavi Khorasan | BDs | 545 | HBsAg- | Real-time PCR | 0 (0) |
| Shahabi et al. (23) | Un | 2009 | Razavi Khorasan | BDs | 60 | HBsAg-anti-HBc+ | Nested PCR | 0 (0) |
| Amini Kafi-abad et al. (9) | Un | 2007 | Tehran | BDs | 230 | HBsAg-anti-HBc+ | Conventional PCR | 0 (0) |
| Vaziri and Javadzadeh Shahshahani (17) | 2015 | 2017 | Yazd | BDs | 74 | HBsAg-anti-HBc+ | Conventional PCR | 0 (0) |
| Alizadeh and Milani (24) | 2008 - 2009 | 2014 | Tehran | BDs | 5000 | HBsAg- | Real-time PCR | 2 (0.04) |
| Khamesipour et al. (25) | Un | 2011 | Guilan | BDs | 78 | HBsAg-anti-HBc+ | Real-time PCR | 1 (1.28) |
| Pourazar et al. (18) | Un | 2005 | Isfahan | BDs | 43 | HBsAg-anti-HBc+ | Conventional PCR | 5 (11.63) |
| Behzad-Behbahani et al. (26) | 2001 - 2002 | 2006 | Fars | BDs | 131 | HBsAg-anti-HBc+ | Conventional PCR | 16 (12.21) |
| Behzad-Behbahani et al. (19) | Un | 2011 | Fars | BDs | 76 | HBsAg-anti-HBc+ | Real-time PCR | 12 (15.79) |
| Kazemi Arababadi et al. (20) | 2008 | 2009 | Kerman | BDs | 352 | HBsAg-anti-HBc+ | Conventional PCR | 57 (16.19) |
| Vaezjalali et al. (27) | 2011 | 2013 | Tehran | BDs | 80 | HBsAg-anti-HBc+ | Nested PCR | 40 (50.00) |
| Samiee et al. (28) | 2014 - 2016 | 2018 | Tehran | Cornea donors | 90 | HBsAg-anti-HBc+ | Real-time PCR | 11 (12.22) |
| Ahmad Akhoundi et al. (29) | 2011 | 2015 | Tehran | HCWs (Dental) | 52 | HBsAg-anti-HBc+ | Real-time PCR | 1 (1.92) |
| Borzooy et al. (30) | Un | 2015 | Tehran | Healthy HCWs | 120 | HBsAg- | Real-time PCR | 4 (3.33) |
| Abbasi et al. (31) | Un | 2012 | Golestan | HD patients | 100 | HBsAg- | Conventional PCR | 0 (0) |
| Joukar et al. (32) | 2009 | 2012 | Guilan | HD patients (59 HCV + cases) | 507 | HBsAg- | Conventional PCR | 0 (0) |
| Kazemi Arababadi et al. (33) | Un | 2009 | Kerman | HD patients (30 HCV + cases) | 90 | HBsAg- | Conventional PCR | 0 (0) |
| Attarpour Yazdi (35) | Un | 2016 | Tehran | HD patients (19 HCV + cases) | 45 | HBsAg- | Conventional PCR | 0 (0) |
| Attarpour Yazdi (34) | Un | 2017 | Yazd | HD HCV + patients | 34 | HBsAg- | Conventional PCR | 0 (0) |
| Ranjbar et al. (63) | 2011 | 2017 | Tehran | HD patients | 200 | HBsAg- | Real time PCR | 1 (0.50) |
| Ramezani et al. (36) | 2013 - 2014 | 2015 | Tehran | HD patients | 100 | HBsAg- | Real time PCR | 1 (1.00) |
| Rastegarvand et al. (37) | 2012 | 2015 | Khuzestan | HD patients | 203 | HBsAg- | Nested PCR | 6 (2.96) |
| Haghazali et al. (38) | 2007 | 2011 | Qazvin | HD patients (10 HCV+ cases) | 129 | HBsAg- | Conventional PCR | 5 (3.88) |
| Keyvani et al. (39) | 2007 | 2013 | 14 provinces | HD patients | 103 | Isolated anti-HBc+ | Conventional PCR | 5 (4.85) |
| Ziyaeyan et al. (40) | Un | 2011 | Fars | HD patients | 55 | HBsAg- | Real time PCR | 4 (7.27) |
| Hashemi et al. (41) | 2011 - 2012 | 2015 | Khuzestan | Relatives of HD patients | 82 | HBsAg- | Nested PCR | 0 (0) |
| HD patients | 82 | HBsAg- | 9 (10.98) | |||||
| Ziaee et al. (42) | Un | 2017 | South Khorasan | Hemophilia | 86 | HBsAg- | Nested PCR | 8 (9.30) |
| Kazemi Arababadi et al. (43) | 2006 - 2007 | 2008 | Kerman | Thalassemia (27 HCV+ cases) | 60 | HBsAg- | Conventional PCR | 0 (0) |
| Makvandi et al. (44) | 2011 - 2012 | 2014 | Khuzestan | Patients with Elevated ALT | 120 | HBsAg- | Nested PCR | 12 (10.00) |
| Kaviani et al. (45) | 1997 - 2001 | 2006 | Fars | Patients with Cryptogenic hepatitis | 104 | HBsAg- | Conventional PCR | 2 (1.92) |
| Hashemi et al. (46) | 2011 - 2012 | 2015 | Khuzestan | Patients with Cryptogenic cirrhosis | 50 | HBsAg- | Nested PCR | 7 (14.00) |
| Sharifi-Mood et al. (47) | 2005 - 2006 | 2009 | Siatan & Baluchestan | Family members of HBsAg + cases | 110 | Isolated anti-HBc+ | Conventional PCR | 3 (2.73) |
| Shahmoradi et al. (48) | Un | 2012 | Mazandaran | Children born to HBsAg + mothers | 75 | HBsAg- | Real-time PCR/Nested PCR | 21 (28.00) |
| Ayatollahi et al. (49) | 2016 | 2019 | Yazd | Patients with cured HBV infection | 96 | HBsAg- | Real-time PCR | 28 (29.17) |
| Shavakhi (50) | 2003 - 2004 | 2004 | Tehran | HCV + patients | 31 | HBsAg- | Conventional PCR | 0 (0) |
| Jonaidi-Jafari et al. (10) | 2009 - 2010 | 2017 | Tehran | HCV + Thalassemia and hemophilia patients | 145 | HBsAg- | Conventional PCR | 0 (4.85) |
| Eshraghi-Mosaabadi et al. (51) | 2013 - 2014 | 2018 | Tehran | HCV + PWID | 94 | HBsAg- | Nested PCR | 7 (7.45) |
| Zandieh et al. (52) | Un | 2005 | Tehran | HCV + patients | 201 | HBsAg- | Nested PCR | 17 (8.46) |
| Shavakhi et al. (53) | 2002 - 2004 | 2009 | Tehran | HCV + patients | 103 | HBsAg- | Nested PCR | 20 (19.42) |
| Vakili Ghartavol et al. (12) | 2010 - 2011 | 2013 | Tehran | HCV + patients | 50 | HBsAg- | Nested PCR | 10 (20.00) |
| Majzoobi et al. (54) | 2013 - 2014 | 2016 | Hamadan | HCV/HIV + patients | 48 | Isolated anti-HBc+ | Conventional PCR | 0 (0) |
| Zhand et al. (55) | Un | 2015 | Golestan | HIV + patients | 120 | HBsAg-anti-HBc+ | Conventional PCR | 0 (0) |
| Aghakhani et al. (56) | 2014 | 2016 | Tehran | HIV + patients (30 HCV + cases) | 92 | HBsAg- | Real-time PCR | 2 (2.17) |
| Tajik et al. (57) | 2015 - 2017 | 2018 | Tehran | HIV + patients | 151 | HBsAg- | Real-time PCR | 4 (2.65) |
| Janbakhsh et al. (58) | Un | 2017 | Kermanshah | HIV + patients (37 HCV + cases) | 66 | HBsAg-anti-HBc+ | Real-time PCR | 8 (12.12) |
| Mohraz et al. (11) | Un | 2016 | Tehran | HIV + patients (99 HCV + cases) | 172 | HBsAg- | Real-time PCR | 31 (18.02) |
| Honarmand et al. (59) | 2012 | 2014 | Fars | HIV + patients | 84 | HBsAg- | Nested PCR | 53 (63.10) |
| Chenari et al. (60) | 2011 - 2013 | 2014 | Razavi Khorasan | HTLV-1 + patients | 109 | HBsAg- | Real-time PCR | 1 (0.92) |
| Asli et al. (13) | 2013 - 2014 | 2016 | Tehran | PWID | 59 | HBsAg-anti-HBc+ | Nested PCR | 13 (22.03) |
| Azizolahi et al. (61) | 2015 | 2017 | Khuzestan | Patients with rheumatologic disorders | 134 | HBsAg- | Real-time PCR | 1 (0.75) |
| Ghorbani Bejandi et al. (62) | Un | 2016 | Tehran | Patients with Behcet's disease | 95 | HBsAg- | - | 7 (7.37) |
The rate of OBI prevalence considerably varied in different parts of the country with the highest prevalence (63.1%) reported among the HIV-positive population in Fars province (Table 1).
