Abstract
Introduction:
SARS-CoV2 (COVID-19) is a serious and global infection that has spread to numerous countries, including Iran. Pneumothorax may occur in cases of COVID-19 as a consequence of lung parenchymal damage, which can disrupt the healing process and increase mortality.Case Presentation:
This manuscript describes the case of a 2-year-old boy with hyper IgM syndrome and COVID-19 infection. The patient developed spontaneous pneumothorax and recovered without chest tube by supportive care and was discharged in good general condition after the completion of the antibiotic course and cessation of fever.Conclusions:
The severity, prognosis, and best treatment for spontaneous pneumothorax in COVID-19 infection, especially in children, remain nebulous. It is recommended that conservative treatment be performed if the patient has stable vital signs and no severe respiratory failure. However, this requires more detailed clinical evaluations.Keywords
1. Introduction
SARS-COV-2 (COVID-19) infection is a global epidemic disease, which primarily affects the respiratory system. Since the initial outbreak of the disease in Wuhan, China, in December 2019, the coronavirus (COVID-19) has spread across the globe with the development of acute respiratory syndrome, causing a widespread epidemic. Common symptoms have been identified as fever, cough, shortness of breath, headache, abdominal pain, nausea and vomiting, myalgia, diarrhea, rhinorrhea, fatigue, anosmia, and ageusia (1). However, some infected people can be asymptomatic (2). Spontaneous pneumothorax is an uncommon complication of COVID-19 viral pneumonia, the risk factors of which remain unknown. Spontaneous pneumothorax is characterized by the existence of air in the pleural space that is not caused by trauma or other factors and occurs clinically without lung disease. This condition can be a complication of lung disease. Only rare cases of pneumothorax have been reported as a complication of COVID-19 viral pneumonia. The exact incidence of this complication is not known yet.
In a study published by Yang et al. conducted among 92 patients with COVID-19, 1 (1.1%) case had pneumothorax who died five days after the initial presentation (3). Six out of 902 (0.66%) cases of confirmed COVID-19 pulmonary involvement experienced pneumothorax in the USA (4). Pneumothorax is associated with a poor prognosis in patients infected with the Coronavirus (MERS-CoV) accompanied with acute Middle Eastern respiratory distress syndrome. The clinical course of this disease is generally consistent with the typical pattern of pneumonia induced by COVID-19 (4). This article aimed to describe the critical issues in the diagnosis and treatment of children with COVID-19 respiratory disease accompanied by pneumothorax (5).
2. Case Presentation
A 2-year-old boy with hyper IgM syndrome was admitted to Mofid Children's Hospital PICU in Tehran with a complaint of fever and shortness of breath four days before admission (conscious consent was obtained from the patient's parent before presenting the case report). He had frequent coughs when he arrived and mentioned a history of contact with his grandfather, a positive COVID-19 case. The patient used to have cotrimoxazole syrup for prophylaxis to prevent pneumocystis jiroveci and received monthly IVIG due to the immunoglobulin deficiency. He was ill but not toxic with tachypnea. His vital signs at the time of emergency visit were as follows: PR = 113/min, RR = 90/min, O2sat = 90%, BP = 90/50
The patient was not dehydrated. He had nasal flaring and supra sternal, subcostal, and intercostal retraction. The lungs’ auscultation revealed bilateral sound reduction, fine crackle, and bilateral wheezing. The heart sounds were normal. Echocardiography was normal.
