Abstract
Background:
Chest radiography after central venous catheter (CVC) insertion is the main method of verifying the catheter location. Despite the widespread use of radiography for detecting catheter position, x-ray may not always be readily available, especially in the operating room.Objectives:
We aimed to compare contrast-enhanced ultrasonography (CEUS) and chest radiography for detecting the correct location of CVCs.Methods:
One hundred sixteen consecutive patients with indications for CVC before cardiac surgery were enrolled in this observational study. After catheter insertion, CEUS was performed. Portable radiography was obtained postoperatively in the intensive care unit. Sensitivity, specificity, and predictive values were determined by comparing the ultrasonography results with radiographic findings as a reference standard.Results:
Chest radiography revealed 16 CVC misplacements: two cases of intravascular and 14 cases of right atrium (RA) misplacement. CEUS detected 11 true catheter malpositionings in the RA, while it could not recognize seven catheter placements correctly. CEUS showed two false RA misplacements and five falsely correct CVC positions. A sensitivity of 98% and specificity of 69% were achieved for CEUS in detecting CVC misplacements. Positive and negative predictive values were 95% and 85%, respectively. The interrater agreement (kappa) between CEUS and radiography was 0.72 (P < 0.001).Conclusions:
Despite close concordance between ultrasonography and chest radiography, CEUS is not a suitable alternative for standard chest radiography in detecting CVC location; however, considering its high sensitivity and acceptable specificity in our study, its usefulness as a triage method for detecting CVC location on a real-time basis in the operating room cannot be ignored.Keywords
Catheterization Central Venous Ultrasonography Interventional Radiography Thoracic
1. Background
Central venous catheter (CVC) placement is a common procedure during various major surgeries and in the intensive care unit (ICU). A complication rate of > 15% has been reported following CVC insertion (1, 2), with complications including catheter misplacement, pneumothorax, arterial puncture, and hematoma (3-9). Since the consequences of catheter misplacement could be hazardous and sometimes lethal to the patient (10, 11), detecting the catheter position is highly important. Post-procedure chest radiography is the main method of verifying catheter location. Despite the widespread use of this method, it is time-consuming and it exposes patients to high levels of radiation (12-14). In addition, the feasibility of immediate post-procedure radiography is controversial. Catheterization during major surgeries is usually performed without radiologic confirmation of the catheter position. In this situation, chest radiography is usually performed postoperatively in the ICU, and the time delay could be harmful to patients. In recent years, some researchers have proposed real-time assessment of catheter location using various ultrasound techniques as an alternative to chest radiography (12-19).
2. Objectives
In the present study, we compared contrast-enhanced ultrasonography (CEUS) with chest radiography to evaluate CVC position.
3. Methods
This double-blind study was conducted on 116 consecutive patients. Based on previous studies and considering a sensitivity of 96%, specificity of 93%, a likelihood ratio of 13, and an α value of 5%, with a confidence interval of 95% using the LR formula, we calculated that the study should include at least 76 patients. The patients were referred to Nemazee hospital, affiliated with Shiraz University of Medical Sciences, from August 2013 to January 2014, with indications for elective cardiac surgery and CVC placement.
The exclusion criteria were age under 18 years, recent abdominal and/or chest surgery, and CVC placement in an emergency situation. Written informed consent was obtained from all patients. The study was approved by the ethics committee of Shiraz University of Medical Sciences.
Under general anesthesia, a triple-lumen 7F, 15- or 20-cm CVC (Arrow International, Inc.) was placed using anatomical landmarks with the Seldinger technique. No sonographic guidance was used during the catheter placement. The insertion approach was chosen based on the anesthesiologist’s preference.
After catheter insertion by an anesthesiology resident, CEUS was performed by another anesthesiology resident who had undergone two days of theory-based teaching sessions on cardiac-focused ultrasonography with an expert cardiologist, with an emphasis on the subxyphoid view. The resident was also trained by an expert radiologist to perform Doppler ultrasonography of the carotid and axilla to detect extrathoracic catheter misplacement. Finally, the resident performed 150 CEUS procedures before the start of the study.