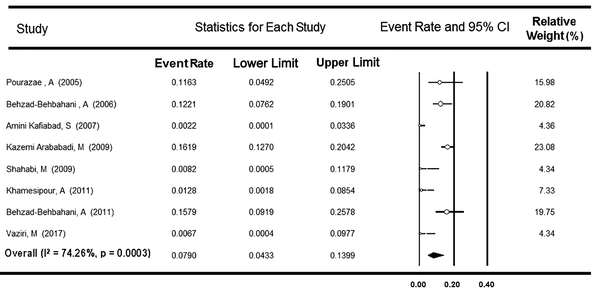
3.1. OBI Prevalence Among Blood Donors
A total of 13 surveys with a report of OBI prevalence among Iranian BDs were used in the meta-analysis. Nine studies investigated the presence of OBI only among HBsAg-negative, and anti-HBc-positive BDs, and four studies explored OBI among HBsAg-negative BDs, regardless of their anti-HBc test results. As Table 2 shows, the first group comprised 1,124 individuals from six provinces. The Cochrane Q-test showed heterogeneity between the studies (P < 0.001, I2 = 90.1%), and the rate of OBI prevalence was estimated at 8.81% (95% CI: 4.11 - 17.91%). After excluding one survey reporting an unexpectedly high rate of OBI (50.0%) (27), the value of I-square decreased to 74.3%, and the OBI rate declined to 7.90% (95% CI: 4.33 - 13.99%, Figure 2). Among the remaining eight surveys, the rate of OBI did not vary by the conventional, real-time, and nested PCR subgroups (P = 0.105, Table 2).
Forest plot of studies on occult hepatitis B infection prevalence among anti-HBc-positive Iranian blood donors
The Pooled Estimates of Occult HBV Infection Prevalence Among Different Iranian Populations, According to the Result of Meta-Analysis
| Population | Prevalence | Sample Size, Total (Min, Max) | Pooled Estimate | Heterogeneity Test | I-Squared, % | ||
|---|---|---|---|---|---|---|---|
| Point, % | 95% CI | Cochran’s Q | P Value | ||||
| Blood donors | With nine surveys included only anti-HBc-positive cases | 1124 (43, 352) | 8.81 | 4.11 - 17.91 | 80.7 | < 0.001 | 90.1 |
| After removing one survey with a report of very high prevalence rate | 1044 (43, 352) | 7.90 | 4.33 - 13.99 | 27.2 | 0.003 | 74.3 | |
| Based on the PCR method used to detect HBV DNA | |||||||
| Conventional (five studies) | 830 (43, 352) | 8.31 | 3.75-17.42 | 16.3 | 0.003 | 75.8 | |
| Real-time (two studies) | 154 (76, 78) | 7.87 | 2.21 - 24.45 | 6.4 | 0.011 | 84.5 | |
| Nested (one study) | 60 (60, 60) | 0.82 | 0.04 - 16.08 | 0 | 1.0 | 0 | |
| Between subgroups | - | - | - | 4.5 | 0.105 | - | |
| With four studies investigating HBsAg-negative BDs regardless of their anti-HBc test results | 7760 (184, 5000) | 0.06 | 0.02 - 0.16 | 1.9 | 0.588 | 0 | |
| Hemodialysis patients | With all 12 related studies | 1648 (34, 507) | 2.49 | 1.28 - 4.81 | 30.8 | 0.001 | 64.2 |
| After excluding one survey with only isolated anti-HBc cases | 1545 (34, 507) | 2.12 | 0.98 - 4.54 | 30.6 | 0.001 | 67.3 | |
| Based on the PCR method used to detect HBV DNA | |||||||
| Conventional (six studies) | 905 (34, 507) | 1.01 | 0.28 - 3.53 | 8.9 | 0.113 | 43.9 | |
| Real-time (three studies) | 355 (55, 200) | 1.98 | 0.44 - 8.43 | 7.7 | 0.021 | 74.0 | |
| Nested (two studies) | 285 (82, 203) | 5.58 | 1.29 - 22.75 | 6.6 | 0.010 | 84.8 | |
| Between subgroups | - | - | - | 7.4 | 0.024 | - | |
| HCV-positive patients | With all 14 related studies | 1029 (30, 201) | 7.76 | 4.57 - 12.86 | 48.2 | < 0.001 | 73.9 |
| After eliminating two surveys with only anti-HBc positive cases | 944 (30, 201) | 7.32 | 4.10 - 12.75 | 43.6 | < 0.001 | 74.8 | |
| Based on the PCR method used to detect HBV DNA | |||||||
| Conventional (six studies) | 367 (30, 145) | 1.51 | 0.54 - 4.16 | 2.2 | 0.824 | 0 | |
| Real-time (two studies) | 129 (30, 99) | 17.01 | 6.96 - 35.95 | 3.9 | 0.048 | 74.4 | |
| Nested PCR (four studies) | 448 (50, 201) | 12.85 | 7.70 - 20.67 | 11.9 | 0.008 | 74.7 | |
| Between subgroups | - | - | - | 25.9 | < 0.001 | - | |
| With six studies with HCV RNA-positive patients | 561 (30, 201) | 8.77 | 4.01 - 18.11 | 21.4 | 0.001 | 76.8 | |
| HIV-positive patients | With all seven related studies | 733 (48, 172) | 6.91 | 1.90 - 22.17 | 116.3 | < 0.001 | 94.8 |
| After removing one survey with a report of very high prevalence rate | 649 (48, 172) | 4.44 | 1.56 - 12.02 | 31.7 | < 0.001 | 84.2 | |
| Based on PCR method used to detect HBV DNA | |||||||
| Conventional (two studies) | 168 (48, 120) | 0.65 | 0.06 - 6.54 | 0.2 | 0.650 | 0 | |
| Real-time (four studies) | 481 (66, 172) | 6.95 | 2.57 - 17.45 | 22.2 | < 0.001 | 86.5 | |
| Between subgroups | - | - | - | 9.3 | 0.002 | - | |
| After removing three surveys with only anti-HBc positive cases | 499 (84, 172) | 11.78 | 2.24 - 43.77 | 94.7 | < 0.001 | 96.8 | |
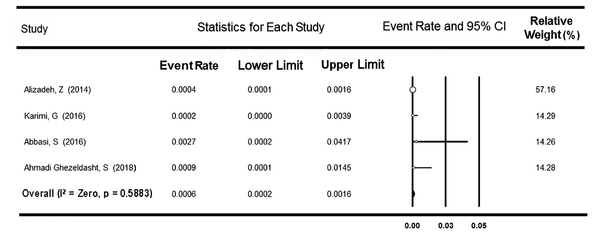
The second group included 7,760 donors from four provinces. There was no heterogeneity between the studies (P = 0.588), and the rate of OBI prevalence was assessed as low as 0.06% (95% CI: 0.02 - 0.16%, Figure 3). A meta-regression analysis indicated no significant time trend in the OBI prevalence rate among both subpopulations of BDs (P = 0.967 and P = 0.510, respectively).
