Abstract
Background:
Team-based learning (TBL) is an active and participatory learning process, which is used to train students on health topics.Objectives:
The present study aimed to assess the effect of TBL in teaching a medical physics course on the poor performance of the students.Methods:
This quasi-experimental study was conducted on 28 medical students at Qom University of Medical Sciences, Iran who were unable to pass the medical physics course in the past semesters. At the beginning the 10-session course, eight questions with four options were provided to the students, and the students had to answer the questions individually within a specified time. After collecting the questionnaire responses, participants were divided into six groups and completed the same test as a team. Afterwards, each question was displayed on a smart board and discussed.Results:
After the procedures of the study, all the participants successfully completed the medical physics course. At the end of the course, 90% of the students reported that the TBL method was more appropriate than lecture, and 80% of the students believed that the TBL method encouraged them to participate in the learning process. In the final exam, the scores of the students in the medical physics course increased by 3.95 ± 2.09 units with the TBL method compared to the prior course, and the difference was considered significant (P < 0.01).Conclusions:
According to the results, the implementation of TBL in the medical physics course improved the learning motivation, satisfaction, and mean scores of the students with poor performance.Keywords
1. Background
Effective training is essential to the promotion of learning in terms of knowledge, skills, and attitude among professionals, such as medical students and paramedics. Today, the development of medical sciences and its widespread use in medical training has further highlighted the need for proper training (1). Teaching and learning methods are important subjects in medical training (2), and significant effort has been made to improve the teaching and learning methods of medical students in the past two decades (3). The awareness of the impact of teaching methods on the learning of students could help teachers to select appropriate methods in order to enhance the quality of teaching (4). Some of the common teaching methods today are lecture, group training, and e-learning (5).
In medical disciplines, teaching is often grounded in lecture (6), which is a method widely used in medical training although it has been criticized for its inefficiency in achieving educational goals (7). In lecture, information is transmitted from the teacher to the students, but there have been no attempts regarding creativity or independent thinking (8). Although lectures provides substantial educational content, effective learning is not achieved due to the lack of active student participation (4).
Educational psychologists believe that the engagement of students in the learning process results in effective teaching and its sustained impact. Therefore, experts emphasize on the use of modern teaching approaches (9), such as student-oriented methods that leads to active learning. Ample evidence suggests that active learning improves understanding as it facilitates the learning process. Active learning occurs when learners find more opportunities for interactive communication with the subject and are encouraged to produce new scientific findings (10). In an active learning environment, teachers often facilitate learning rather than dictating the materials to the learners (11).
Team-based learning (TBL) is an active and participatory method of teaching, which has a distinct structure. Since the 1970s, TBL has been evaluated in various learning environments and used to train professionals on health-related subjects (12). This methodology was introduced by Michaelsen (13) with the goal of improving the quality of learning in students through enhancing problem-solving skills, ensuring the participation of students in the classroom with adequate preparation, and creating energetic and active learning classes. TBL is based on individual and group responsiveness and student participation in group discussions. This method enables the teacher to manage multiple small groups within a classroom (14). Previous findings have indicated group learning creates deeper and better learning (14) and is considered to be more effective compared to lectures (15). TBL reduces stress and work pressure, while increasing the preparedness of students for classroom learning, so that more time would be spent on discussions and interactions in the classroom (16).
Experience shows that numerous medical students consider the medical physics course is extremely difficult; in particular, the students who have poor performance may be unable to pass the course despite repeated attempts.
2. Objectives
For the first time, the present study aimed to assess the effect of TBL in teaching a medical physics course on the students with poor performance.
3. Methods
3.1. Participants
This quasi-experimental study was conducted on the medical students of Qom University of Medical Sciences, Iran. The sample population included 15 and 14 medical students admitted in 2016 and 2017, respectively, who were unable to pass the medical physics course in the past semesters and were highly dissatisfied with the status quo. After obtaining the consent of the students, they were enrolled in the study. Each test group included 80 medical students (two separate 40-person classes), and each participant had been admitted to the university for two consecutive years.