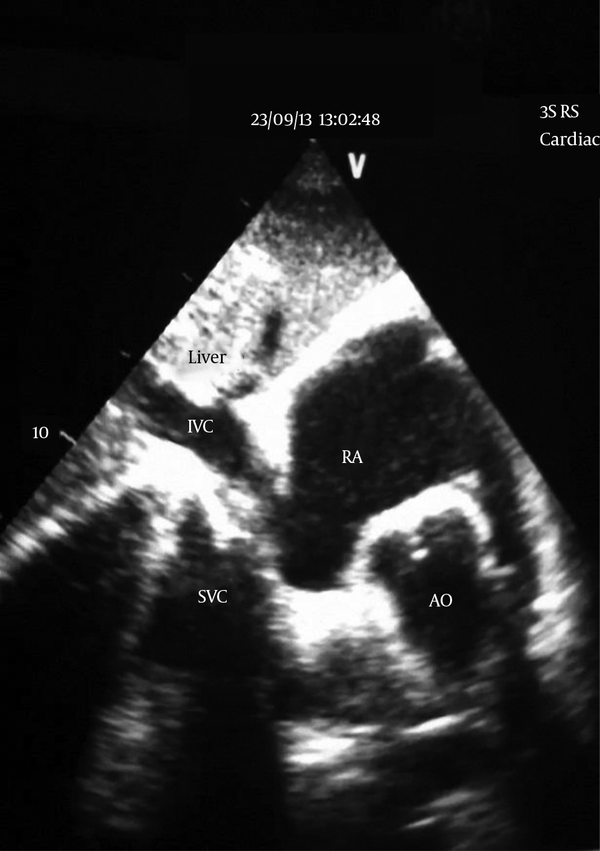
Ultrasound examination was performed through epigastric and subcostal acoustic windows along the short heart axis using a 3S-RS, 1.5 - 3.6 MHZ probe (GE vivid S5 cardiovascular ultrasound machine, USA), which made possible the simultaneous visualization of the superior vena cava (SVC), inferior vena cava (IVC), and right atrium (RA) (Figure 1). To detect catheter position by CEUS, we used the standard technique applied by cardiologists for the diagnosis of a patent foramen ovale (12).
Acceptable View from Subcostal Acoustic Window Before Injection of Contrast
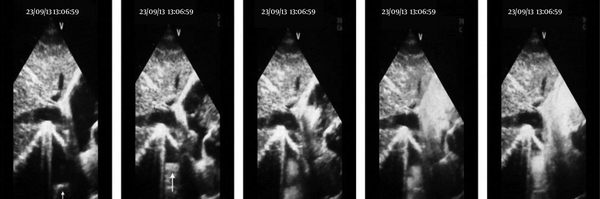
Two 10-mL syringes, one containing 9 mL of saline and the other containing 1 mL of air, were connected to a 3-way stopcock. The saline and air were mixed through the stopcock until a homogenous mixture of air and saline was achieved. The stopcock was attached to the lumen of the catheter, ending at its tip. Next, 5 mL of the solution was injected rapidly through the catheter. Interpretation of the microbubble test was performed using the criteria described by Vezzani and colleagues (Table 1) (12). A stream of microbubbles with laminar jet flow from the SVC within 1 - 2 seconds after the injection indicated correct catheter location (Figure 2). Incorrect placement was defined as turbulent flow coming from the RA or the IVC. The second injection was done only if the catheter location was not confirmed with certainty. If no bubbles were seen, Doppler sonography of the axillary and jugular veins was performed to assess misplacements in these locations, and if the catheter was not seen in these locations, evaluation of the catheter site with fluoroscopic guidance before the start of surgery was planned.
Criteria Described by Vezzani et al. for Classification and Interpretation of Microbubble Test (12)
| Characteristic | Interpretation |
|---|---|
| No bubbles | Negative test: an aberrant or too-distal tip position must be considered. |
| Few bubbles or appearance time > 2 sec | Test to be repeated: if confirmed, possible misplacement (probably in SV or IJV). |
| Numerous bubbles indistinguishable separately; turbulent flow coming from the atrium within 2 sec | Negative test: intra-atrial positioning. |
| Numerous bubbles indistinguishable separately; linear flow coming from SVC | Positive test: CVC tip correctly placed in the SVC. |
Laminar Jet Flow Coming from SVC Indicates Correct Catheter Location (left to right)
All of the ultrasonography video clips were recorded, but only the clips from suspicious cases were reviewed and evaluated for a microbubble flow pattern. After the operation was completed and the patient was transferred to the ICU, portable anteroposterior chest radiography was performed. The results were reported by an expert radiologist who was blinded to the ultrasonography results. Identification of the catheter in the SVC or SVC–RA junction was considered correct placement. Visualization of the catheter tip in any other position was defined as CVC misplacement.