Forest plot of studies on occult hepatitis B infection prevalence among Iranian blood donors regardless of their anti-HBc test results
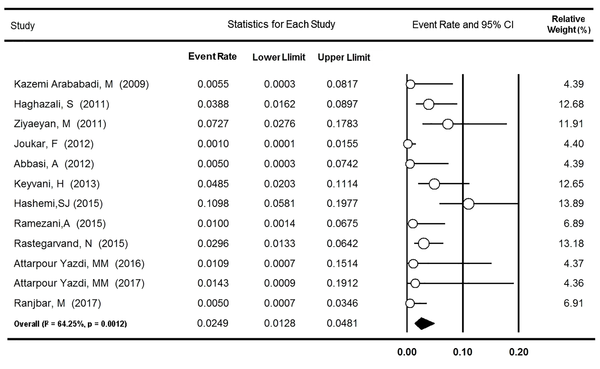
3.2. OBI Prevalence Among Hemodialysis Patients
Twelve surveys from eight provinces of Iran reported the rate of OBI among 1,648 HD patients. Based on heterogeneity found between the studies (P = 0.001, I2 = 64.2%), the prevalence rate was estimated to be 2.49% (95% CI: 1.28 - 4.81%, Figure 4). After excluding one survey assessing OBI among only patients with isolated anti-HBc (39), no significant change occurred in the value of I-square (67.3%) and OBI prevalence (2.12%; 95% CI: 0.98 - 4.54%). As Table 2 indicates, the rate of OBI was higher in the nested PCR subgroup (5.58% [95% CI: 1.29 - 22.75%]) than in the real-time and conventional PCR subgroups (1.98% [95% CI: 0.44 - 8.43%] and 1.01% [95% CI: 0.28 - 3.53%], respectively, P = 0.024). In addition, no significant change over the years was found in the OBI prevalence among Iranian HD patients (P = 0.946).
Forest plot of studies on occult hepatitis B infection prevalence among Iranian hemodialysis patients
3.3. OBI Prevalence Among HCV-Positive Patients
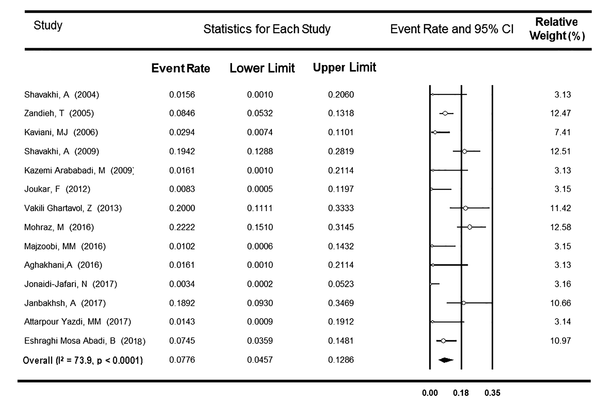
A total of 14 surveys from six provinces of Iran reported the OBI prevalence among 1,029 anti-HCV-positive patients. Considering heterogeneity found between the studies (P < 0.001, I2 = 73.9%), the rate of OBI prevalence was estimated at 7.76% (95% CI: 4.57 - 12.86%) (Figure 5). Based on the meta-analysis of only six studies that reported occult infection among 561 anti-HCV- and HCV RNA-positive patients, the OBI prevalence was estimated to be 8.77% (95% CI: 4.01 - 18.11%) (Table 2). After excluding two surveys assessing OBI among only anti-HBc-positive patients (54, 58), no change was observed in both I-square (74.8%) and OBI frequency (7.32%; 95% CI: 4.10 - 12.75%). Among the remaining 12 studies, a subgroup analysis was done to assess the modulating effect of three different methods used to detect serum HBV DNA, including conventional, nested, and real-time PCR (Table 2). The rates of OBI were apparently higher in real-time and nested PCR subgroups (17.01% [95% CI: 6.96 - 35.95%] and 12.85% [95% CI: 7.70 - 20.67%], respectively) than in conventional PCR subgroup (1.51% [95% CI: 0.54 - 4.16%], P < 0.001). Besides, no significant relationship was detected between the year of the study and the OBI prevalence rate among Iranian HCV-positive patients (P = 0.058).
Forest plot of studies on occult hepatitis B infection prevalence among Iranian HCV-positive patients
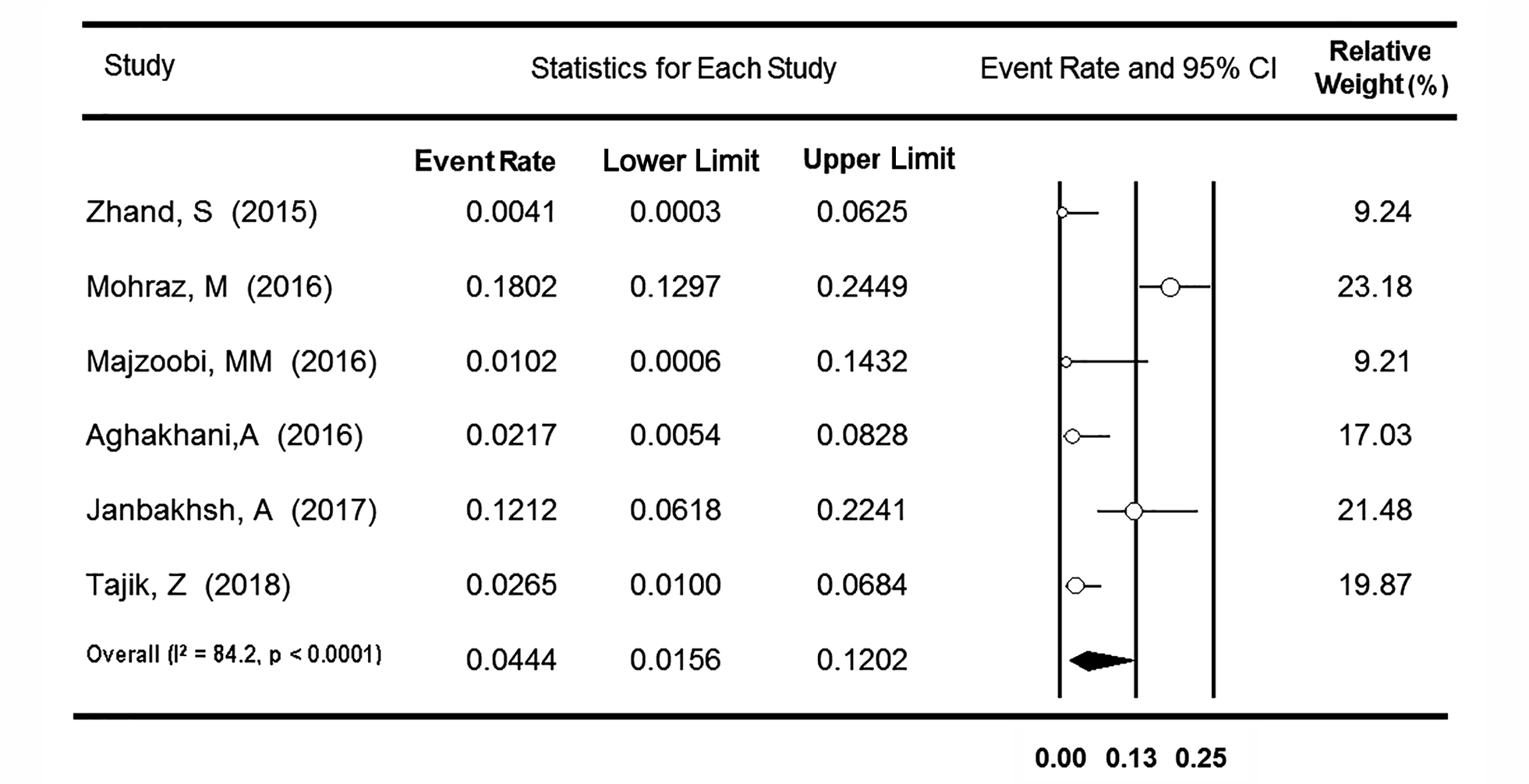
3.4. OBI Prevalence Among HIV-Positive People
Regarding the OBI prevalence among the Iranian population with HIV infection, seven surveys reported the rate among 733 HIV-positive cases from five provinces. Based on heterogeneity detected between the studies (P < 0.001, I2 = 94.8%), the OBI frequency was estimated at 6.91% (95% CI: 1.90 - 22.17%). After excluding one survey that reported an unexpectedly high rate of OBI (63.1%) (59), the value of I-square was declined to 84.2%, and the OBI rate decreased to 4.44% (95% CI: 1.56 - 12.02%) (Figure 6). A subgroup analysis was applied to the remaining six surveys regarding the different molecular methods used to diagnose serum HBV DNA (Table 2). The rate of OBI was significantly higher in the real-time PCR subgroup (6.95% [95% CI: 2.57 - 17.45%]) than in the conventional PCR subgroup (0.65% [95% CI: 0.06 - 6.54%], P = 0.002). After removing three studies that evaluated OBI among only the cases with anti-HBc seropositivity (54, 55, 58), the data from the other four surveys were analyzed. With no change in the value of I-square (96.8%), the rate of OBI prevalence increased to 11.78% (95% CI: 2.24 - 43.77%). A meta-regression analysis showed no significant time trend in the OBI prevalence rate among Iranian HIV-positive individuals (P = 0.599).
