Abstract
Introduction:
Spontaneous spinal epidural hematoma (SSEH) is an uncommon but potentially fatal condition. The increased bleeding tendency associated with anticoagulant medications has been proven to increase the risk of SSEH. The symptoms of SSEH usually begin with sudden severe neck or back pain and are followed by neurological deficits. However, some cases present with only axial pain or with radicular pain similar to herniated disc disorders.Case Presentation:
A 28-year-old healthy man developed a sudden onset of severe neck and right shoulder pain with mild arm weakness. The MRI revealed an SSEH that was compressing his spinal cord in the right posterolateral epidural space from C2-C6. On the second hospital day, his symptoms suddenly improved, and most of the hematoma had spontaneously resolved.Conclusions:
Currently, the incidence of SSEH is expected to increase. Pain physicians must include SSEH in their differential diagnosis for patients with axial pain or radicular symptoms alone, particularly when risk factors are present.Keywords
1. Introduction
Spontaneous spinal epidural hematoma (SSEH) is a rare, spinal epidural space-occupying lesion. The initial presentation of SSEH is varied widely from only axial neck or back pain to severe neurological compromise (1). The diagnosis could be delayed for patients who report axial spinal pain alone or minimal neurological deficits compared with those patients with definite motor or sensory abnormalities. Traditionally, emergent decompressive surgery was considered in these cases because the progression of spinal compromise can lead to catastrophic neurologic deficits or even death (2). As SSEHs run a benign course more often than previously estimated, the choice of treatment should be decided for each case individually.
To remind the pain physician to keep this condition in mind when making a diagnosis, we report a cervical SSEH case that showed minimal neurological deficits and a benign course.
2. Case Presentation
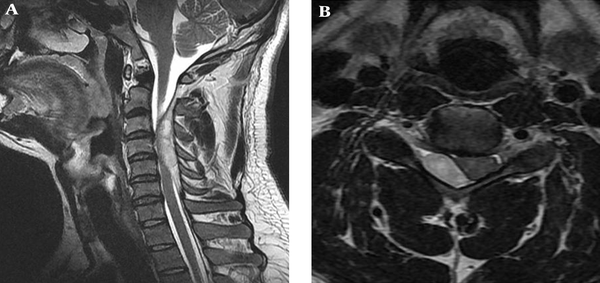
A 28-year-old healthy man developed severe neck and right shoulder pain of a sudden onset while he was getting out of a car. He was admitted to a local hospital where a cervical magnetic resonance imaging (MRI) study was performed. The MRI demonstrated a large epidural mass compressing the spinal cord on the right posterolateral side from C2-C6 (Figure 1). The lesion was isointense to the spinal cord on T1-weighted images, hyperintense on T2-weighted images, and exhibited no contrast enhancement.
Initial T2-weighted sagittal (A) and axial (B) magnetic resonance images showed a hyperintense acute hematoma compressing the spinal cord in the right dorsal epidural space at the C2-C6 level.
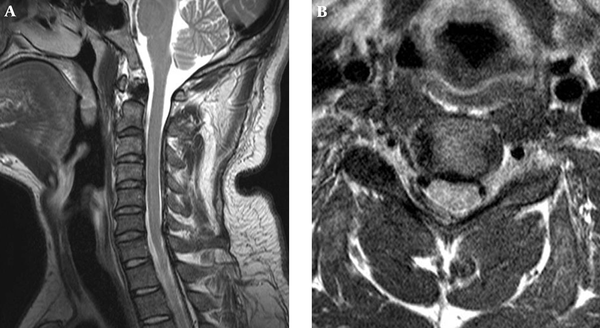
He was referred to our institution two days after the onset of his symptoms. At that time, his neck and shoulder pain were somewhat improved. The patient denied a recent history of trauma or systemic illness. Upon physical examination, a mild biceps weakness in his right arm was identified. The deep tendon reflex of the biceps muscle was increased, and Hoffman’s sign was positive. Laboratory investigations revealed a complete blood cell count, prothrombin time, and partial thromboplastin time within normal limits. A clinical diagnosis of SSEH in the cervical spine was made, and elective surgery was scheduled due to the patient’s minimal neurological deficits. On the second hospital day, his neck and shoulder pain were much improved. The follow-up MRI showed that most of the hematoma had disappeared (Figure 2). The patient was discharged three days after admission, and his right arm weakness improved thereafter. A follow-up MRI obtained four months after the onset of symptoms revealed that the hematoma had completely disappeared.
T2-weighted sagittal (A) and axial (B) magnetic resonance images obtained three days after onset demonstrated the resolution of the hematoma.