3.1. Statistical Analysis
Analysis was performed using SPSS 19.00 for Windows (SPSS Inc. IBM Corp., Chicago, IL, USA) and continuous variables were presented as the mean (±SD). Sensitivity, specificity, and predictive values were determined by comparing ultrasonography results with radiographic findings as the reference standard. For calculating concordance between CEUS and CXR, the қ statistic was used. P values of < 0.05 were considered statistically significant.
4. Results
Of the total of 116 patients, acceptable acoustic windows could not be achieved in 12, and analyses were performed on the remaining 104. Coronary artery bypass grafting was the main cardiac procedure with an indication for CVC insertion (n = 93). The patient characteristics are shown in Table 2. The right internal jugular approach (n = 91), left internal jugular approach (n = 2), and right subclavian approach (n = 11) were used for catheter placement. Using the anatomical landmark technique, CVC placement was successful on the first attempt in 90 patients (86.5%).
Characteristics of the 104 Patients and Type of Surgery
| Clinical characteristics | |
|---|---|
| Sex, No. (%) | |
| Male | 62 (60) |
| Female | 42 (40) |
| Age, y | 58.2 (12) |
| Weight, kg | 67.7 (15) |
| Height, cm | 166 (10) |
| BMI, kg/m2 | 25.2 (13) |
| Type of surgery, No. | |
| Aortic web | 1 |
| AVR | 3 |
| CABG | 91 |
| MVR | 8 |
| TVR | 1 |
In 97 of the 104 evaluated patients, there was concordance between chest radiography and CEUS findings (both techniques demonstrated correct placement in 86 patients and both demonstrated misplacement in the remaining 11).
The characteristics of the seven patients in whom there was lack of concordance between radiography and CEUS are shown in Table 3. In two of these seven patients, radiography accurately depicted extra-atrial placement of the catheter, while CEUS was reported to show intra-atrial placement (false negative). In the remaining five patients, radiography indicated intra-atrial placement in three cases and intrathoracic vascular placement in two cases, while CEUS demonstrated them all as correct placements (false positive) (Table 4).
Characteristics of Patients in Whom Ultrasound Could not Detect Catheter Position Correctly
| Patient | Age, y | Type of Surgery | Catheterization Approach | Ultrasound Findings | CXR Findings |
|---|---|---|---|---|---|
| 1 | 58 | MVR | Right IJV | RA | Above SVC-RA junction (correct catheter position) |
| 2 | 68 | CABG | Right IJV | RA | Above SVC-RA junction (correct catheter position) |
| 3 | 58 | CABG | Right IJV | Correct catheter position | RA (misplacement) |
| 4 | 59 | CABG | Subclavian vein | Correct catheter position | Brachiocephalic vein (misplacement) |
| 5 | 50 | CABG | Right IJV | Correct catheter position | RA (misplacement) |
| 6 | 53 | CABG | Left IJV | Correct catheter position | Right subclavian vein (misplacement) |
| 7 | 57 | CABG | Right IJV | Correct catheter position | RA (misplacement) |
Comparison Between CEUS and Radiography in Detecting Correct Catheter Placement
| CEUS | Radiography | ||
|---|---|---|---|
| Correct Placement | Misplacement | Sum | |
| Correct placement | 86 | 5 | 91 |
| Misplacement | 2 | 11 | 13 |
| Sum | 88 | 16 | 104 |
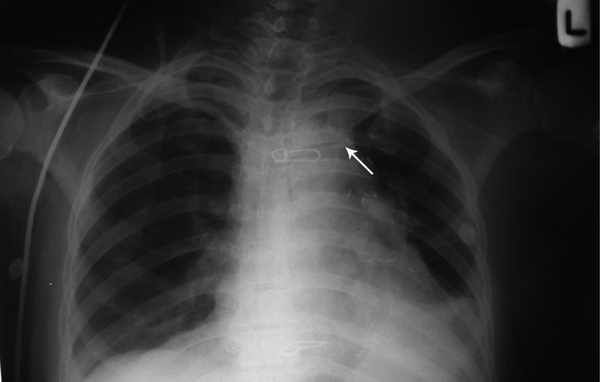
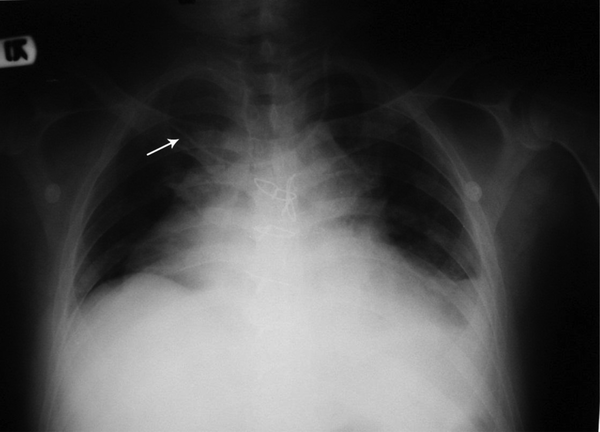
Chest radiography revealed aberrant catheter position in 16 patients: two cases of intravascular and 14 cases of RA misplacement. One of the intravascular misplacements was in the brachiocephalic vein through a right subclavian approach (Figure 3), and one was in the right subclavian vein through a left internal jugular approach (Figure 4).