Forest plot of studies on occult hepatitis B infection prevalence among Iranian HIV-positive individuals
3.5. OBI Prevalence Among Other Groups
As shown in Table 1, the rate of OBI prevalence has been reported as about 10% in both children and adults from the general Iranian population (21, 22). Likewise, one study among cornea donors in Tehran indicated that 12.2% had molecular evidence of occult infection in their sera (28). The prevalence rate of OBI among PWID ranged from 7.4% to 22% in Tehran (11, 13, 51) while it was as high as 17.9% among this population from Kermanshah (58). Regarding OBI among MTPs, one survey found no cases of OBI among thalassemia patients (43), but another study reported a rate of 9.3% among hemophilia patients (42). Similarly, one survey detected only two cases of OBI among 104 patients with non-cirrhotic cryptogenic hepatitis (45); however, another survey reported a rate of 14% among patients with cryptogenic cirrhosis (46). A considerably high frequency of OBI (28%) was observed among children born to HbsAg-positive mothers (48). In another study, HBV DNA was detected in the serum of 29.2% of individuals with a history of chronic HBV infection who experienced HBsAg seroconversion (49). Moreover, 2-3% of healthcare personnel in Tehran had OBI (29, 30).
4. Discussion
The prevalence of OBI in each population depends partly on the studied people, the prevalence of HBV infection and its risk factors in the community, as well as the sensitivity of techniques used for the detection of serum HBsAg and DNA (64-66). In countries with high endemicity of HBV infection, where the majority of infections occur perinatally or during early childhood, a higher percentage of affected adults might have chronic HBV infection while they are not seroreactive for HBsAg (67). In two systematic reviews of studies conducted in 25 years from 1990 to 2014 (68, 69), the overall rates of HBV infection among the general population of Iran were estimated at 2.2% to 3%, ranging from 0.7% and 0.9% in Kermanshah and Kurdistan provinces, respectively, to 8.9% in Golestan Province. Therefore, Iran could be considered a country with a low-intermediate level of HBV infection. The current systematic review showed a significant variation in the OBI prevalence reported from different provinces of Iran, as well as among diverse populations in the same province. In a study by Azarkar et al. (22), 596 out of 5,234 people selected from the general population of Birjand, South Khorasan, were seroreactive for anti-HBc, of whom 10.2% were detected to be seropositive for HBV DNA. In addition, Ghaziasadi et al. (70) showed that 9.7% of HBsAg- and anti-HBc-negative children in Alborz, Markazi Province, were HBV DNA positive.
Today, OBI is the leading cause of HBV infection following blood transfusion in countries with both low and high levels of HBV endemicity (71). The prevalence of OBI among HbsAg-negative blood donors depends on the level of HBV infection in the community, as well as the serological or molecular methods used to screen the virus (6, 72). The OBI frequency has been reported in 0.1 to 2.4% of HbsAg-negative and anti-HBc-positive blood donor volunteers in western communities with a 5% rate of previous HBV exposure. On the other hand, up to 6% of the donors in HBV-endemic areas, where 70% to 90% of the population show evidence of HBV exposure, are OBI-positive (73). In the present meta-analysis, the prevalence of OBI was estimated at 8.81% (95% CI: 4.11 - 17.91%) among anti-HBc-positive BDs of Iran; however, it was assessed as low as 0.06% (95% CI: 0.02-0.16%) among BDs regardless of their serum anti-HBc status. The detection rate of serum HBV DNA among Iranian HbsAg-negative blood donors varied from 0.15% in Tehran (9) to 2.72% in Zahedan (47). This variation can be partly explained by different prevalence rates of overt HBV infection among BDs from different parts of Iran. In a systematic review of studies with at least 1,000 samples during 2000 - 2015 (74), the overall frequency of HBsAg seropositivity in Iranian blood donors was estimated to be 0.6% (95% CI: 0.4 - 0.8%); however, the prevalence varied from 0.11% in Chaharmahal and Bakhtiari Province to 2.4% in Golestan Province.
Studies showed that occult hepatitis B is mainly found among populations at risk of HBV infection and those with liver disease (2, 6). Similarly, the prevalence of HBsAg seropositivity is reported to be high among high-risk populations of Iran. A review of studies published from 2003 to 2015 (75) estimated the average prevalence rate of 4.8% for HBV infection among drug abusers, PWID, prisoners, and prostitutes in Iran, with the highest prevalence (24.7%) among PWID in Tehran. The HD patients are at risk of acquisition of parenterally transmitted infections. A review of studies published during 1985 - 2015 showed that up to 40% of Iranian HD patients were suffering from HBV infection with an average prevalence of 4% (76). The repetitive blood transfusions, repeated invasive procedures, low response to HBV vaccination, and immunosuppression status are proposed as the reasons for a high incidence of hepatitis B in these patients (77, 78). Moreover, chronic HCV infection in some HD patients may complicate the condition (79). Consistently, the prevalence of OBI has been reported to be up to 36% in HD patients and up to 10% in patients with continuous peritoneal dialysis (6, 77). In 1997, Cabrerizo et al. (80) found HBV DNA in 58% of sera samples and 54% of peripheral blood mononuclear cells derived from 33 HbsAg-negative HD patients. The researchers concluded that the absence of HBsAg in dialysis patients could be due to the presence of HBV surface antigen-antibody immune complex or mutations in the S gene of HBV that precluded HBsAg from being identified by conventional methods. The prevalence of OBI in HD patients varies from country to country in the Middle East. It is reported as 4.1% in Egypt (81). In a study from Turkey (82), OBI was reported in 12 out of 33 HD patients with chronic HCV; however, in other dialysis units from this country, the results were negative (83). Based on the current meta-analysis, the prevalence of OBI among HD patients of Iran was estimated at 2.49% (95% CI: 1.28 - 4.81%) with the highest rate (11%) in patients from Khuzestan Province.
There are significant reports that OBI is more common in people with chronic liver disease, especially those with chronic HCV infection (2, 66, 84). The presence of OBI in patients with chronic hepatitis C has been repeatedly reported and the possible role of OBI in the progression of liver damage following HCV infection has been discussed (78). Cacciola et al. (85) detected the HBV genome in the liver tissue of 33% of patients with HCV infection compared to 14% of HCV-negative groups. In a review, Brechot et al. (64) concluded that HBV DNA was detectable by the PCR technique among 20% - 30% of serum samples of anti-HCV-positive patients and 40% - 50% of liver samples. In the present meta-analysis, the prevalence of OBI among Iranian HCV-positive patients was predicted as 7.76% (95% CI: 4.57 - 12.86%). As hepatitis B and C are common infections with the same transmission routes and risk factors, it is expected that a substantially high prevalence of OBI is reported among patients with chronic hepatitis C (86, 87). Moreover, OBI has shown to worsen the clinical course of HCV infection. Indeed, there is a higher degree of inflammatory activity and fibrosis and a greater rate of cirrhosis and HCC in HCV patients with OBI (88, 89). This clinical consequence of OBI is likely due to the integration of HBV into the host genome or the production of pro-oncogenic proteins by the HBV-free genome within the liver (90). Cacciola et al. (85) reported that 33% of patients with HCV infection and OBI were cirrhotic compared to 19% of those patients with no evidence of occult infection. In addition, it is reported that occult hepatitis B may lead to increased HCV RNA load and serum transaminases levels (90).