The abdomen was soft with no organomegaly. Chest computed tomography (CT) scan was performed at baseline, and COVID-19 was suspected. The patient received fluid, and normal urine output was established. Peripheral pulses were normal and symmetrical, and muscle tone was normal. The patient underwent oxygen therapy and received methylprednisolone pulse, salbutamol, and fluticasone spray due to respiratory distress. He did not receive antiviral drug for COVID-19. COVID-19 polymerase chain reaction (PCR) virus test was performed due to strong suspicion, and the result was positive. The initial lab test findings are listed (Table 1): WBC = 3100/mm3 with PMN = 68% and Lym = 25%, Hb = 10 mg/dL, PLT = 447000/mm3, Na = 134 (135 - 145 mEq/L), K = 3.8 (3.6 - 5.2 mmol/L), Ca = 8.4 (8.6 - 10.3 mg/dL), Mg = 2.2 (1.7 - 2.2 mg/dL), BUN = 6.7 (7 - 20 mg/dL), Cr = 0.7 (0.7 - 1.2 mg/dL), pH = 7.41, HCO3 = 20 (22 - 28 mEq/L), PCO2 = 24 (38 - 42 mmHg), BE = -4 (-5 - +3), ESR = 58, CRP = 120, AST = 45, ALT = 15. Due to the disease, positive COVID-19 test result, and immunodeficiency, treatment was started.
. Lab Data
| Variables | Values |
|---|---|
| CBC | |
| WBC | 3100 |
| N | 68% |
| L | 25% |
| Hb | 10 |
| PLT | 447000 |
| Electrolyte | |
| Na | 134 |
| K | 3.8 |
| Ca | 8.4 |
| Mg | 2.2 |
| BUN | 6.6 |
| Cr | 0.7 |
| VBG | |
| pH | 7.41 |
| HCO3 | 20 |
| PCo2 | 24 |
| BE | -4 |
| AST | 45 |
| ALT | 15 |
| ESR | 58 |
| CRP | 120 |
| First LDH | 1310 |
| Second LDH | 800 |
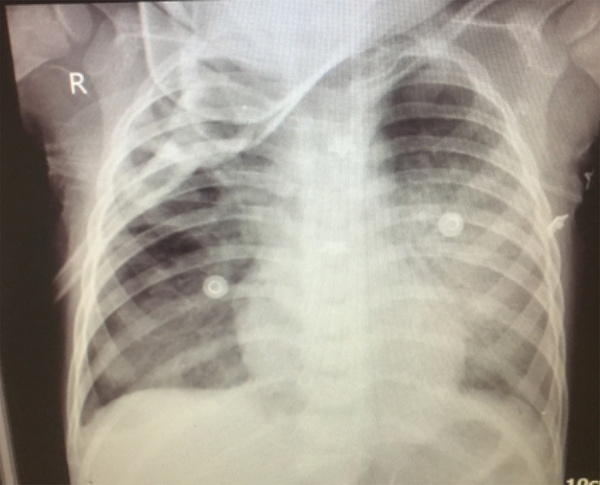
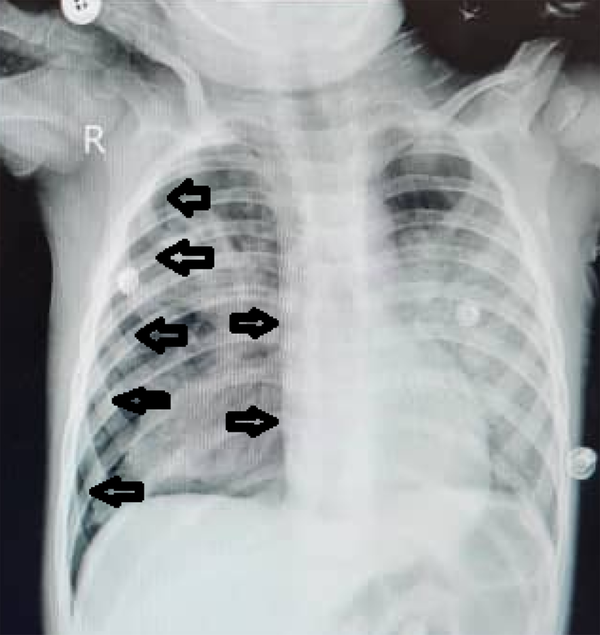
First, chest X-ray showed infiltration in both lungs with haziness and ground glass appearance (Figure 1). During hospitalization, the patient experienced a sudden drop in O2sat (87%), and his respiratory distress intensified. Venous blood gases (VBGs) were pH = 7.27, HCO3 = 23.8 (22 - 28 mEq/L), PCO2 = 41 (38 - 42mmHg), and BE = -0.7 (-5 - +3) and the patient underwent oxygen mask reservation. Re-imaging showed spontaneous pneumothorax and mediastinal shift (Figure 2). Due to the patient's stable condition, the decision was conservative treatment, and chest tube was not inserted. Due to 90% O2sat and its gradual increase with oxygen through the reserve mask, we closely monitored him while receiving oxygen and repeated serial graphs and VBGs. Because the patient was undergoing prophylaxis and treatment with anti-PJP (pneumocystis jiroveci), PJP was not considered due to the COVID-19 epidemic and the patient’s X-ray. Pneumothorax is also commonly reported in COVID-19.