Central venous catheter is inserted through a right subclavian approach. Misplacement can be seen in the brachiocephalic vein.
Central venous catheter inserted through a left internal jugular approach. Arrow shows the tip of the catheter in the right subclavian vein.
On the ultrasound examinations, the flow of microbubbles was seen in all 104 patients. CEUS detected 11 true catheter malpositions in the RA, while it was not able to recognize seven catheter placements correctly (Table 3). No intravascular misplacement was identified with CEUS. Considering chest radiography as a reference standard, a sensitivity of 98% and specificity of 69% were achieved for CEUS in detecting CVC misplacements. Positive and negative predictive values were 95% and 85%, respectively. Interrater agreement (kappa) between CEUS and CXR was 0.72 (P < 0.001).
5. Discussion
We found that CEUS could accurately detect approximately 70% of catheter misplacements in the operating room in real time. Routine chest radiography after CVC insertion has been considered the gold standard for detecting catheter location; however, this is usually done after the patient is transferred to the ICU. The presence of various radiographic landmarks allows the radiologist to ensure the correct positioning of catheter tips (11, 20-23). According to our findings, detecting catheter misplacement in a real-time fashion can prevent related possible complications in at least two thirds of patients.
In recent years, some studies have investigated the potential of ultrasonography as an alternative to radiography in the detection of catheter positioning and other complications after CVC placement. Some of these studies described ultrasonography as an accurate method for identifying catheter location and avoiding life-threatening complications, such as pneumothorax (12-15, 17-19). Maury and colleagues reported a high success rate of ultrasonic evaluation in detecting aberrant catheter location and pneumothorax (14). Vezzani and colleagues compared chest radiography with a combination of B-mode ultrasonography and CEUS. In their study, some cases (n = 6) could not be detected with B-mode ultrasonography alone, while additional evaluations with CEUS could reveal the undetected cases. They argued that this combined method could be an accurate alternative to radiography. Although the performance of ultrasonography by an experienced physician in their study could increase the sensitivity and specificity of their technique and increase the general feasibility of ultrasonography, their study differs from ours because we only used CEUS for catheter location and could not achieve sufficiently high specificity and sensitivity to recommend similar accuracy between radiography and ultrasonography. Vezzani and colleagues also did not have brachiocephalic vein or SVC misplacements, so we cannot say that they could have found them (12).
Zanobetti and colleagues considered correct catheter position at the level of the SVC based on the absence of an echogenic CVC tip within the heart chambers or the internal jugular or subclavian veins (13). They found a high concordance between chest radiography and ultrasonography, but it should be noted that they could not visualize the catheter tip directly in 45% of the cases, and those cases were considered as correct catheter positioning. Due to the limitations of ultrasonography in obtaining a direct view of the catheter tip in the thoracic cavity, the lack of direct visualization of the catheter tip in the defined positions does not necessarily indicate correct CVC placement.