Due to similar transmission routes and risk factors, HBV/HIV co-infection is a common condition. Several studies indicated a higher prevalence of HBsAg seropositivity among HIV-positive patients than among HIV-negative individuals (91, 92). The current investigations showed different rates of OBI in HIV-positive groups ranging from zero to 89%; however, the prevalence remains controversial (6, 93, 94). In our systematic review, the prevalence of OBI in HIV-positive patients was estimated to be 6.91% (95% CI: 1.90 - 22.17%); however, a lower rate (4.44%, 95% CI: 1.56 - 12.02%) was discovered after excluding one survey with a high rate of OBI. Some researchers believe that the reasons for diversity observed in OBI prevalence among HIV-positive patients are the same as seen in HIV-negative individuals. These include the different incidence and risk factors of HBV infection in the general population, as well as various methods applied to measure serum HBsAg and/or HBV DNA (6, 94). However, differences between reports may also be explained by fluctuations in HBV proliferation over time, the coincidence of HCV infection, or the impacts of therapeutic strategies for both HIV and HBV. Additionally, heterogeneity between the study populations and regional differences in the overall prevalence of HBV infection may contribute to the observed variance in the prevalence of OBI. HIV patients with OBI might have lower CD4 counts and high plasma HIV RNA loads (93). Reactivation of occult infection and HBsAg seroconversion could also occur with immunosuppression conditions. Thus, the clinical importance of OBI in HIV-positive individuals should be emphasized (90).
5. Limitation
In this review, we tried to address the heterogeneity between studies among different populations through excluding studies with high impacts on the prevalence rates and performing subgroup analysis, as well as meta-regression methods. However, other sources of heterogeneity were impossible to discover.
6. Conclusions
This review estimated the high rates of OBI frequency among high-risk populations of Iran. It is strongly suggested that occult hepatitis B be investigated among Iranian populations with a high chance of its occurrences such as dialysis patients, HCV-positive patients, and HIV-infected individuals.
References
-
1.
Raimondo G, Allain JP, Brunetto MR, Buendia M, Chen D, Colombo M, et al. Statements from the Taormina expert meeting on occult hepatitis B virus infection. Journal of Hepatology. 2008;49(4):652-7.
-
2.
Raimondo G, Navarra G, Mondello S, Costantino L, Colloredo G, Cucinotta E, et al. Occult hepatitis B virus in liver tissue of individuals without hepatic disease. Journal of Hepatology. 2008;48(5):743-6. [PubMed ID: 18314221]. https://doi.org/10.1016/j.jhep.2008.01.023.
-
3.
Allain JP. Occult hepatitis B virus infection. Transfusion Clinique et Biologique. 2004;11(1):18-25.
-
4.
Candotti D, Allain J. Transfusion-transmitted hepatitis B virus infection. Journal of Hepatology. 2009;51(4):798-809.
-
5.
Abdelmalek MF, Pasha TM, Zein NN, Persing DH, Wiesner RH, Douglas DD. Subclinical reactivation of hepatitis B virus in liver transplant recipients with past exposure. Liver Transplantation. 2003;9(12):1253-7.
-
6.
Gutiérrez-García ML, Fernandez-Rodriguez CM, Lledo-Navarro JL, Buhigas-Garcia I. Prevalence of occult hepatitis B virus infection. World Journal of Gastroenterology: WJG. 2011;17(12):1538-42.
-
7.
Shi Y, Wu YH, Wu W, Zhang WJ, Yang J, Chen Z. Association between occult hepatitis B infection and the risk of hepatocellular carcinoma: a meta‐analysis. Liver International. 2012;32(2):231-40.
-
8.
Manzano-Alonso ML, Castellano-Tortajada G. Reactivation of hepatitis B virus infection after cytotoxic chemotherapy or immunosuppressive therapy. World Journal of Gastroenterology: WJG. 2011;17(12):1531.
-
9.
Amini Kafi-abad S, Talebian A, Moghtadaie M, Ranjbar Kermani F, Ferdowsian F, Samie S, et al. Detection of hepatitis B virus DNA (PCR) in HBsAg negative, anti-HBc positive blood donors in Tehran province. The Scientific Journal of Iranian Blood Transfusion Organization. 2007;3(5):379-87.
-
10.
Jonaidi-Jafari N, Rezaee-Zavareh MS, Tavallaei-Nosratabadi J, Ajudani R, Ramezani-Binabaj M, Karimi-Sari H, et al. Occult Hepatitis B Infection in Hepatitis C Patients with Hematological Disorders. Jundishapur Journal of Microbiology. 2017;10(2). e40816.
-
11.
Mohraz M, Jafari R, Poortahmasebi V, Sadeghi A, Hajabdolbaghi M, Rasoolinejad M, et al. Molecular analysis of occult hepatitis B infection among Iranian HIV-positive patients. Future Virology. 2016;11(7):497-508. https://doi.org/10.2217/fvl-2016-0032.
-
12.
Vakili Ghartavol Z, Alavian SM, Amini S, Vahabpour R, Bahramali G, Mostafavi E, et al. Prevalence of occult hepatitis B virus in plasma and peripheral blood mononuclear cell compartments of patients with chronic hepatitis C infection in tehran-iran. Hepatitis Monthly. 2013;13(5). e10134. [PubMed ID: 23967017]. [PubMed Central ID: PMCPmc3741907]. https://doi.org/10.5812/hepatmon.10134.
-
13.
Asli M, Kandelouei T, Rahimyan K, Davoodbeglou F, Vaezjalali M. Characterization of occult hepatitis B infection among injecting drug users in Tehran, Iran. Hepatitis Monthly. 2016;16(3). e34763.
-
14.
Ahmadi Ghezeldasht S, Tehranian F, Mosavat A, Hedayati-Moghaddam MR. Prevalence of hepatitis B core antibody seropositivity and occult hepatitis B in blood donors of Mashhad. The First National Conference of Blood Borne Infections. October 24-26, 2017; Mashhad, Iran. 2018. 68 p.
-
15.
Karimi G, Zadsar M, Vafaei N, Sharifi Z, Falahtafti M. Prevalence of antibody to Hepatitis B core antigen and Hepatitis B virus DNA in HBsAg negative healthy blood donors. Virology Journal. 2016;13(1):36. https://doi.org/10.1186/s12985-016-0492-8.
-
16.
Abbasi S, Makvandi M, Karimi G, Neisi N. The Prevalence of SEN Virus and Occult Hepatitis B (OBI) Virus Infection Among Blood Donors in Ahvaz City. Jundishapur Journal of Microbiology. 2016;9(7).
-
17.
Vaziri M, Javadzadeh Shahshahani H. O74 Frequency of HBc-Ab, HBs-Ab and HBV-DNA among HBs-Ag negative healthy blood donors in Yazd. 7th International Tehran Hepatitis Conference (THC7). Septmber 6-8, 2017; Tehran, Iran. 2017. 12 p.
-
18.
Pourazar A, Salehi M, Jafarzadeh A, Kazemi Arababadi M, Oreizi F, Shariatinezhad K. Detection of HBV DNA in HBsAg negative normal blood donors. Iranian Journal of Immunology. 2005;2(3):172-6.
-
19.
Behzad-Behbahani A, Sabrfirozi M, Eghbali H, Nejabat N, Abbasfard Z, Amirzadeh S, et al. Hepatitis B virus DNA load and genetic characterization of HBsAg S-region isolated from Iranian blood donors with occult infection. The 4th International & 9th National Congress on Quality Improvement in Clinical Laboratories. April 20-23, 2011; Tehran, Iran. 2011.
-
20.
Kazemi Arababadi M, Pourfathollah AA, Jafarzadeh A, Hassanshahi G, Afrooz MR, Hadadian M. Occult HBV infection in Rafsanjanese blood donors. Pathobiology Research. 2009;11(3-4):81-6.
-
21.