3. Discussion
Two decades ago, the annual incidence of SSEH was estimated to be 0.1 patients per 100,000 (3). Recently, the prevalance of SSEH may be on the rise because the number of patients currently taking single or various combinations of antiplatelet and anticoagulant medications is increasing due to the frequent occurrence of heart or cerebrovascular disease. In addition, the application of MRI in daily medical practice even for patients with minimal neurological abnormalities is easier than in the past; MRI has greatly facilitated the diagnosis of SSEH, allowing for the detection of more cases with a benign, natural course. SSEH of idiopathic origin is most frequently observed and accounts for 40% - 50% of spinal epidural hematomas (4). Other secondary causes, such as an increased bleeding tendency for various medications (5), blood dyscracia (6), direct or indirect spinal trauma (7), hypertension (8), and pregnancy (9), have been discussed in the literature.
Most reviews that have been conducted to determine the pathophysiologic mechanism in this process have indicated venous bleeding as the most likely source of hemorrhage due to the structural characteristics of the posterior internal vertebral venous plexus and the positional predominance of SSEH cases, especially in the cervicothoracic and thoracolumbar areas (10-12).
The clinical presentation of SSEH is variable. The symptoms usually start with sudden, severe neck or back pain and followed by motor or sensory deficits around and below the corresponding dermatomes related to compression of nerve roots and the spinal cord. Some cases present only with axial pain or with radicular pain, similar to herniated disc disease. Various time intervals were found between the onset of axial pain and the development of neurological deficits. Sometimes, the axial pain resolved spontaneously without producing any neurological deficits (13).
MRI is the study of choice not only for its definitive diagnosis but also to rule out the presence of SSEH. SSEH should be certainly doubted and an immediate spinal MRI must be ordered if a patient presents with definite neurological deficits in the early phase of the disease progression. However, the diagnosis could be difficult and therefore be delayed for patients with only axial spinal pain or minimal neurological deficits similar to herniated disc disease.
Major reviews for the outcomes of SSEH have indicated that less severe preoperative neurological deficits and a shorter time to surgical evacuation from the onset of symptoms were closely linked to more favorable recovery (14). Therefore, early surgical decompression that takes place before the condition proceeds to serious spinal compromise is regarded as the standard of management. However, the number of reported cases of SSEH treated conservatively has recently increased. Conservative care has been applied in patients who showed evidence of spontaneous neurological improvement and subsequent hematoma disappearance in follow-up imaging in the early phase of the disease (15). Furthermore, non-operative treatment was extended to patients with minimal neurological deficits (13), and the repeated assessment of neurological deterioration was emphasized (16). The spontaneous resolution of SSEH usually began several hours to days after onset; spreading of the hematoma along the spinal epidural space was suggested as one plausible explanation (13, 17). This condition was found irrespective of the causative mechanisms (i.e., hemophilia (18), anticoagulant medication (19), and trauma (20)).
We report a case of cervical SSEH with minimal neurological symptoms that spontaneously resolved. Currently, it is expected that pain physicians will have more opportunities to see these potentially fatal diseases in the pain clinic. A detailed history-taking and spinal MRI study should be provided for all patients with isolated axial pain or radicular symptoms. An epidural steroid block should be avoided in patients with sudden, unexplained axial spinal pain, even though minimal neurological deficits may be overlooked without a proper evaluation. Consequently, pain physicians must include SSEH in their differential diagnosis for patients suffering with axial pain or radicular symptoms alone, particularly when risk factors are also present.
References
-
1.
Matsumura A, Namikawa T, Hashimoto R, Okamoto T, Yanagida I, Hoshi M, et al. Clinical management for spontaneous spinal epidural hematoma: diagnosis and treatment. Spine J. 2008;8(3):534-7. [PubMed ID: 17434807]. https://doi.org/10.1016/j.spinee.2007.01.009.
-
2.
Saritas A, Guneysu F, Guneysu S, Buyukkaya R, Kandis H. An unusual presentation of spontaneous spinal epidural hematoma. J Emerg Med. 2014;47(6):689-91. [PubMed ID: 25256411]. https://doi.org/10.1016/j.jemermed.2014.06.048.
-
3.
Holtas S, Heiling M, Lonntoft M. Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology. 1996;199(2):409-13. [PubMed ID: 8668786]. https://doi.org/10.1148/radiology.199.2.8668786.
-
4.
Penar PL, Fischer DK, Goodrich I, Bloomgarden GM, Robinson F. Spontaneous spinal epidural hematoma. Int Surg. 1987;72(4):218-21. [PubMed ID: 3448033].
-
5.