The inclusion criteria of the study were having taken the medical physics course in the past semesters and inability to obtain a passing grade for admission. The number of the students in the class was 39 at the time, and 10 students taking the medical physics course for the first time were not evaluated. Student attendance was monitored throughout the study, and the students who were absent for more than three sessions were dismissed. Finally, the scores of 28 students were evaluated.
3.2. Procedures
The medical physics course selected in this study was regularly taught by a faculty member of the Medical Physics Lecture Group. After completing a TBL workshop before the first session, the professor of the course explained thoroughly how the students should pursue the course, and additional explanations were provided regarding the goals, components, and method of class implementation; questions and possible ambiguities were also addressed. The pages of the book to be studied in each class were announced to the students. Initially, the students were divided into six groups of four or five based on the TBL principles. Each group was assigned an English letter (A, B, or C) as its name. In the subsequent sessions, the students learned that their groups were not permanent. During all the sessions, tips to improve the quality of learning were shared, which were mainly focused on time management, communication and motivation among the students, content comprehensiveness, summing up, drawing conclusions, and answering questions.
The first step in the beginning of each session was an individual preparedness assurance test. At this stage, eight questions with four options were provided to the students, and they were asked to answer the questions individually without using the course book within a specified time. Afterwards, the questionnaires were collected, and the same test was carried out in each team. The teams discussed each question and selected a response that was agreed upon by all the members as the team response. After collecting the responses, each question was displayed on the smart board. Before the answers were discussed, the answers of each group were written on the board. After the correct answers were agreed upon, each group with the score of ≤ 4 were to treat the class to cookies in the next session! After 2 - 3 days, the individual test results were published by the communication group of the class, reported by the name of each group in the form of an Excel file, and ranked from high to low.
In the appeal stage, the students were given the opportunity to express their objections regarding the questions or the way they were designed. At the end of each session, the teacher explained the content that was not covered, as well as ambiguities. The final part of the course was the peer-learner evaluation, which often requires the evaluation of each team member at the end of the classes in accordance with the TBL principles in terms of team performance; notably, the evaluation was not implemented in the classroom.
During the TBL sessions (n = 10), some aspects of the method were discussed with the students. After completing the course and before the final exam, the academic motivation of the study group was evaluated using the Harter’s Motivation questionnaire (HMQ), and the students were asked several questions regarding the use of this method in the medical physics course.
3.3. Harter’s Motivation Questionnaire
HMQ (17) is commonly used for the measurement of academic motivation (18), and the items in the questionnaire are scored based on a five-point Likert scale (never = 1, rarely = 2, sometimes = 3, often = 4, almost always = 5). The standard cutoff scores within the range of 33 - 65 indicate minimal motivation, scores 66 - 98 show moderate motivation, and higher scores than 99 indicate good motivation. The validity and reliability of the Persian version of HMQ have been confirmed in Iran, and the validity coefficient of the retest for the total scale of intrinsic and extrinsic motivation has been estimated at 0.86 and 0.69, respectively. In addition, the Cronbach’s alpha for the total scale of intrinsic and extrinsic motivation has been calculated to be 0.85 and 0.72, respectively (19).
3.4. Statistical Analyses
Paired t-test was used for the comparison of the final exam scores of the students in the medical physics course based on TBL with the prior course. The generalized estimating equations (GEE) test was also applied for the evaluation of all the exams during the 10 sessions of the TBL.
4. Results
All the participants successfully completed the medical physics course. At the end of the course, 90% of the students reported the TBL method to be more effective in their performance compared to lecture. Furthermore, 80% of the students believed that the TBL method encouraged them to participate in the learning process. In terms of teaching and learning principles, 75% of the students reported the TBL method to be more appropriate than lecture. Regarding the skills of the teacher and mastery of teaching, 52.4% of the students selected TBL, 28.6% selected lecture, and 19% considered no difference in this regard.