Lanza and colleagues also reported close concordance between B-mode and color Doppler sonography and radiography in evaluating the catheter tip (15). They recommended radiography only for suspected cases. Considering the population of their study, who were mostly children, their findings are different from ours, which were derived from an adult population. Other researchers also reported more favorable efficacy of CEUS in children (16).
Our results are in accordance with Cortellaro and co-workers, who reported that CEUS could not substitute for chest radiography; however, their reported sensitivity (33%) was lower than ours (98%) and their reported specificity (98%) was higher than ours (69%) (16). Their low reported sensitivity led them to not recommend CEUS as a triage test. However, due to the sensitivity we obtained, we believe that CEUS may detect at least 69% of malpositionings. Therefore, using it for triage in the operating room seems logical, although it cannot replace radiography as the gold standard.
One of the limitations of our study was that we could not achieve an acceptable acoustic window in 12 cases due to technical limitations. Pneumothorax, another complication of CVC placement, could not be evaluated because thoracotomies were performed in our sample and postoperative CXR could not demonstrate pneumothorax as a CVC complication. Measurement of time was another limitation of our study; CXR was done in the ICU a few hours after CVC insertion, so a comparison of the time required to perform CEUS versus CXR was not possible.
5.1. Conclusion
CEUS is not an alternative for standard chest radiography in detecting CVC location; however, considering its high sensitivity and acceptable specificity in our study, its utility as a triage method for detecting CVC location on a real-time basis in the operating room cannot be denied. Although CVC placements still require final confirmation by radiography, which is done in the ICU, the safety and feasibility of using CEUS in cases with suspected CVC malposition makes it worth trying in the operating room. Large non-inferiority studies to confirm similar results are recommended.
Acknowledgements
References
-
1.
Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001;286(6):700-7. [PubMed ID: 11495620].
-
2.
Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331(26):1735-8. [PubMed ID: 7984193]. https://doi.org/10.1056/NEJM199412293312602.
-
3.
Ruesch S, Walder B, Tramer MR. Complications of central venous catheters: internal jugular versus subclavian access--a systematic review. Crit Care Med. 2002;30(2):454-60. [PubMed ID: 11889329].
-
4.
Aminnejad R, Razavi SS, Mohajerani SA, Mahdavi SA. Subclavian Vein Cannulation Success Rate in Neonates and Children. Anesth Pain Med. 2015;5(3):24156. [PubMed ID: 26161322]. https://doi.org/10.5812/aapm.24156v2.
-
5.
Moeinipour AA, Amouzeshi A, Joudi M, Fathi M, Jahanbakhsh S, Hafez S, et al. A rare central venous catheter malposition: a case report. Anesth Pain Med. 2014;4(1):16049. [PubMed ID: 24660160]. https://doi.org/10.5812/aapm.16049.
-
6.
Lie J, Yadagiri M, Aspinall C. Letter to editor on a rare central venous catheter malposition. Anesth Pain Med. 2014;4(4):20019. [PubMed ID: 25337476]. https://doi.org/10.5812/aapm.20019.
-
7.
Fathi M, Izanloo A, Jahanbakhsh S, Taghavi Gilani M, Majidzadeh A, Sabri Benhang A, et al. Central Venous Cannulation of the Internal Jugular Vein Using Ultrasound-Guided and Anatomical Landmark Techniques. Anesth Pain Med. In Press;In Press:35803.
-
8.
Lentz RJ, Sandler KL, Miller AN. Cannulation of the Internal Thoracic Artery with a Central Venous Catheter. Am J Respir Crit Care Med. 2016;193(5):9-11. [PubMed ID: 26652299]. https://doi.org/10.1164/rccm.201509-1748IM.
-
9.
Shah PN, Kane D, Appukutty J. Depth of central venous catheterization by intracardiac electrocardiogram in adults. Anesth Pain Med. 2013;2(3):111-4. [PubMed ID: 24244919]. https://doi.org/10.5812/aapm.7557.
-
10.