Ghaziasadi A, Soleimani A, Alavian SM, Aghcheli B, Gharavi MJ, Fakhari Z, et al. Characterization of OBI prevalence among vaccinated children from Alborz general Population, Iran; vertical OBI, myth or truth? 7th International Tehran Hepatitis Conference (THC7). Septmber 6-8, 2017; Tehran, Iran. 2017. 21 p.
-
22.
Azarkar Z, Ziaee M, Ebrahimzadeh A, Sharifzadeh G, Javanmard D. Epidemiology, risk factors, and molecular characterization of occult hepatitis B infection among anti-hepatitis B core antigen alone subjects. Journal of Medical Virology. 2019;91(4):615-22. [PubMed ID: 30345529]. https://doi.org/10.1002/jmv.25343.
-
23.
Shahabi M, Sayadpour Zanjani D, Tabatabaee A, Khayami MA, Shakibaei H, Bazargani R. Anti-HBc, viral markers and occult hepatitis B infection in blood donors of Mashhad. Iranian Journal of Infectious Diseases. 2009;14(1):21-5.
-
24.
Alizadeh Z, Milani S. Occult Hepatitis B Virus Infection among Iranian Blood Donors: A Preliminary Study. Archives of Iranian Medicine. 2014;17(2):106-7. [PubMed ID: 1511118043; 24527970].
-
25.
Khamesipour A, Mohtasham Amiri Z, Amini Kafiabad S, Saadat F, Mansour-ghanaei F, Esteghamati A, et al. Frequency of hepatitis B virus DNA in anti-HBc positive, HBsAg negative blood donors in Rasht, northern Iran. Transfusion and Apheresis Science. 2011;45(2):195-7. https://doi.org/10.1016/j.transci.2011.08.005.
-
26.
Behzad-Behbahani A, Mafi-Nejad A, Tabei SZ, Lankarani KB, Torab A, Moaddeb A. Anti-HBc & HBV-DNA detection in blood donors negative for hepatitis B virus surface antigen in reducing risk of transfusion associated HBV infection. Indian Journal of Medical Research. 2006;123(1):37-42. [PubMed ID: 16567866].
-
27.
Vaezjalali M, Rashidpour S, Rezaee H, Hajibeigi B, Zeidi M, Gachkar L, et al. Hepatitis B viral DNA among HBs antigen negative healthy blood donors. Hepatitis Monthly. 2013;13(3).
-
28.
Samiee S, Kanavi MR, Javadi MA, Bagheri A, Balagholi S, Hashemi MS. Real Time Polymerase Chain Reaction for Hepatitis B Screening in Donor Corneas in the Central Eye Bank of Iran. Journal of Ophthalmic & Vision Research. 2018;13(4):392-6. [PubMed ID: 30479707]. [PubMed Central ID: PMCPmc6210878]. https://doi.org/10.4103/jovr.jovr_157_17.
-
29.
Ahmad Akhoundi MS, Momeni N, Norouzi M, Ghalichi L, Shamshiri AR, Alavian SM, et al. Prevalence of blood-borne viruses among Iranian dentists: Results of a national survey. International Journal of Occupational Medicine and Environmental Health. 2015;28(3):593-602. [PubMed ID: 26190734]. https://doi.org/10.13075/ijomeh.1896.00324.
-
30.
Borzooy Z, Jazayeri SM, Mirshafiey A, Khamseh A, Mahmoudie MK, Azimzadeh P, et al. Identification of occult hepatitis B virus (HBV) infection and viral antigens in healthcare workers who presented low to moderate levels of anti-HBs after HBV vaccination. Germs. 2015;5(4):134-40. [PubMed ID: 26716102]. [PubMed Central ID: PMCPmc4691194]. https://doi.org/10.11599/germs.2015.1081.
-
31.
Abbasi A, Tajbakhsh R, Kabotari M, Zhand S, Tabarraei A. Occult hepatitis B virus infection in chronic hemodialysis patients in Panje-Azar Hospital, Gorgan. Medical Laboratory Journal. 2012;6(1):7-12.
-
32.
Joukar F, Mansour‐Ghanaei F, Besharati S, Khosh‐Sorur M. Occult hepatitis B infection in a hemodialysis population in Guilan province, northern Iran. Hemodialysis International. 2012;16(2):294-7.
-
33.
Kazemi Arababadi M, Hassanshahi G, Yousefi H. HBV-DNA in hemodialysis patients infected by HCV. Saudi Journal of Kidney Diseases and Transplantation. 2009;20(3):398-401.
-
34.
Attarpour Yazdi MM. Prevalence of occult HBV infection in haemodialysis patients with chronic HCV in the province of Yazd (Iran). The 9th International Iranian Congress of Laboratory and Clinic. February 22-25, 2016; Tehran, Iran. 2017. p. PV-22.
-
35.
Attarpour Yazdi MM. Prevalence of occult HBV infection in haemodialysis patients with chronic HCV in the province of Tehran (Iran). Yazd, Iran. 2016.
-
36.
Ramezani A, Aghasadeghi MR, Ahmadi F, Razeghi E, Eslamifar A, Banifazl M, et al. Isolated anti-hbc and occult HBV infection in dialysis patients. Nephro-Urology Monthly. 2015;7(1).
-
37.
Rastegarvand N, Makvandi M, Samarbafzadeh A, Rasti M, Neisi N, Pouremamali A, et al. Molecular Characterization of Pre-Core/Core and S Region of Hepatitis B Virus in Hemodialysis Patients With Occult Hepatitis B Infection. Jundishapur Journal of Microbiology. 2015;8(10):1. [PubMed ID: 1749597556; 26587212]. https://doi.org/10.5812/jjm.23686.
-
38.
Haghazali S, Aslanimehr M, Charkhchian M, Alizadeh-Kavashkoohi S, Khabaz F, Rajabkhani Z, et al. Occult HBV infection in hemodialysis patients in Qazvin. Razi Journal of Medical Sciences. 2011;18(8):8-14.
-
39.
Keyvani H, Agah S, Kabir A, Alavian SM. Prevalence and risk factors of isolated anti-HBc antibody and occult hepatitis B infection in hemodialysis patients: A nationwide study. Annals of Hepatology. 2013;12(2):213-9.
-
40.
Ziyaeyan M, Aliabadi N. Investigation of hepatitis B virus occult infection in patients of a hemodialysis center in Fasa, Southern Iran. 4th International Tehran Hepatitis Congress. November 23-25, 2011; Tehran, Iran. 2011. 96 p.
-
41.
Hashemi SJ, Hajiani E, Masjedizadeh A, Makvandi M, Shahbazian H, Shayesteh A, et al. A Case-Control Study on Occult Hepatitis B Infection in Chronic Hemodialysis Patients from South-West of Iran. Govaresh. 2015;20(1):135-40.
-
42.
Ziaee M, Javanmard D, Namaei MH. Characterization of occult HBV infection (OBI) among hemophiliacs in The South Khorasan, Iran. Birjand Hepatitis Conference (BHC1). September 10, 2017; Birjand, Iran. 2017. 91 p.
-
43.
Kazemi Arababadi M, Hassanshahi G, Yousefi H, Rezazadeh Zarandi E, Moradi M, Mahmoodi M. No Detected Hepatitis B Virus-DNA in Thalassemic Patients Infected by Hepatitis C Virus in Kerman Province of Iran. Pakistan Journal of Biological Sciences. 2008;11(13):1738-41. [PubMed ID: 18819629]. https://doi.org/10.3923/pjbs.2008.1738.1741.
-
44.
Makvandi M, Neisi N, Khalafkhany D, Makvandi K, Hajiani E, Shayesteh AA, et al. Occult hepatitis B virus among the patients with abnormal alanine transaminase. Jundishapur Journal of Microbiology. 2014;7(8):e11648.
-
45.
Kaviani MJ, Behbahani B, Mosallaii MJ, Sari-Aslani F, Taghavi SA. Occult hepatitis B virus infection and cryptogenic chronic hepatitis in an area with intermediate prevalence of HBV infection. World Journal of Gastroenterology. 2006;12(31):5048-50.
-
46.
Hashemi SJ, Hajiani E, Masjedizadeh A, Makvandi M, Shayesteh AA, Alavinejad SP, et al. Occult hepatitis B infection in patients with cryptogenic liver cirrhosis in southwest of iran. Jundishapur Journal of Microbiology. 2015;8(3).