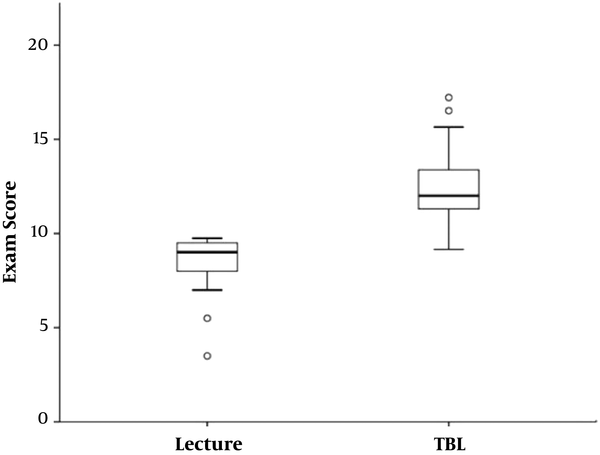
In the final exam, which was in the descriptive and written format, the scores of the students of the medical physics course increased by 3.95 ± 2.09 units with the TBL method compared to the prior course (Figure 1), and the difference was considered significant based on the paired t-test (P < 0.01). Before the current semester, the mean score of all the students in the TBL course was 14.8 ± 1.2. According to the results of independent t-test, the score was significantly lower than the mean score of all the students (16.9 ± 1.7) who had passed the medical physics course (P = 0.005).
Box plot of lecture versus TBL score medical physics course
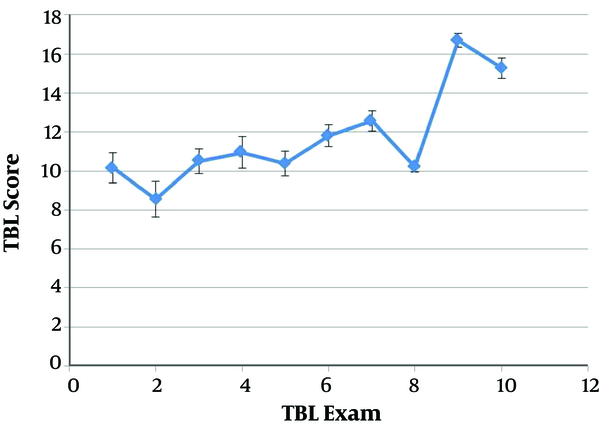
The GEE test showed no significant correlation between the previous total mean score of each student and the score obtained in the TBL-based course (P = 0.497) (Figure 2). The academic motivation of the study group was also evaluated using HMQ, and the results are shown in Figure 3.
The TBL scores during the course, normed to a score of 20
Motivational distribution percentage of students’ studying, based on Harter’s Motivation questionnaire
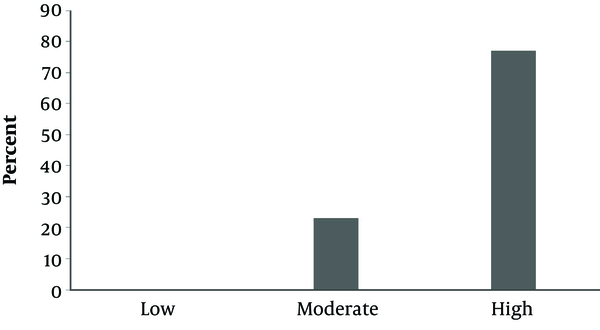
Figure 2 depicts the TBL scores of this class through 10 exams as normed to the score of 20. The GEE analysis indicated that the mean scores of the last two TBL exams (tests 9 and 10) were significantly higher compared to the scores of the other exams (P < 0.001).
5. Discussion
In the present study, the application of the TBL method was compared to the lecture method in the teaching of a medical physics course in the students with poor performance. The classification of these students was based on the comparison of the mean score of each student in the prior semesters with the average of all the students in the class, the outcome of which was considered statistically significant (P = 0.005).