First chest X-ray
Second chest X-ray with pneumothorax and mediastinal shift
Finally, the patient's spontaneous pneumothorax improved (Figure 3) with supportive care over the course of a week, and the patient was discharged in good general condition after completion of the antibiotic course and cessation of fever.
Third chest X-ray shows re-expansion of the lungs

3. Discussion
We report the case of spontaneous pneumothorax in an immunocompromised patient (hyper IgM syndrome) with COVID-19 that improved with supportive care. COVID-19 is a serious and widespread global infection that has spread to numerous countries, including Iran. Pneumothorax rarely occurs in cases of COVID-19 due to damage to the lungs and parenchymal alveoli, which may increase mortality (6). The proposed mechanism of spontaneous pneumothorax in patients with COVID-19 disease is thought to be related to the structural changes occurring in the lung parenchyma. These include cystic and fibrotic changes leading to alveolar tears. In addition, the increase in intrathoracic pressure can result in prolonged coughing and/or mechanical ventilation (7). In the case of a persistent cough, sudden increase in intra-alveolar pressure occurs, and in the event of a ruptured alveoli, it may result in pneumothorax (8). As pneumothorax does not occur only in patients on positive pressure ventilation and barotrauma cannot be the sole mechanism, direct invasion of virus and tissue damage is an important cause. (9). Cystic lung changes secondary to COVID-19 infection is another mechanism leading to spontaneous pneumothorax. (4)
The known risk factors for spontaneous pneumothorax include male gender, smoking, trauma, age group 10 - 30 years, infection, respiratory distress syndrome (ARDS), and mechanical ventilation (10). Pediatric reports of COVID-19 infection and pneumothorax are rare. In a case series report from Cambridge, 2% of 46 cases with spontaneous pneumothorax due to COVID-19 were under 30 years, with a mortality rate of 67% (11) . Hyper IgM syndrome and COVID-19 infection accompanied by spontaneous pneumothorax have not been reported in the literature. However, the case of an 18 years old male with tension pneumothorax and hyper IgM syndrome with pneumocystis Jiroveci pneumonia was reported by Tsai et al. in 2015 (Taiwan) (12).
A multicenter study in the USA (2020) reported six cases of spontaneous pneumothorax, four of whom underwent mechanical ventilation, and five expired. Chest tube insertion was used in all of them (4).
Since conservative management with oxygen through the reserve mask was done successfully in our patient, this modality can be an optional treatment. Lack of experience in the management of spontaneous pneumothorax in COVID-19 patients results in individual decision in their management. Spontaneous pneumothorax in COVID-19 infection is a rare, immediate, but treatable complication and may occur days to weeks after the resolution of the obvious symptoms of COVID-19. Physicians should consider spontaneous pneumothorax in patients with acute shortness of breath and chest pain, especially if they have a recent history of COVID-19 pneumonia. In addition, some studies have suggested that patients may be at risk for pneumothorax even weeks after recovery from COVID-19 infection. However, more research is warranted (10). The best approach to this complication seems to be selecting less invasive ways such as oxygen through the reserve mask if applicable.
3.1. Conclusions
The severity and prognosis of spontaneous pneumothorax in COVID-19 infection, especially in children, is not yet known. It is recommended that conservative treatment be performed if the patient has stable vital signs and no severe respiratory failure. However, this requires more detailed clinical evaluations.
References
-
1.