-
47.
Sharifi-Mood B, Sanei-Moghaddam E, Ghasem-Zadeh I, Khosravi S. Occult Hepatitis B virus Infection among Anti-HBc only Positive Individuals in the Southeast of Iran in high prevalence of HBV Infection Region. Iranian Red Crescent Medical Journal. 2009;11(1):90-2.
-
48.
Shahmoradi S, Yahyapour Y, Mahmoodi M, Alavian SM, Fazeli Z, Jazayeri SM. High prevalence of occult hepatitis B virus infection in children born to HBsAg-positive mothers despite prophylaxis with hepatitis B vaccination and HBIG. Journal of Hepatology. 2012;57(3):515-21. https://doi.org/10.1016/j.jhep.2012.04.021.
-
49.
Ayatollahi J, Kargar Shooroki V, Doosti M, Shahcheraghi SH, Heidari FS, Hemati S, et al. Investigation of Prevalence of HBV DNA in the Individuals of Negative HBs Ag in Yazd, Iran. SN Comprehensive Clinical Medicine. 2019;1(3):183–187.
-
50.
Shavakhi A. Frequency of HBV DNA seropositivity in serum and tissue of patients with hepatitis C in Taleghani Hospital, 2003-2004. Tehran: Shahid Beheshti University of Medical Sciences; 2004.
-
51.
Eshraghi-Mosaabadi B, Kandelouei T, Eslami G, Asli M, Vaezjalali M. Prevalence and risk factors for occult hepatitis B and HIV infections among HCV infected intravenous drug users, Tehran, Iran. Archives of Clinical Infectious Diseases. 2018;13(6). e67968.
-
52.
Zandieh T, Cohan N, Samiei S, Amini S, Ataei Z, Kavari M. Characteristics and prevalence of occult hepatitis B virus infection in patients with hepatitis C in Iran. Medical Journal of the Islamic Republic of Iran (MJIRI). 2005;19(2):147-51.
-
53.
Shavakhi A, Norinayer B, Esteghamat FS, Seghatoleslami M, Khodadustan M, Somi MH, et al. Occult hepatitis B among Iranian hepatitis C patients. Journal of Research in Medical Sciences. 2009;14(1):13-7.
-
54.
Majzoobi MM, Hashemi SH, Mahjoob H, Khakizadeh S, Nikbakht M. Occult Hepatitis B in Patients Co-Infected With Hepatitis C and Human Immunodeficiency Viruses. Avicenna Journal of Clinical Microbiology and Infection. 2016;3(4).
-
55.
Zhand S, Karami C, Hosseinzadeh Adli A, Rostamian G, Tabarraei A, Moradi A. Occult hepatitis B virus infection in HIV infected patients of Iran. 6th Tehran Hepatitis Congress. May 27-29, 2015; Tehran, Iran. 2015. O247 p.
-
56.
Aghakhani A, Mohraz M, Aghasadeghi MR, Banifazl M, Vahabpour R, Karami A, et al. Occult hepatitis B virus infection and S gene escape mutants in HIV-infected patients after hepatitis B virus vaccination. International Journal of STD & AIDS. 2016;27(11):967-72. [PubMed ID: 26384943]. https://doi.org/10.1177/0956462415602419.
-
57.
Tajik Z, Bokharaei-Salim F, Ghorbani S, Keyvani H, Esghaei M, Monavari SH, et al. Detection of HBV genome in the plasma and peripheral blood mononuclear cells of Iranian HBsAg negative patients with HIV infection: occult HBV infection. Archives of Virology. 2018;163(6):1559-66. [PubMed ID: 29476259]. https://doi.org/10.4103/abr.abr_233_16.
-
58.
Janbakhsh A, Farzinpoor J, Mansouri F, Vaziri S, Sayad B, Afsharian M, et al. Prevalence of Occult Hepatitis B in HIV Positive Patients (Adolescents and Adults) in Kermanshah- Iran. International Journal of Pediatrics. 2017;5(9):5797-803.
-
59.
Honarmand A, Pourahmad M, Solhjoo K, Kohan M, Davami MH, Mostafavi Zadeh SK. Occult hepatitis B demonstrated by anti-HBc and HBV DNA in HIV-positive patients. Reports of Biochemistry & Molecular Biology. 2014;3(1):38-42. [PubMed ID: 1774531294; 26989735].
-
60.
Chenari M, Norouzi M, Ghalichi L, Rezaee A, Yari A, Alavian SM, et al. Characterization of overt and occult hepatitis B virus infection among HTLV‐1 positive healthy carriers in the Northeast of Iran; An HTLV‐I endemic area. Journal of Medical Virology. 2014;86(11):1861-7.
-
61.
Azizolahi B, Rajaei E, Taherkhani R, Makvandi M. Low detection of hepatitis B and occult hepatitis B infection in patients with rheumatic diseases. The Egyptian Rheumatologist. 2017;39(4):239-43. https://doi.org/10.1016/j.ejr.2017.04.009.
-
62.
Ghorbani Bejandi S, Jazayeri SM, Ghorbani S, Pourtahmaseb V, Norouzi M, Aghcheli B, et al. Overt and occult hepatitis B infection (OBI) in behcet’s disease. The 8th International Iranian Congress of Laboratory and Clinic. February 6-8; Tehran, Iran. 2016. p. PV-62.
-
63.
Ranjbar M, Dadkhah M, Bokharaei Salim F, Daneshbodi M, Savaj S, Keyvani H. The Prevalence of Occult HBV Infection Among Hemodialysis Patients of Tehran, Iran. Modern Care Journal. 2017;14(4):1-4.
-
64.
Brechot C, Thiers V, Kremsdorf D, Nalpas B, Pol S, Paterlini-Brechot P. Persistent hepatitis B virus infection in subjects without hepatitis B surface antigen: clinically significant or purely "occult"? Hepatology. 2001;34(1):194-203. [PubMed ID: 11431751]. https://doi.org/10.1053/jhep.2001.25172.
-
65.
Raimondo G, Pollicino T, Cacciola I, Squadrito G. Occult hepatitis B virus infection. Journal of Hepatology. 2007;46(1):160-70. [PubMed ID: 17112622]. https://doi.org/10.1016/j.jhep.2006.10.007.
-
66.
Raimondo G, Caccamo G, Filomia R, Pollicino T. Occult HBV infection. Seminars in Immunopathology. 2013;35(1):39-52. [PubMed ID: 22829332]. [PubMed Central ID: PMCPmc3540364]. https://doi.org/10.1007/s00281-012-0327-7.
-
67.
Said ZN. An overview of occult hepatitis B virus infection. World Journal of Gastroenterology. 2011;17(15):1927-38. [PubMed ID: 21528070]. [PubMed Central ID: PMCPmc3082745]. https://doi.org/10.3748/wjg.v17.i15.1927.
-
68.
Mohammadi Z, Keshtkar A, Eghtesad S, Jeddian A, Pourfatholah AA, Maghsudlu M, et al. Epidemiological profile of hepatitis B virus infection in Iran in the past 25 years; A systematic review and meta-analysis of general population studies. Middle East Journal of Digestive Diseases. 2016;8(1):5-18. [PubMed ID: 26933476]. [PubMed Central ID: PMCPmc4773083]. https://doi.org/10.15171/mejdd.2016.01.
-
69.
Salehi-Vaziri M, Sadeghi F, Almasi Hashiani A, Gholami Fesharaki M, Alavian SM. Hepatitis B virus infection in the general population of Iran: An updated systematic review and meta-analysis. Hepatitis Monthly. 2016;16(4). e35577. [PubMed ID: 27257428]. [PubMed Central ID: PMCPmc4888501]. https://doi.org/10.5812/hepatmon.35577.
-
70.
Ghaziasadi A, Soleimani A, Alavian SM, Aghcheli B, Gharavi MJ, Fakhari Z, et al. Characterization of OBI prevalence among vaccinated children from Alborz general population, Iran; vertical OBI, myth or truth? Birjand Hepatitis Conference (BHC1). September 10, 2017; Birjand, Iran. 2017. 21 p.
-
71.