Orme RM, McSwiney MM, Chamberlain-Webber RF. Fatal cardiac tamponade as a result of a peripherally inserted central venous catheter: a case report and review of the literature. Br J Anaesth. 2007;99(3):384-8. [PubMed ID: 17611250]. https://doi.org/10.1093/bja/aem181.
-
11.
Collier PE, Blocker SH, Graff DM, Doyle P. Cardiac tamponade from central venous catheters. Am J Surg. 1998;176(2):212-4. [PubMed ID: 9737635].
-
12.
Vezzani A, Brusasco C, Palermo S, Launo C, Mergoni M, Corradi F. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med. 2010;38(2):533-8. [PubMed ID: 19829102]. https://doi.org/10.1097/CCM.0b013e3181c0328f.
-
13.
Zanobetti M, Coppa A, Bulletti F, Piazza S, Nazerian P, Conti A, et al. Verification of correct central venous catheter placement in the emergency department: comparison between ultrasonography and chest radiography. Intern Emerg Med. 2013;8(2):173-80. [PubMed ID: 23242559]. https://doi.org/10.1007/s11739-012-0885-7.
-
14.
Maury E, Guglielminotti J, Alzieu M, Guidet B, Offenstadt G. Ultrasonic examination: an alternative to chest radiography after central venous catheter insertion? Am J Respir Crit Care Med. 2001;164(3):403-5. [PubMed ID: 11500340]. https://doi.org/10.1164/ajrccm.164.3.2009042.
-
15.
Lanza C, Russo M, Fabrizzi G. Central venous cannulation: are routine chest radiographs necessary after B-mode and colour Doppler sonography check? Pediatr Radiol. 2006;36(12):1252-6. [PubMed ID: 17016700]. https://doi.org/10.1007/s00247-006-0307-y.
-
16.
Cortellaro F, Mellace L, Paglia S, Costantino G, Sher S, Coen D. Contrast enhanced ultrasound vs chest x-ray to determine correct central venous catheter position. Am J Emerg Med. 2014;32(1):78-81. [PubMed ID: 24184012]. https://doi.org/10.1016/j.ajem.2013.10.001.
-
17.
Duran-Gehring PE, Guirgis FW, McKee KC, Goggans S, Tran H, Kalynych CJ, et al. The bubble study: ultrasound confirmation of central venous catheter placement. Am J Emerg Med. 2015;33(3):315-9. [PubMed ID: 25550065]. https://doi.org/10.1016/j.ajem.2014.10.010.
-
18.
Weekes AJ, Keller SM, Efune B, Ghali S, Runyon M. Prospective comparison of ultrasound and CXR for confirmation of central vascular catheter placement. Emerg Med J. 2016;33(3):176-80. [PubMed ID: 26446313]. https://doi.org/10.1136/emermed-2015-205000.
-
19.
Saul T, Doctor M, Kaban NL, Avitabile NC, Siadecki SD, Lewiss RE. The Ultrasound-Only Central Venous Catheter Placement and Confirmation Procedure. J Ultrasound Med. 2015;34(7):1301-6. [PubMed ID: 26112635]. https://doi.org/10.7863/ultra.34.7.1301.
-
20.
Aslamy Z, Dewald CL, Heffner JE. MRI of central venous anatomy: implications for central venous catheter insertion. Chest. 1998;114(3):820-6. [PubMed ID: 9743173].
-
21.
Schuster M, Nave H, Piepenbrock S, Pabst R, Panning B. The carina as a landmark in central venous catheter placement. Br J Anaesth. 2000;85(2):192-4. [PubMed ID: 10992822].
-
22.
Yoon SZ, Shin JH, Hahn S, Oh AY, Kim HS, Kim SD, et al. Usefulness of the carina as a radiographic landmark for central venous catheter placement in paediatric patients. Br J Anaesth. 2005;95(4):514-7. [PubMed ID: 16040638]. https://doi.org/10.1093/bja/aei199.
-
23.
Wirsing M, Schummer C, Neumann R, Steenbeck J, Schmidt P, Schummer W. Is traditional reading of the bedside chest radiograph appropriate to detect intraatrial central venous catheter position? Chest. 2008;134(3):527-33. [PubMed ID: 18641117]. https://doi.org/10.1378/chest.07-2687.