Spiro JE, Sisovic S, Ockert B, Bocker W, Siebenburger G. Secondary tension pneumothorax in a COVID-19 pneumonia patient: a case report. Infection. 2020;48(6):941-4. [PubMed ID: 32557347]. [PubMed Central ID: PMC7301769]. https://doi.org/10.1007/s15010-020-01457-w.
-
2.
Alhakeem A, Khan MM, Al Soub H, Yousaf Z. Case report: COVID-19-associated bilateral spontaneous pneumothorax-A literature review. Am J Trop Med Hyg. 2020;103(3):1162-5. [PubMed ID: 32666917]. [PubMed Central ID: PMC7470558]. https://doi.org/10.4269/ajtmh.20-0680.
-
3.
Yang F, Shi S, Zhu J, Shi J, Dai K, Chen X. Analysis of 92 deceased patients with COVID-19. J Med Virol. 2020;92(11):2511-5. [PubMed ID: 32293741]. [PubMed Central ID: PMC7262332]. https://doi.org/10.1002/jmv.25891.
-
4.
Zantah M, Dominguez Castillo E, Townsend R, Dikengil F, Criner GJ. Pneumothorax in COVID-19 disease- incidence and clinical characteristics. Respir Res. 2020;21(1):236. [PubMed ID: 32938445]. [PubMed Central ID: PMC7492794]. https://doi.org/10.1186/s12931-020-01504-y.
-
5.
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 2020;295(3):715-21. [PubMed ID: 32053470]. [PubMed Central ID: PMC7233367]. https://doi.org/10.1148/radiol.2020200370.
-
6.
Fahad AM, Mohammad AA, Al-Khalidi HA, Alshewered AS. Spontaneous pneumothorax as a complication in COVID-19 male patient: A case report. Clin Case Rep. 2020. [PubMed ID: 33042545]. [PubMed Central ID: PMC7537536]. https://doi.org/10.1002/ccr3.3378.
-
7.
Zhou C, Gao C, Xie Y, Xu M. COVID-19 with spontaneous pneumomediastinum. Lancet Infect Dis. 2020;20(4). https://doi.org/10.1016/s1473-3099(20)30156-0.
-
8.
Fan Q, Pan F, Yang L. Spontaneous pneumothorax and subpleural bullae in a patient with COVID-19: a 92-day observation. Eur J Cardiothorac Surg. 2020;58(4):858-60. [PubMed ID: 32951046]. [PubMed Central ID: PMC7543338]. https://doi.org/10.1093/ejcts/ezaa305.
-
9.
Liu K, Zeng Y, Xie P, Ye X, Xu G, Liu J, et al. COVID-19 with cystic features on computed tomography: A case report. Medicine (Baltimore). 2020;99(18). e20175. [PubMed ID: 32358406]. [PubMed Central ID: PMC7440163]. https://doi.org/10.1097/MD.0000000000020175.
-
10.
Dennison J, Carlson S, Faehling S, Lieb M, Mubarik A. Case report: Spontaneous pneumothorax in resolved, uncomplicated COVID-19 Pneumonia-A literature review. Respir Med Case Rep. 2020;31:101291. [PubMed ID: 33200068]. [PubMed Central ID: PMC7658556]. https://doi.org/10.1016/j.rmcr.2020.101291.
-
11.
Martinelli AW, Ingle T, Newman J, Nadeem I, Jackson K, Lane ND, et al. COVID-19 and pneumothorax: a multicentre retrospective case series. Eur Respir J. 2020;56(5). [PubMed ID: 32907891]. [PubMed Central ID: PMC7487269]. https://doi.org/10.1183/13993003.02697-2020.
-
12.
Tsai HY, Yu HH, Chien YH, Chu KH, Lau YL, Lee JH, et al. X-linked hyper-IgM syndrome with CD40LG mutation: two case reports and literature review in Taiwanese patients. J Microbiol Immunol Infect. 2015;48(1):113-8. [PubMed ID: 23010537]. https://doi.org/10.1016/j.jmii.2012.07.004.