According to our findings, the TBL method could enhance the learning level of the students. All the participants could pass the medical physics course, and based on this analysis, the satisfaction of the students also increased significantly. Furthermore, more than 90% of the students believed that TBL was more effective in learning than the lecture method as it encouraged their participation in the learning process. This is consistent with the previous studies in this regard (5, 20, 21). For instance, Akbari et al. (22) reported that the mean scores of the students who participated in a TBL-based class at a rehabilitation clinic were higher compared to the mean scores of the control group. In addition, 97% of the students in the mentioned study agreed to partake in the course and considered TBL to be useful in the passing of the course. In another research, Vaezie et al. (23) compared TBL and lecture in the teaching-learning process of nursing students, reporting that the satisfaction and mean score of the general tests based on the TBL method were higher compared to the lecture group. In the study by Kumar et al., the majority of students believed that the TBL method helped in the conceptual learning of the course and effectively increased their knowledge and understanding of the concept.
In the present study, TBL resulted in the high satisfaction rate of the students and a significant increase in the grades of the medical physics course over the lecture method. Moreover, all the students could successfully pass the course, which indicated the increased academic efficiency in the medical physics course and higher satisfaction of those who initially had not considered the medical physics course as specialized and necessary. Consequently, the total mean score of the students all the courses was higher compared to the medical students admitted in 2016 and 2017 (P = 0.005).
Few studies have been focused on the impact of TBL on students with poor performance. In a research in this regard, Koles et al. (24) reported that students in the lowest academic quartile may benefit more than other students from the TBL strategy. Yet, mastery of course content enhanced in Medical students’ higher performance (24). If the impact of TBL on the reduction of number of failures could influence the poor performance of students, the results obtained by Brunner et al. confirmed the effectiveness of the method in improving the poor performance of the students (25). Indeed, the mentioned research confirmed the impact of TBL on poorly-qualified students.
The results of paired t-test test showed no significant correlation between the previous grade of each student and the scores obtained in the TBL-based course (P = 0.497) (Figure 1). In other words, no association was observed between the previous grades of the students and their current scores in the medical physics course. Therefore, it could be concluded that TBL could easily influence the performance of weaker students in terms of curriculum. Therefore, the students with lower and higher scores in the medical physics course could not be distinguished based on their average score in the entire previous semester within the range of 12.3 - 17.0, and further investigations on larger sample sizes are required in this regard.
In response to the question “Did the teacher’s skills and mastery influence the choice of the most appropriate method?”, 52.4% of the students selected the TBL method, while 19% considered no difference in this regard. In the current research, the teacher had several years of experience in the teaching of the course by lecture, and this was his first experience of TBL implementation. The reason behind the responses of the students was possibly rooted in deeper learning and better transfer of the educational content (26) as in the TBL methodology, the students may have associated the method with the skill and mastery of the teacher. Notably, 90% of the students believed that the presentation of the medical physics course by the TBL method was more appropriate, and 85% believed that the students are interested in participation in the learning process through TBL, which may support the veracity of their statements.
As can be seen in Figure 2, the average trend of the TBL tests was incremental, and the average grades of the class improved with time, so that the GEE showed a significant increase in the grades, especially in the last two tests compared to the initial tests. These findings were predictable due to the familiarity of the students with the new presentation method (i.e., TBL) although they had not previously experienced TBL in any other courses. One of the reasons behind the incremental score pattern could be the notification of the results of the individual TBL tests since 2 - 3 days after the test, the individual test results of the communication group of the class were labeled from the highest to the lowest in the form of an Excel file. The scores of the student seemed to have prompted them to upgrade their status to the top or maintain their favorable status.
Due to other midterm exams of the classes, the TBL test was not given in one of the sessions, and the volume of test pages doubled for the following exam, totaling 16 questions and 40 pages of the reference books instead of the usual 20 pages. After passing the test, the majority of the students acknowledged that the large volume of the educational material caused a decline in their mastery of the content and difficulty in studying the textbook. Figure 2 shows the effects of the increased volume of the contents in a visible drop in the eighth test. Therefore, it could be concluded that the selection of the appropriate amount of educational contents in the TBL method must be heeded by teachers.