Moon HJ, Kim JH, Kim JH, Kwon TH, Chung HS, Park YK. Spontaneous spinal epidural hematoma: an urgent complication of adding clopidogrel to aspirin therapy. J Neurol Sci. 2009;285(1-2):254-6. [PubMed ID: 19635624]. https://doi.org/10.1016/j.jns.2009.06.028.
-
6.
Arishima H, Tada A, Isozaki M, Kitai R, Kodera T, Kikuta K, et al. Spontaneous spinal epidural hematoma in a patient with acquired Factor X deficiency secondary to systemic amyloid light-chain amyloidosis. J Spinal Cord Med. 2015;38(5):641-4. [PubMed ID: 24974738]. https://doi.org/10.1179/2045772314Y.0000000230.
-
7.
Lefranc F, David P, Brotchi J, De Witte O. Traumatic epidural hematoma of the cervical spine: magnetic resonance imaging diagnosis and spontaneous resolution: case report. Neurosurgery. 1999;44(2):408-10. discussion 410-1. [PubMed ID: 9932898].
-
8.
Spengos K, Tsivgoulis G, Zakopoulos N. Could high blood pressure be the cause of acute spontaneous spinal epidural hematoma? Eur J Emerg Med. 2007;14(1):59. [PubMed ID: 17198332]. https://doi.org/10.1097/01.mej.0000224434.82117.47.
-
9.
Tada S, Yasue A, Nishizawa H, Sekiya T, Hirota Y, Udagawa Y. Spontaneous spinal epidural hematoma during pregnancy: three case reports. J Obstet Gynaecol Res. 2011;37(11):1734-8. [PubMed ID: 21790886]. https://doi.org/10.1111/j.1447-0756.2011.01592.x.
-
10.
Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004;146(2):103-10. [PubMed ID: 14963742]. https://doi.org/10.1007/s00701-003-0160-9.
-
11.
Kim T, Lee CH, Hyun SJ, Yoon SH, Kim KJ, Kim HJ. Clinical Outcomes of Spontaneous Spinal Epidural Hematoma : A Comparative Study between Conservative and Surgical Treatment. J Korean Neurosurg Soc. 2012;52(6):523-7. [PubMed ID: 23346323]. https://doi.org/10.3340/jkns.2012.52.6.523.
-
12.
Fedor M, Kim ES, Ding K, Muizelaar JP, Kim KD. Spontaneous Spinal Epidural Hematoma: A Retrospective Study on Prognostic Factors and Review of the Literature. Korean J Spine. 2011;8(4):272-82. [PubMed ID: 26064145]. https://doi.org/10.14245/kjs.2011.8.4.272.
-
13.
Serizawa Y, Ohshiro K, Tanaka K, Tamaki S, Matsuura K, Uchihara T. Spontaneous resolution of an acute spontaneous spinal epidural hematoma without neurological deficits. Intern Med. 1995;34(10):992-4. [PubMed ID: 8563102].
-
14.
Groen RJ, Van Alphen HA. Operative treatment of spontaneous spinal epidural hematomas: a study of the factors determining postoperative outcome. Neurosurgery. 1996;39(3):494-508.
-
15.
Kingery WS, Seibel M, Date ES, Marks MP. The natural resolution of a lumbar spontaneous epidural hematoma and associated radiculopathy. Spine (Phila Pa 1976). 1994;19(1):67-9. [PubMed ID: 8153808].
-
16.
Aoki Y, Yamagata M, Shimizu K, Ikeda Y, Nakajima F, Ohtori S, et al. An unusually rapid spontaneous recovery in a patient with spinal epidural hematoma. J Emerg Med. 2012;43(2):75-9. [PubMed ID: 19892504]. https://doi.org/10.1016/j.jemermed.2009.08.031.
-
17.
Hentschel SJ, Woolfenden AR, Fairholm DJ. Resolution of spontaneous spinal epidural hematoma without surgery: report of two cases. Spine (Phila Pa 1976). 2001;26(22):E525-7. [PubMed ID: 11707724].
-
18.
Noth I, Hutter JJ, Meltzer PS, Damiano ML, Carter LP. Spinal epidural hematoma in a hemophilic infant. Am J Pediatr Hematol Oncol. 1993;15(1):131-4. [PubMed ID: 8447556].
-
19.
Wagner S, Forsting M, Hacke W. Spontaneous resolution of a large spinal epidural hematoma: case report. Neurosurgery. 1996;38(4):816-8. [PubMed ID: 8692404].
-
20.
Kim IY, Kim SH, Kim JH, Lee JK. Rapid spontaneous resolution of a traumatic cervical epidural haematoma. Br J Neurosurg. 2005;19(5):451-2. [PubMed ID: 16455573]. https://doi.org/10.1080/02688690500390524.