Lledo JL, Fernandez C, Gutierrez ML, Ocana S. Management of occult hepatitis B virus infection: An update for the clinician. World Journal of Gastroenterology. 2011;17(12):1563-8. [PubMed ID: 21472122]. [PubMed Central ID: PMCPmc3070127]. https://doi.org/10.3748/wjg.v17.i12.
-
72.
Kazemi Arababadi M,, Hassanshahi G, Pourfathollah AA, Zarandi ER, Kennedy D. Post-transfusion occult hepatitis B (OBI): a global challenge for blood recipients and health authorities. Hepatitis Monthly. 2011;11(9):714-8. [PubMed ID: 22235213]. [PubMed Central ID: PMCPmc3234543]. https://doi.org/10.5812/kowsar.1735143X.694.
-
73.
Hollinger FB. Hepatitis B virus infection and transfusion medicine: science and the occult. Transfusion. 2008;48(5):1001-26. [PubMed ID: 18454738]. https://doi.org/10.1111/j.1537-2995.2008.01701.x.
-
74.
Babanejad M, Izadi N, Najafi F, Alavian SM. The HBsAg Prevalence Among Blood Donors From Eastern Mediterranean and Middle Eastern Countries: A Systematic Review and Meta-Analysis. Hepat Mon. 2016;16(3). e35664. [PubMed ID: 27226804]. [PubMed Central ID: PMCPmc4875562]. https://doi.org/10.5812/hepatmon.35664.
-
75.
Almasi-Hashiani A, Ayubi E, Mansori K, Salehi-Vaziri M, Moradi Y, Gholamaliei B, et al. Prevalence of hepatitis B virus infection among Iranian high risk groups: a systematic review and meta-analysis. Gastroenterol Hepatol Bed Bench. 2018;11(2):91-100. [PubMed ID: 29910849]. [PubMed Central ID: PMCPmc5990920].
-
76.
Djalalinia S, Ramezan Ghorbani N, Tajbakhsh R, Modirian M, Esmaeili Abdar Z, Mahdavi Gorabi A, et al. Hepatitis B Virus Infection in Iranian Hemodialysis Patients: a Systematic Review and Meta-Analysis. Iran J Kidney Dis. 2018;12(1):1-9. [PubMed ID: 29421769].
-
77.
Fabrizi F, Messa PG, Lunghi G, Aucella F, Bisegna S, Mangano S, et al. Occult hepatitis B virus infection in dialysis patients: a multicentre survey. Aliment Pharmacol Ther. 2005;21(11):1341-7. [PubMed ID: 15932364]. https://doi.org/10.1111/j.1365-2036.2005.02501.x.
-
78.
Aghakhani A, Banifazl M, Velayati AA, Eslamifar A, Ramezani A. Occult hepatitis B virus infection in hemodialysis patients: a concept for consideration. Therapeutic Apheresis and Dialysis. 2012;16(4):328-33. [PubMed ID: 22817120]. https://doi.org/10.1111/j.1744-9987.2012.01072.x.
-
79.
Hollinger FB, Daneshmand A, Alavian SM; Habibollahi P. Occult Hepatitis B Infection in Chronic Hemodialysis Patients: Current Concepts and Strategy. Hepat Mon. 2010;10(3):199–204.
-
80.
Cabrerizo M, Bartolome J, De Sequera P, Caramelo C, Carreno V. Hepatitis B virus DNA in serum and blood cells of hepatitis B surface antigen-negative hemodialysis patients and staff. J Am Soc Nephrol. 1997;8(9):1443-7. [PubMed ID: 9294837].
-
81.
Abu El Makarem MA, Abdel Hamid M, Abdel Aleem A, Ali A, Shatat M, Sayed D, et al. Prevalence of occult hepatitis B virus infection in hemodialysis patients from egypt with or without hepatitis C virus infection. Hepat Mon. 2012;12(4):253-8. [PubMed ID: 22690232]. [PubMed Central ID: PMCPmc3360934]. https://doi.org/10.5812/hepatmon.665.
-
82.
Besisik F, Karaca C, Akyuz F, Horosanli S, Onel D, Badur S, et al. Occult HBV infection and YMDD variants in hemodialysis patients with chronic HCV infection. J Hepatol. 2003;38(4):506-10. [PubMed ID: 12663244]. https://doi.org/10.1016/s0168-8278(02)00457-9.
-
83.
Goral V, Ozkul H, Tekes S, Sit D, Kadiroglu AK. Prevalence of occult HBV infection in haemodialysis patients with chronic HCV. World J Gastroenterol. 2006;12(21):3420-4. [PubMed ID: 16733862]. [PubMed Central ID: PMCPmc4087876]. https://doi.org/10.3748/wjg.v12.i21.3420.
-
84.
Fukuda R, Ishimura N, Niigaki M, Hamamoto S, Satoh S, Tanaka S, et al. Serologically silent hepatitis B virus coinfection in patients with hepatitis C virus-associated chronic liver disease: clinical and virological significance. J Med Virol. 1999;58(3):201-7. [PubMed ID: 10447413]. https://doi.org/10.1002/(sici)1096-9071(199907)58:3<201::aid-jmv3>3.0.co;2-2.
-
85.
Cacciola I, Pollicino T, Squadrito G, Cerenzia G, Orlando ME, Raimondo G. Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease. N Engl J Med. 1999;341(1):22-6. [PubMed ID: 10387938]. https://doi.org/10.1056/nejm199907013410104.
-
86.
Alavian SM, Jazayeri SM. Other views of occult hepatitis B in Hepatitis C infected patients. Eur J Intern Med. 2011;22(5):e67-8. [PubMed ID: 21925047]. https://doi.org/10.1016/j.ejim.2011.05.003.
-
87.
Habibollahi P, Safari S, Daryani NE, Alavian SM. Occult hepatitis B infection and its possible impact on chronic hepatitis C virus infection. Saudi J Gastroenterol. 2009;15(4):220-4. [PubMed ID: 19794265]. [PubMed Central ID: PMCPmc2981836]. https://doi.org/10.4103/1319-3767.56089.
-
88.
Fernandez-Rodriguez CM, Gutierrez ML, Lledó JL, Casas ML. Influence of occult hepatitis B virus infection in chronic hepatitis C outcomes. World Journal of Gastroenterology: WJG. 2011;17(12):1558.
-
89.
Squadrito G, Cacciola I, Alibrandi A, Pollicino T, Raimondo G. Impact of occult hepatitis B virus infection on the outcome of chronic hepatitis C. Journal of Hepatology. 2013;59(4):696-700.
-
90.
Alavian SM, Miri SM, Hollinger FB, Jazayeri SM. Occult hepatitis B (OBH) in clinical settings. Hepatitis Monthly. 2012;12(8). e6126. [PubMed ID: 23087749]. [PubMed Central ID: PMCPmc3475016]. https://doi.org/10.5812/hepatmon.6126.
-
91.
Lukhwareni A, Burnett RJ, Selabe SG, Mzileni MO, Mphahlele MJ. Increased detection of HBV DNA in HBsAg-positive and HBsAg-negative South African HIV/AIDS patients enrolling for highly active antiretroviral therapy at a Tertiary Hospital. J Med Virol. 2009;81(3):406-12. [PubMed ID: 19152393]. https://doi.org/10.1002/jmv.21418.
-
92.
Mphahlele MJ, Lukhwareni A, Burnett RJ, Moropeng LM, Ngobeni JM. High risk of occult hepatitis B virus infection in HIV-positive patients from South Africa. J Clin Virol. 2006;35(1):14-20. [PubMed ID: 15916918]. https://doi.org/10.1016/j.jcv.2005.04.003.
-
93.
Cohen Stuart JW, Velema M, Schuurman R, Boucher CA, Hoepelman AI. Occult hepatitis B in persons infected with HIV is associated with low CD4 counts and resolves during antiretroviral therapy. J Med Virol. 2009;81(3):441-5. [PubMed ID: 19152397]. https://doi.org/10.1002/jmv.21422.
-
94.
Ramezani A, Banifazl M, Mohraz M, Rasoolinejad M, Aghakhani A. Occult hepatitis B virus infection: A major concern in HIV-infected patients: Occult HBV in HIV. Hepat Mon. 2011;11(1):7-10. [PubMed ID: 22087108]. [PubMed Central ID: PMCPmc3206662].