The assessment of the scores of all the students in the medical physics course with the TBL method indicated a significant increase in the scores as measured by t-test compared to the lecture method, which had been used for the same students the previous year (P < 0.01). Our findings in this regard are consistent with several studies (20, 21, 27).
The main limitations of the present study were the small sample size and quantitative statistical volume of Qom University of Medical Sciences, which made it quite difficult to generalize the results to other groups and communities. Another notable point about the improve scores of the students was the possible interference of the new method (TBL) with the previous learning method (lecture), because they were not unable to pass the medical physics course in the past semesters. This study was carried out with the knowledge of these limitations since the primary aim of the study was to increase the active participation and dissatisfaction of students with poor classroom performance. Achieving this goal could improve the performance of students (10, 11, 28, 29).
The main strength of the study was the uniformity of some features with possible effects on the study outcomes, such as the curriculum content, teacher, and especially the study group.
5.1. Conclusions
According to the results, the implementation of TBL in the medical physics course could enhance learning motivation, increase satisfaction, and improve the mean scores of the students with poor performance. Furthermore, the students found TBL to be a more relevant learning method in demanding mathematics-based courses, which resulted in greater participation by more students in the learning process.
Acknowledgements
References
-
1.
Barry Issenberg S, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Medical teacher. 2005;27(1):10-28. [PubMed ID: 16147767]. https://doi.org/10.1080/01421590500046924.
-
2.
Kern DE, Bass EB, Thomas PA, Howard DM. Curriculum development for medical education: a six step approach. Baltimore: JHU Press; 1998.
-
3.
Flexner A. Medical education in the United States and Canada. Bulletin of the World Health Organization. 2002;80:594-602.
-
4.
Biggs JB. Teaching for quality learning at university: What the student does. UK: McGraw-Hill Education; 2011.
-
5.
Bates AT. Technology, e-learning and distance education. USA: Routledge; 2005. https://doi.org/10.4324/9780203463772.
-
6.
Kennedy TJ, Lingard LA. Making sense of grounded theory in medical education. Medical education. 2006;40(2):101-8. [PubMed ID: 16451236]. https://doi.org/10.1111/j.1365-2929.2005.02378.x.
-
7.
Busse H, Aboneh EA, Tefera G. Learning from developing countries in strengthening health systems: an evaluation of personal and professional impact among global health volunteers at Addis Ababa University’s Tikur Anbessa Specialized Hospital (Ethiopia). Globalization and health. 2014;10(1):64. [PubMed ID: 25190076].
-
8.
Magolda MBB. Students' Epistemologies and Academic Experiences: implications for Pedagogy. College Student Development and Academic Life: Psychological, Intellectual, Social and Moral Issues. 2014;15(3):117.
-
9.
Emmer ET, Stough LM. Classroom management: A critical part of educational psychology, with implications for teacher education. Educational psychologist. 2001;36(2):103-12. https://doi.org/10.1207/S15326985EP3602_5.
-
10.
Lee EA, Wong KW, Fung CC. How does desktop virtual reality enhance learning outcomes? A structural equation modeling approach. Computers & Education. 2010;55(4):1424-42. https://doi.org/10.1016/j.compedu.2010.06.006.
-
11.
Cazden CB. The language of teaching and learning. The language of teaching and learning. 2001:348-69.
-
12.
Fatmi M, Hartling L, Hillier T, Campbell S, Oswald AE. The effectiveness of team-based learning on learning outcomes in health professions education: BEME Guide No. 30. Medical teacher. 2013;35(12):e1608-24. [PubMed ID: 24245519].
-
13.
Michaelsen LK. Three keys to using learning groups effectively. Teaching Excellence: Toward the Best in the Academy. 1998;9(5):1997-8.
-
14.
Vasan NS, DeFouw DO, Compton S. A survey of student perceptions of team‐based learning in anatomy curriculum: Favorable views unrelated to grades. Anatomical sciences education. 2009;2(4):150-5. [PubMed ID: 19572279].
-
15.
Freeman S, Eddy SL, McDonough M, Smith MK, Okoroafor N, Jordt H, et al. Active learning increases student performance in science, engineering, and mathematics. Proceedings of the National Academy of Sciences. 2014;111(23):8410-5. [PubMed ID: 24821756].
-
16.
Hazel SJ, Heberle N, McEwen M, Adams K. Team-based learning increases active engagement and enhances development of teamwork and communication skills in a first-year course for veterinary and animal science undergraduates. Journal of veterinary medical education. 2013;40(4):333-41. [PubMed ID: 24077314]. https://doi.org/10.3138/jvme.0213-034R1.
-
17.
Harter S. A new self-report scale of intrinsic versus extrinsic orientation in the classroom: Motivational and informational components. Developmental psychology. 1981;17(3):300. https://doi.org/10.1037/0012-1649.17.3.300.
-
18.
Akbari Balootbangan A, Talepasand S. Validation of the Illinois bullying scale in primary school students of Semnan, Iran. Journal of fundamentals of mental health. 2015;17(4):178-85.
-
19.
Bahrani M. The Study of Validity and Reliability of Harter’s Scale of Educational Motivation. Journal of Psychological Studies. 2009;5(1):51-72. https://doi.org/10.22051/psy.2009.1591.
-
20.
Odell KE. Team-based learning and student performance: Preliminary evidence from a principles of macroeconomics classroom. International Review of Economics Education. 2018. https://doi.org/10.1016/j.iree.2018.01.001.
-
21.
Birk T. A comparison of student responses to team based learning in a first year medical curriculum. Indiana: Indiana University; 2014.
-
22.
Akbari M, Moeintaghavi A, Ghanbari H, Bageri M, Otoufi A. A Comparison of the Students’ and Teachers’ Viewpoints about the Characteristics of a Good Teacher in Dentistry. Journal Management System. 2015;38(4):281-90. https://doi.org/10.22038/jmds.2014.3148.
-
23.
Vaezi AA, Azizian F, Kopayehzadeh J. Survey compare team based learning and lecture teaching method, on learning-teaching process nursing student's, in Surgical and Internal Diseases course. The Journal of Medical Education and Development. 2015;10(3):246-54.
-
24.
Koles PG, Stolfi A, Borges NJ, Nelson S, Parmelee DX. The impact of team-based learning on medical students' academic performance. Academic Medicine. 2010;85(11):1739-45. [PubMed ID: 25449204]. https://doi.org/10.1016/j.eururo.2014.09.054.
-
25.
Nelson M, Allison SD, McCollum M, Luckey SW, Clark DR, Paulsen SM, et al. The Regis Model for pharmacy education: A highly integrated curriculum delivered by Team-Based Learning™(TBL). Currents in Pharmacy Teaching and Learning. 2013;5(6):555-63. [PubMed ID: 20881827]. https://doi.org/10.1016/j.cptl.2013.07.002.
-
26.
Rotellar C, Cain J. Research, perspectives, and recommendations on implementing the flipped classroom. American journal of pharmaceutical education. 2016;80(2):34. [PubMed ID: 27073287]. https://doi.org/10.5688/ajpe80234.
-
27.
Chen M, Ni C, Hu Y, Wang M, Liu L, Ji X, et al. Meta-analysis on the effectiveness of team-based learning on medical education in China. BMC medical education. 2018;18(1):77. [PubMed ID: 29636039]. https://doi.org/10.1186/s12909-018-1179-1.
-
28.
Momeni Danaei S, Zarshenas L, Oshagh M, Omid Khoda SM. Which method of teaching would be better cooperative or lecture? Iranian Journal of Medical Education. 2011;11(1):24-31.
-
29.
Sadeghi R, Sedaghat MM, Sha Ahmadi F. Comparison of the effect of lecture and blended teaching methods on students' learning and satisfaction. J Adv Med Educ Prof. 2014;2(4):146-50. [PubMed ID: 25512938]. [PubMed Central ID: PMC4235559].